- Biomedical Research (2008) Volume 19, Issue 2
Relationship between paraoxanase activity and lipid levels in ischemic stroke patients
Purnima Dey Sarkar and Sushree S. Rautaray
Department of Biochemistry, M.G.M Medical College, Indore (M.P), India
- *Corresponding Author:
- Sushree .S. Rautaray
Department of Biochemistry
M.G.M Medical College
Indore (M.P)
India
E-mail: sushree_rautaray@yahoo.com; sr.rgpv@gmail.com
Accepted date: May 17 2008
Abstract
Ischemic stroke is the major killer and is the most important cause of morbidity and mortal-ity world wide. The increasing incidence is due to hypertension, stress of life,obesity, lack of exercise and other factors. We attempted to determine an independent association of paraoxanase with ischemic stroke patients. The lipid profile and serum paraoxanase were investigated in 100 ischemic stroke patients and 100 control subjects. A significant increase was observed in the concentration of total cholesterol, triglycerides and low density lipopro-tein in ischemic stroke patients. The activities of paraoxanase (PON) and high density lipo-protein concentration decreased in ischemic stroke patients compared to controls. A paraoxanase was an independent (p<0.001) risk factor for ischemic stroke patients along with lipid profiles. PON activity should be evaluated in all ischemic stroke patients in the absence of traditional risk factors.
Key words
Ischemic stroke, Paraoxanase, Risk factors, Lipoproteins.
Introduction
The term stroke defines rapidly developing clinical symptoms and signs of focal loss of cerebral function lasting for more than 24 hours leading to death with no apparent cause other than vascular origin [1]. The increasing incidence of stroke in Indian patients (>65 years) is possibly due to industrialization, stress of life, less exercise, increasing incidence of smoking, hypertension and other factors.
Paraoxanse [(PON) E.C 3.1.8.3 aryldialkyl phophatase] has been extensively studied in the field of toxicology because it hydrolyses organophosphate compounds used as insecticides and nerve gases. [2,3] PON is synthesized in the liver and in serum is located of high density lipoprotein (HDL). The serum HDL concentration is inversely correlated with atherosclerosis risk [4]. HDL protects against oxidative modification of LDL [5,6] which is believed to be central in the initiation and progression of atherosclerosis. [7] The antioxidant activity of HDL relates to its enzymes primarily PON, but also leci-thin/cholesterol acyl transferase (LCAT) and these can prevent lipid peroxide accumulation on LDL both invitro and in vivo [8]. Some studies have shown that serum PON activity is decreased in disease that are associated with accelerated atherogenesis [9,10]. Many studies [11,12,13,14) have proposed that PON-192 polymorphisms might be a risk factor for atherosclerosis. But some studies have failed to find such a relationship .Therefore the present study was carried out to assess the serum PON activity in ischemic stroke patients compared to controls.
Materials and Methods
The study was case controlled in design. We have selected the patients as they have presented. Patients included in the present study were all admitted to the Intensive Care Unit (ICU) or attending the outpatient department of Medicine of Maharaja Yashvantrao Hospital attached to Mahatma Gandhi Memorial College, Indore (M.P).
The study group consisted of 100 patients with ischemic stroke between 60-75 years of age and they were undergoing admission to hospital and 100 age and sex matched controls were taken with no family history of stroke. Brief clinical history covering the signs and symptoms, past, personal and family history of concerned risk factors were taken. All participants gave written informed consent and this protocol was approved by ethical and research committee of Mahatma Gandhi Memorial Medical College, Indore. Serum cholesterol, HDL-c, LDL-c were determined by CHOD-PAP method (Roche Diagnostics). Serum triglyceride was measured enzymatic GPO-POD method (Roche Diagnostics). Serum PON activity was measured by 5.5mmol/l p-nitrophenyl acetate (Sigma Chemicals) as a substrate, the increase in the absorbance of p-nitrophenol formed at 412nm was measured by using ELICO spectrophotometer [15]. The activity of PON was measured in 20mM/L tris buffer at pH8.0 and which contains 1mM calcium chloride. The generated product of p-nitrophenol was calculated by using molar extinction coefficient of 17000 per mole per cm t pH 8.0.Results are expressed as U/ml. (1U, 1nmol p-nitrophenol formed per minute).
Risk factors for ischemic stroke
Diabetes was diagnosed on the basis of fasting blood glu-cose concentration of >126mg/dl. Systemic hypertension was considered to be present if the patient was taking hypertensive treatment at the time of hospital admission or if the blood pressure was considered >145mmof Hg systolic and 90mmof Hg diastolic. For lipid analysis samples were obtained over an overnight fast. Patients who had serum concentration of total cholesterol >240mg/dl or triglycerides >300mg/dl or LDL-c >160mg/dl or HDL-c<30mg/ dl are considered as hyperlipidemia.
