Case Report - Journal of Cardiovascular Medicine and Therapeutics (2017) Volume 1, Issue 1
Replacement of clopidogrel with ticagrelor for a patient with polycythemia vera accompanied by repeated myocardial infarction and acute stent thrombosis
- *Corresponding Author:
- Hsin-Fu Lee
Department of Internal Medicine Cardiovascular Intervention Centre Chang Gung Memorial Hospital Linkou, Taiwan
Tel: +886 3 3281200
Fax: +886 3 3271192
E-mail: hsinfu.lee@gmail.com
Accepted date: January 06, 2017
Citation: Lee HF, Wang CL, Chan YH. Replacement of clopidogrel with ticagrelor for a patient with polycythemia vera accompanied by repeated myocardial infarction and acute stent thrombosis. J Cardiovasc Med Ther. 2017;1(1):1-4.
Abstract
A 58-year-old male presented with acute coronary syndrome (ACS) and an abnormal hematologic profile. After further testing and consultation with a haematologist, the patient was diagnosed with Polycythemia vera (PV). Coronary arteries were normal on angiography, and he was treated with dual antiplatelet regimen of Aspirin and Clopidogrel. In less than one month the patient experienced recurrent ACS with ST segment elevation. Primary percutaneous coronary intervention (PCI) was performed, and a coronary stent was implanted. However, the patient developed acute stent thrombosis as a complication. After a second PCI and replacement of Clopidogrel with Ticagrelor, no further cardiac event occurred during his hospitalization. In addition of phlebotomy, hydroxyurea was added to the medication and the patient was kept on a dual antiplatelet regimen of aspirin and ticagrelor for nine months. No cardiac event was noted over the course of a follow-up of more than one year. This is the first report describing successful treatment utilizing ticagrelor in a PV patient with repeated myocardial infarction and acute stent thrombosis.
Keywords
Ticagrelor, Polycythemia vera, Acute coronary syndrome, Stent thrombosis.
Learning Objective
In the literature, PV patients may have an increased risk of stent thrombosis after coronary stent implantation. In this first case in which Clopidogrel was replaced by ticagrelor in the treatment of a patient suffering repeated myocardial infarctions and acute stent thrombosis after stent implantation, ticagrelor may be suitable as an antiplatelet medication in this situation.
Introduction
Polycythemia vera (PV) is a clonal disorder arising in multipotent hematopoietic progenitor cells. It causes the overproduction of red cells and, to a lesser extent, neutrophils and platelets. PV occurs with a slight predominance in men, and the median age of diagnosis is 60 years [1]. Although the association between PV and coronary artery disease is unknown, previous studies have reported coronary events occurring during the course of PV [2].
For patients in whom PV presents with acute myocardial infarction, the treatment includes aggressive phlebotomy, to maintain the haematocrit level below 45%, and medical therapy with aspirin and hydroxyurea [1]. The role of angioplasty and stenting is still uncertain and may be challenged by the development of stent thrombosis [3].
Ticagrelor (Brilinta) is an oral antiplatelet treatment that works by inhibiting platelet activation. It was first approved by the FDA in July 2011 on the basis of data from the PLATO study [4]. This report describes the successful use of ticagrelor in treating a PV patient with repeated myocardial infarction and acute stent thrombosis.
Case Presentation
A 58-year-old male presented to our hospital (Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan) with severe retrosternal compressive chest pain. The pain was radiating to left shoulder and was accompanied by cold sweating. The patient had no history of diabetes mellitus, hypertension, or hypercholesterolemia. He also had no habit of smoking, and there was neither a recent history of drug use nor a family history of premature coronary artery disease.
