Case Report - Archives of General Internal Medicine (2019) Volume 3, Issue 2
Rare orbital manifestations and vasculitis, giant cell arteritis or side effects of zoledronic acid infusion?
Nazanin Naderi*Department of Rheumatology, Danderyd Hospital, Stockholm, Sweden
- *Corresponding Author:
- Nazanin Naderi
Department of Rheumatology
Danderyd Hospital
Stockholm
Sweden
E-mail:Nazanin.naderi.f@gmail.com
Accepted Date: June 17, 2019
Citation: Naderi N. Rare orbital manifestations and vasculitis, giant cell arteritis or side effects of zoledronic acid infusion? 2019; 3(2): 6-7.
Abstract
Giant cell arteritis (GCA), affects an age group where osteoporosis is common. A well-established treatment for osteoporosis is medication with bisphosphonates. Bisphosphonates are overall welltolerated but can trigger several different acute inflammatory reactions with systemic features and symptoms and signs from the ocular and musculoskeletal system, all of which resemble those of GCA. Here is described a second case of GCA brought about by zoledronic acid infusion, presenting with cranial, orbital and systemic features; diagnosed through ultrasound with both cranial and extra-cranial vessel involvement and successfully treated with glucocorticoids.
Keywords
Giant cell arteritis, Orbital manifestations, Swollen eyelids, Conjunctivitis, Blepharitis, Keratitis, Zoledronic acid, Side effect, Adverse event.
Introduction
Zoledronic acid is a bisphosphonate that is well-established and effective in the treatment of osteoporosis. Although generally well-tolerated it can provoke acute inflammatory reactions, including: headache, fever, musculoskeletal pain, joint swelling, general malaise, fatigue and eye inflammation, all of which also symptoms and signs of giant cell arteritis (GCA).
The ocular side effects of zoledronic acid are conjunctivitis, eye pain, uveitis/iritis, episcleritis and scleritis and the ones related to the vascular system are hyper-or hypotension as reported by the pharmaceutical company and the literature. Vasculitic reaction to the drug with development of clinical GCA has been reported only once previously.
Case Presentation
Medical history and clinical presentation
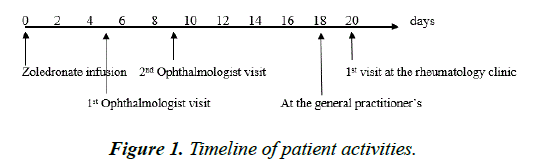
A 99-yerar-old male was referred to the rheumatologic clinic inquiring possible GCA in the middle of February 2019. He had an unremarkable past medical history with atrial fibrillation treated with apixaban, osteoporosis treated with a first infusion of zoledronic acid a few weeks earlier and close in time two visits to two separate ophthalmologic units. At the first ophthalmological evaluation he presented with red and painful right eye of a few days duration, was diagnosed with bilateral keratoconjunctivitis and given eye drops. The eye drops were without effect, prompting a visit to a second ophthalmologist a few days later with complains of swollen eyelids and bilateral eye pains. He was diagnosed with pronounced bilateral blepharitis and given a different type of eye drops. Ten days later he visits the general practitioner due to right sided headache, tenderness of the left cheek and left forehead towards the scalp, fatigue, loss of appetite last few days, some weight loss, chills and pressure pain behind the left eye but no fever, visual symptoms, jaw claudication or neck-shoulder-hip-girdle pains, Figure 1. According to the patient these problems started the day after the zoledronic acid infusion.
Clinical findings at first visit
Physical examination at first visit revealed no cardiac murmur or vessel bruits over the common carotid, subclavian, axillary, renal or common femoral arteries. The radial and femoral pulses and brachial blood pressures were equal. The temporal arteries (TA) were clearly visible on both sides without any redness, tenderness or discolouration but with some resistance on palpation. Bilateral slightly discoloured swollen upper and lower eyelids and some redness of both conjunctiva. Left eye with slight proptosis. Laboratory analysis with erythrocyte sedimentation rate (ESR) 10 mm/h, C-reactive protein (CRP) <1 mg/L, platelets 225x109/L, hemoglobin 151g/L.
Investigations, treatment and disease course
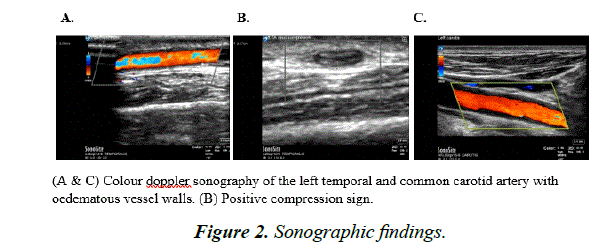
Ultrasonography of the left temporal, common carotid, axillary and femoral arteries revealed unequivocal vasculitis of the temporal and common carotid arteries and suspicious involvement of the axillary artery, Figure 2. Glucocorticoid treatment with prednisolone 40 mg/day was initiated with prompt response. Temporal artery biopsy (TAB) and magnetic resonance imaging of the orbits were suggested but the patient declined. A computed tomography angiography of the aorta seven days after prednisolone initiation, showed no vasculitis. The prednisolone could be tapered without any flare and was discontinued in the beginning of May.