Statistical analysis
All values are presented as mean+/-s.d. Statistical significance was analysed by student‘t’ test. The level of significance was set at p<0.05.For multivariate analysis median (50 percentile) was used as cut off value (as a marker) for differentiating the presence or absence of the disease.
Results
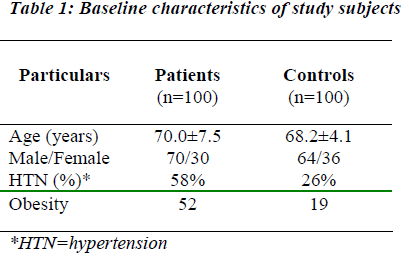
The clinical characteristics of ischemic stroke patients and control subjects are presented in Table no1.Among 100 ischemic stroke patients, 70% were males and 30% were females. Among 100 controls 64 were males and 36 were females. There are 52 patients with obesity and only 19 subjects among controls were obese and they are statistically significant (p<0.001). Among 100 ischemic stroke patients 58% had the history of hypertension and 26% in control group which was statistically significant (p<-0.001).
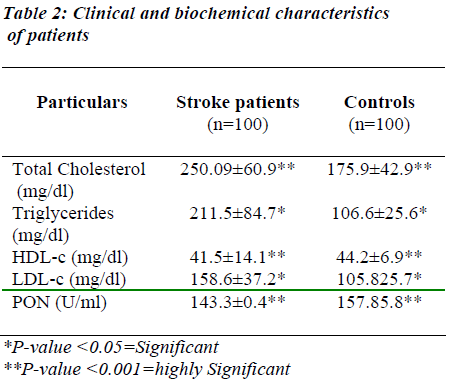
The clinical and biochemical characteristics of the patients and controls is described in Table-2.Stroke patients had highest TC (250.9 ±60.9 mg/dl), LDL-c (158.6 ±37.2 mg/dl) and highest triglyceride (211.5 +/-84.7 mg/dl) concentrations; in comparison, the normal subjects had significantly lower TC (175.9±42.9 mg/dl), lower LDL-c (105.8±25.7 mg/dl) and low triglyceride (106.6±25.6 mg/dl).Stroke patients had significantly lower HDL-c (41.5±14.1 mg/dl) and lower paraoxanase (143.4±0.4 U/ml) activity; in comparison, the control subjects had HDL-c (44.2±6.9 mg/dl) and highest paraoxanase (157.9 ±5.9 U/ml) concentrations.
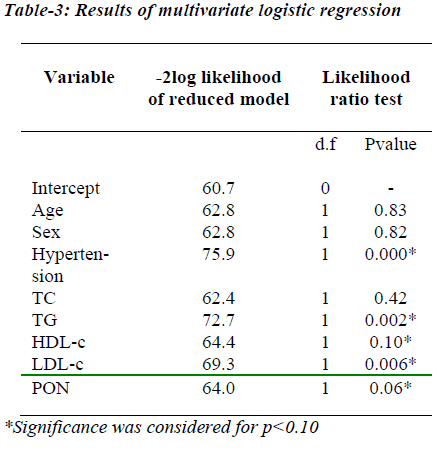
The multivariate regression analysis for risk factors versus ischemic stroke revealed that hypertension, increased triglycerides and LDL-c and decreased HDL-c, paraoxanase activities were significantly associated with the occurrence of ischemic stroke as indicated in Table 3.
Discussion
In this study, mean age of patients was 70.0+/-7.5 years. The incidence of ischemic stroke was high as 80% as given by health information in India in 1988. [16] Sex distribution in this study was 70% males and 30% females. The study was predominantly male oriented as ischemic stroke affects male’s severly and commonly than females increased serum cholesterol is causally associated with increased risk of ischemic stroke. Specifically a 10%increase in serum cholesterol is associated with 20 to 30% increased risk of stroke and elevations may be associated with higher risk of stroke as given by La Rosa. [17] Like other 16tudies [18,19,20] in our study hypertension diabetes mellitus were found to be significantly high.
Our current findings show that low serum PON activity in ischemic stroke patients was profoundly lower than controls. Similar observations are noticed in other studies. PON has been suggested as the factor responsible for an-tioxidant role of HDL. Several studies have shown an increase in the products of lipid peroxidation in plasma of patients with ischemic stroke [21] Further more LDL-c isolated from the plasma of patients of ischemic stroke has reported to be more susceptible to oxidation invitro than from normal subjects [22] and autoantibodies oxidized to lipoproteins are increased in patients with ischemic stroke. PON present on serum is reported to be located on HDL, low concentration of HDL increases susceptibility to atherosclerosis and consequently ischemic stroke [23].