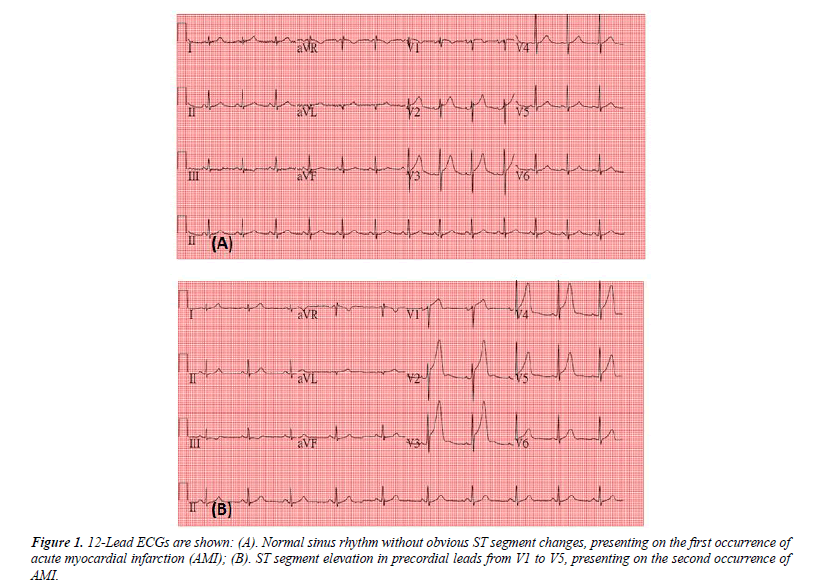
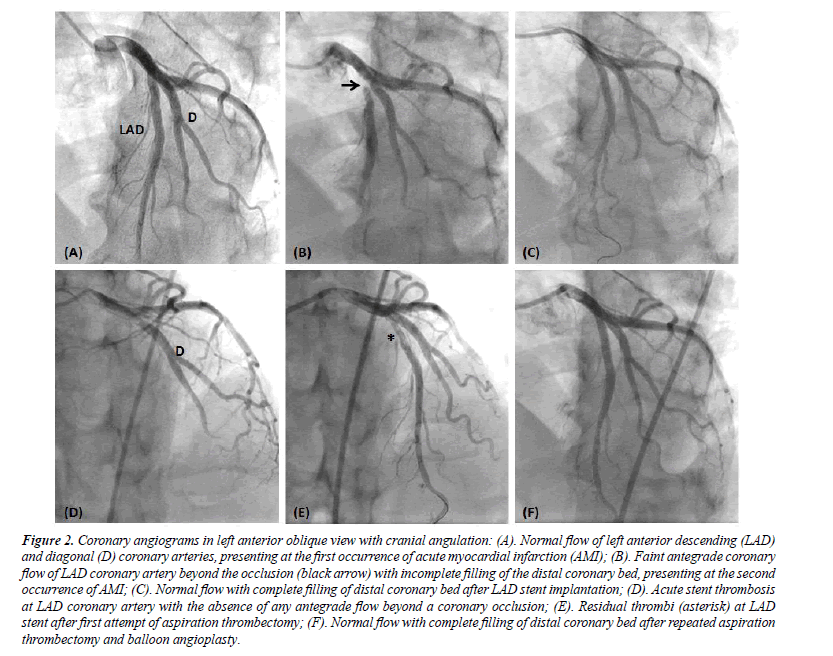
The ECG on admission showed normal sinus rhythm, with no changes indicative of ischemia or infarction (Figure 1A). Laboratory results were as follows (normal range shown in brackets): WBC 19.8 × 103/uL (3.9–10.6 × 103/uL); neutrophils 89.4%; lymphocytes 5.0%; haemoglobin 17.8 g/L (13.5–17.5 g/L); haematocrit 59.2% (41% to 53%); and platelets 401 × 103/ uL (150–400 × 103/uL). The coagulation profile, lipid profile, renal function test, liver function test, and electrolytes were all within normal ranges. The maximum troponin was 7.465 ng/ mL (upper limit of normal is 0.5 ng/mL). Diagnostic coronary angiography revealed no significant stenosis of the coronary arteries (Figure 2A). The patient was discharged five days later with daily medications of aspirin (100 mg), Clopidogrel (75 mg), and bisoprolol (1.25 mg).