Discussion
A search of the English literature using the keywords “giant cell arteritis”, “temporal arteritis”, “vasculitis”, “large vessel vasculitis”, “adverse events”, “side effects”, “zoledronic acid” and “zoledronate” in PubMed, Web of Science, Embase, Google Scholar and the databases for adverse events SIDER and Micromedex yielded only one result.
Present case is the second report of GCA provoked by zoledronic acid infusion, but the first confirmed through imaging and demonstrating large vessel involvement as well. Metyas et al. reported on a 84-year-old woman with osteoporosis developing fever, myalgia, fatigue, flue-like symptoms, pain and swelling around the left eye, left sided jaw pain and left temporal headache three days after her first zoledronic acid infusion. Clinical examination revealed tender left TA with diminished pulsation, ESR 65 mm/h. Bilateral TAB was non-diagnostic [1].
The eye manifestations described in this case are most probably due to adverse drug reactions, considering the striking time relationship with the zoledronate infusion and consistent with previous reports [2,3]. Of note, GCA can in rare instances present with the same orbital manifestations described here: eyelid swelling/oedema [4-7], conjunctivitis [4-6,8-10], proptosis [4- 7,11,12], keratitis [13,14].
Another interesting and remarkable finding was the normal levels of ESR and CRP at the time of diagnosis, given the intense orbital inflammation, the systemic features and the presence of large vessel vasculitis. This is an uncommon finding with a reported frequency of up to 4% [15-18].
In conclusion, vasculitis i.e. GCA, should join the list of adverse side effects of zoledronic acid and physicians should be aware of this rare complication.
The patient’s written informed consent has been obtained for publication.
References
- Metyas S, Ibrahim M, Solyman J, et al. Giant cell arteritis with visual loss following zoledronic acid infusion. Int J Rheum Dis. 2014;17(1):113-5.
- Patel DV, Horne A, House M, et al. The incidence of acute anterior uveitis after intravenous zoledronate. Ophthalmology. 2013;120(4):773-6.
- Patel DV, Bolland M, Nisa Z, et al. Incidence of ocular side effects with intravenous zoledronate: Secondary analysis of a randomized controlled trial. Osteoporos Int. 2015;26(2):499-503.
- Gibbs P. Temporal arteritis: Onset with pseudotumour orbit or red eye. Practitioner. 1974;213(1274):205-11.
- Clark AE, Victor WH. An unusual presentation of temporal arteritis. Ann Ophthalmol. 1987;19(9):343-6.
- Lee AG, Tang RA, Feldon SE, et al. Orbital presentations of giant cell arteritis. Graefes Arch Clin Exp Ophthalmol. 2001;239(7):509-13.
- Islam N, Asaria R, Plant GT, et al. Giant cell arteritis mimicking idiopathic orbital inflammatory disease. Eur J Ophthalmol. 2003;13(4):392-4.
- Naderi N. Splinter hemorrhage as a telltale of active extra-cranial giant cell arteritis: A case report and review of the literature. Arch Gen Intern Med. 2019;3(1):10-2.
- Mitchell JR, Krashin-Bichler I, Rosenblum M, et al. Giant cell arteritis presenting with bilateral orbital inflammatory disease and enhancing superficial temporal arteries. Pract Neurol. 2014;14(6):446-7.
- Zenone T, Souquet PJ, Bohas C, et al. Unusual manifestations of giant cell arteritis: Pulmonary nodules, cough, conjunctivitis and otitis with deafness. Eur Respir J. 1994;7(12):2252-4.
- Laidlaw DA, Smith PE, Hudgson P. Orbital pseudotumour secondary to giant cell arteritis: An unreported condition. BMJ. 1990;300(6727):784.
- Nassani S, Cocito L, Arcuri T, et al. Orbital pseudotumor as a presenting sign of temporal arteritis. Clin Exp Rheumatol. 1995;13(3):367-9.
- Long RG, Friedmann AI, James DG. Scleritis and temporal arteritis. Postgrad Med J. 1976;52(613):689-92.
- Papathanassiou M, Elezoglu A, Nikita E, et al. A rare case of peripheral ulcerative keratitis in temporal arteritis. Eur J Ophthalmol. 2009;19(5):866-9.
- Naderi N, Mohammad AJ, Turesson C. Large vessel involvement in biopsy-proven giant cell arteritis: Incidence, distribution, and predictors. Scand J Rheumatol. 2017;46(3):215-21.
- Kermani TA, Schmidt J, Crowson CS, et al. Utility of erythrocyte sedimentation rate and c-reactive protein for the diagnosis of giant cell arteritis. Semin Arthritis Rheum. 2012;41(6):866-71.
- Parikh M, Miller NR, Lee AG, et al. Prevalence of a normal C-reactive protein with an elevated erythrocyte sedimentation rate in biopsy-proven giant cell arteritis. Ophthalmology. 2006;113(10):1842-5.
- Myklebust G, Gran JT. A prospective study of 287 patients with polymyalgia rheumatica and temporal arteritis: Clinical and laboratory manifestations at onset of disease and at the time of diagnosis. Br J Rheumatol. 1996;35(11):1161-8.