In the current study, patients who sustained ischemic stroke did not on average have markedly decreased HDL concentration, but PON activity was profoundly decreased. Under most circumstances, the serum PON activity is therefore likely to be depending on the no. of PON molecules in HDL rather than the serum HDL concentration.
In summary, we have shown that PON activities towards nitro phenyl acetate were lower in subjects with ischemic stroke than in control subjects. So that identification of these individual factors has opened up different approaches other than simplify modifying the lipid profile and traditional risk factors in primary prevention of ischemic stroke. PON would thus be seen worthy of further study as an etiologic factor in the development of ischemic stroke and perhaps other diseases. Although the present study validates the earlier views that PON activities are indeed associated with ischemic stroke, further verification in large prospective case control studies to draw a concrete conclusion is warranted.
References
- Dalal PM. Ischaemic strokes, Management in first six hours.Neurol India 2001; 49: 104-115.
- La Du B. Human serum paraoxanase/arylesterase.In: Kalow W, editor. Pharmacogenetics of drug metabolism, New York: NY Pergamom press, 1992; p51-91.
- Mackness MI, Mackness B, Durrington PN. Paraoxanase in biochemistry,genetics and relationship to plasma lipoproteins. Current opinion Lipidol 1996; 7: 69-76.
- Parthasarthy S, Fong LG. HDL inhibits the oxidative modification of LDL. Biochim Biophys Acta 1990; 1044: 275-283.
- Klimov AM, Pleskov VM. Antioxidative effect of HDL in the oxidation of LDL. Bull Exp Biol Med (Russ) 1987; 103: 550-552.
- Mackness MI, Abott CA. The role of HDL and lipid soluble antioxidant vitamins in inhibiting LDL.J Clin Invest 1991; 88: 2039-2046.
- Steinberg D, Parthasarthy S, Khoo JC. Beyond cholesterol modifications of LDL that increases its atherogenicity. N Engl J Med 1989; 320: 915-924.
- Mackness MI, Durrington PN. HDL,its enzymes and its potential to influence lipid peroxidation. Atherosclerosis 1995; 115: 243-253.
- Mackness MI, Bhatnagar D et al. Serum PON activity in familial hypercholesterolemia and insulin dependent diabetes mellitus. Atherosclerosis 1991; 86: 193-198.
- Abott CA, Kumar S, Mackness MI. Serum paraoxanase activity, concentration and phenotype distribution in diabetes mellitus and its relationship to lipids and lipoproteins. Arterioscler Thromb Vasc Biol 1995; 15: 1812-1818.
- Ruiz J, James RW et.al. Gln Arg 192 polymorphism of paraoxanase and ischemic stroke. Lancet 1995; 346: 869-872.
- Serrato M, Marian AJ. A variant of human PON/arylesterase gene (HUMPONA) risk factor for coronary artery disease.J Clin Invest 1995; 96: 3005-3008.
- Sanghera DK, Saha N. Genetic polymorphism of PON and risk of coronary heart disease. Arterioscler Thromb Vasc Biol 1997; 17: 1067-1073.
- Pati N, Pati U. Paraoxanase gene polymorphism and coronary artery disease in Indian subjects. Int J Cardiol 1998; 66: 165-168.
- Gan KN, Smolen A, Eckerson HW. Purification of human serum paraoxanase / arylesterase.Evidence for one esterase’s catalyzing both activities. Drug Metab Dispos 1991; 19: 100-106.
- Bhatnagar D, Anand IS et.al. Coronary risk factors in people from Indian subcontinent living in West India and their siblings in India. Lancet 1995; 345: 405-409.
- La Rosa JC. The cholesterol facts. A joint statement by the Am Heart Assoc and NHLBI. Circulation 1990; 81: 1721-1733.
- Uhl GS, Farell PW. Myocardial infarction in adults: risk factors and natural history. Am Heart J 1983; 105: 548-553.
- Chen L, Chester M, Kaski JC. Clinical factors and angiographic features associated with premature coronary artery disease. Chest 1995; 108: 364-369.
- Zimmermann FH, Fisher LD, et.al. Myocardial Infarction in young adults: angiographic characterization, risk factors and prognosis. J Am Coll Cardiol 1995; 26: 654-661.
- Liu K, Cuddy T. Oxidative status of lipoproteins in coronary disease patients. Am Heart J 1992; 123: 285-289.
- Regnstrom J, Nilsson J, Hamsten A. Susceptibility to low density lipoprotein oxidation and coronary athero-sclerosis in man. Lancet 1992; 339: 1183-1185.
- Mackness MI. ‘A’-esterases: enzymes looking for a role? Biochem Pharmacol 1989; 38: 385-390.