Figure 2: Coronary angiograms in left anterior oblique view with cranial angulation: (A). Normal flow of left anterior descending (LAD) and diagonal (D) coronary arteries, presenting at the first occurrence of acute myocardial infarction (AMI); (B). Faint antegrade coronary flow of LAD coronary artery beyond the occlusion (black arrow) with incomplete filling of the distal coronary bed, presenting at the second occurrence of AMI; (C). Normal flow with complete filling of distal coronary bed after LAD stent implantation; (D). Acute stent thrombosis at LAD coronary artery with the absence of any antegrade flow beyond a coronary occlusion; (E). Residual thrombi (asterisk) at LAD stent after first attempt of aspiration thrombectomy; (F). Normal flow with complete filling of distal coronary bed after repeated aspiration thrombectomy and balloon angioplasty.
Additional haematology tests were conducted on an outpatient basis, and further tests were done to exclude potential causes of secondary polycythemia. In addition, the patient was positive for the JAK-2V617F mutation, while a cytogenetic test for the BCR/ABL1 rearrangement was negative.
Within one month the patient again reported similar chest pain. The ECG showed ST segment elevation with precordial leads (Figure 1B). His hematologic profile indicated WBC 18.5 × 103/ uL (3.9–10.6 × 103/uL); neutrophils 85.2%; lymphocytes 8.4%; haemoglobin 18.8 g/L (13.5–17.5 g/L); haematocrit 60.9% (41% to 53%); and platelets 366 × 103/uL (150–400 × 103/uL). In addition, an elevation of 0.562 ng/mL in Troponin I was also noted. Diagnostic coronary angiography showed a faint antegrade coronary flow of the left anterior descending (LAD) coronary artery beyond the occlusion with incomplete filling of the distal coronary bed (Figure 2B). Percutaneous coronary intervention (PCI) was performed with aspiration thrombectomy using a 6 French Medtronic Export XT catheter, with resultant removal of a significant number of thrombi. A 3 mm × 26 mm Resolute Integrity Zotarolimus-eluting stent was implanted in the proximal LAD coronary artery (Figure 2C). A 3.5 mm × 15 mm balloon (Boston Scientific Quantum Maverick balloon) was used to do post-dilatation at 20 atm. Subsequent angiography demonstrated flow improvement to TIMI 3 and excellent results in the treated LAD coronary artery segment. However, around 6 hours after the procedure, the patient again felt chest pain. Acute stent thrombosis was identified by coronary angiography (Figure 2D). Coronary flow was restored after intervention with aspiration thrombectomy and balloon angioplasty (Figures 2E- 2F). The patient was given an immediate loading dose of 150 mg ticagrelor and treated twice daily with 75 mg ticagrelor as a replacement for Clopidogrel. No further cardiac event occurred during the course of the patient’s hospital stay.
Phlebotomy was performed, and hydroxyurea was prescribed to achieve a haematocrit level of around 45% two months following the index of ST elevation myocardial infarction. The patient received dual antiplatelet treatment with aspirin and ticagrelor for nine months, according to the guidelines of Taiwan’s national health insurance. Thereafter he continued with aspirin treatment alone. No evidence of sub-acute or latent stent thrombosis or any other cardiac event was noted over the course of follow-up for more than one year.
Discussion
To the best of our knowledge, this is the first report in which ticagrelor was used to replace Clopidogrel for the treatment of a PV patient with repeated myocardial infarction and acute stent thrombosis following coronary stenting. The cardiovascular outcome was excellent, without recurrent stent thrombosis or myocardial infarction over the course of a more than one-year follow-up.
Acute coronary syndrome (ACS) has been reported to occur in PV patients [2]. Although the pathophysiology of thromboembolic events is not well-known, there are some features of PV which may contribute, including the increased hematocrit and blood viscosity, leukocytosis, thrombocytosis, stimulation of platelet aggregation, and intimal proliferation [5]. In general, antiplatelet therapy and cytoreductive therapy (including phlebotomy, hydroxyurea, or both) have been indicated for the treatment of ACS in PV [5]. However, it is uncertain which type of coronary reperfusion procedure is appropriate for treating ACS in PV patients. For PCI with stent implantation, acute or subacute stent thrombosis has been reported as a serious complication for PV patients [3,6-8]. Fibrinolytic therapy and coronary artery bypass graft (CABG) may be alternatives to PCI. Unfortunately, the effectiveness of fibrinolytic therapy as the sole treatment is unknown. Regarding the risk of postoperative thrombosis with CABG treatment, a previous study showed that even gaining stable control of blood counts in PV patients did not eliminate the risk of postoperative thrombosis [9]. Future studies are needed to determine which intervention is most appropriate in PV patients.
This case report may have some important implications. First, our findings echo previous case reports which in PV patients may have had a higher risk of stent thrombosis after stent implantation [3,6-8]. Second, some reports showed the risk of recurrent thrombosis was avoided by adding warfarin to the antiplatelet regimen with aspirin and Clopidogrel [8]. However, the increased risk of nonfatal and fatal bleeding with the combination of aspirin, Clopidogrel, and warfarin is still a major concern [10]. Ticagrelor, a new antiplatelet agent, is a direct-acting, reversible antagonist of adenosine diphosphate P2Y12 receptors that exhibits greater platelet inhibition, a faster offset of action, and a comparable bleeding risk compared to Clopidogrel [4]. Instead of adding warfarin to the treatment regimen, we used ticagrelor to replace Clopidogrel for the patient and found no recurrent thrombosis or myocardial infarction over the course of a one-year follow-up. Therefore, a dual-antiplatelet regimen with aspirin and ticagrelor may be more appropriate in PV patients after coronary stent implantation compared with the combination of aspirin and Clopidogrel. Further studies are warranted to examine the effectiveness of ticagrelor for the treatment of arterial thrombosis in PV patients, especially in a high risk subset of patients with recurrent thrombosis or stent thrombosis. Furthermore, an exploration of the underlying biological processes may contribute to a better understanding of the pathophysiology of thromboembolic events and promote the development of new strategies for preventive interventions for PV patients.
Conclusion
In conclusion, ticagrelor is a new class of antiplatelet drug that exhibits greater platelet inhibition and a comparable risk of bleeding compared to Clopidogrel. PV patients may have an increased risk of stent thrombosis after coronary stent implantation. In this first case in which Clopidogrel was replaced by ticagrelor in the treatment of a patient suffering repeated myocardial infarctions and acute stent thrombosis after stent implantation, we report the patient experienced no cardiac event over the course of a one-year follow-up.
References
- Tefferi A. Polycythemiavera:A comprehensive review and clinical recommendations. Mayo Clin Proc. 2003;78:174-94.
- Malak S, Labopin M, Saint-Martin C,et al. A French group of familial myeloproliferative disease. Long term follow up of 93 families with myeloproliferative neoplasms: Life expectancy and implications of JAK2V617F in the occurrence of complications. Blood Cells Mol Dis. 2012;49:170-76.
- Goethals P, Evrard S, Dubois C. Recurrent coronary stent thrombosis. ActaCardiol. 2000;55:371-73.
- Wallentin L, Becker RC, Budaj A, et al.Ticagrelor versus Clopidogrel in patients with acute coronary syndromes. N Engl J Med.2009;361:1045-57.
- Gilbert HS. Current management in polycythemiavera.SeminHematol. 2001;38:25-28.
- Inami T, Okabe M, Matsushita M, et al. JAK2 mutation and acute coronary syndrome complicated with stent thrombosis. Heart Vessels 2016;31:1714-16.
- Hvelplund A, Hansen PR. Subacute intracoronary stent thrombosis in a patient with polycythaemia vera. UgeskrLaeger. 2006;168:4104-05.
- Zavalloni D, Marsico F, Milone F, et al. Is conventional anti-platelet therapy for the prevention ofcoronary stent thrombosis always safe? A case report of a patient with polycythemiavera. Ital Heart J. 2004;5:163-66.
- Ruggeri M, Rodeghiero F, Tosetto A, et al. Chronic myeloproliferative diseases working Prognosis. Post-surgery outcomes in patients with polycythemiavera and essential thrombocythemia: A retrospective survey. Blood 2008;111:666-71.
- Hansen ML, Sorensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and Clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010;170:1433-41.