Research Article - Archives of General Internal Medicine (2017) Volume 1, Issue 1
Psychosocial Differences of Bariatric Surgery Candidates.
Carlos J van der Hofstadt Román1,2,4, César Leal Costa3*, Sonia Tirado González2, Enrique Pérez Martínez4,5,6 and Jesús Rodríguez-Marín1,2,41Clinical and Health Psychology Unit, University General Hospital of Alicante, Spain
2Department of Psychology, Miguel Hernández University of Elche, Spain
3Faculty of Nursing, Catholic University of Murcia, Spain
4Alicante Institute for Health and Biomedical Research (ISABIAL-FISABIO Foundation), Alicante, Spain
5Department of Clinical Medicine, Universidad Miguel Hernández de Elche, Elche, Spain
6Psychiatry Service, Alicante University General Hospital, Alicante, Spain
- *Corresponding Author:
- César Leal Costa
Nursing Department
Catholic University of Murcia, Spain
E-mail: cleal@ucam.edu
Accepted on January 15, 2017
Citation: van-der Hofstadt CJ, Leal C, González S, et al. Psychosocial differences of bariatric surgery candidates. Arch Gen Intern Med. 2017;1:6-13
Abstract
Background and objectives: Patients with Morbid Obesity (MO) asking for weight loss and candidates to Bariatric Surgery (BS) are commonly administered extensive psychiatric and psychological assessment prior to surgery. The purpose of the present study was to investigate if there are differences among BS candidates, according to psychosocial variables.
Methods: Data was obtained from a random sample of 463 BS candidates at a General University Hospital, using measures of socio-economic (age, gender, marital status, employment and highest education level), medical and psychological variables (State-Trait Anxiety Inventory, Beck Depression Inventory, and Eating Disorder Inventory-2).
Results: Data show that there were differences between morbidly and super morbidly obese groups only in the scale of Body Dissatisfaction obtained on the EDI-2. We also found differences between men and women in trait anxiety and in concerns about weight, satisfaction with their physical appearance, with feelings of inadequacy, worthlessness and without control over their lives, and satisfaction with anything less than something perfect.
Conclusions: We have found a differential psychosocial profile for women, and we think it can be taken into account to design and implement specific programs of BS preparation and follow-up.
Keywords
Morbid obesity, Bariatric surgery, Anxiety, Depression, Eating disorders
Introduction
Morbid Obesity (MO) has significant cognitive, emotional and behavioral components and Bariatric Surgery (BS) to succeed requires their identification and understanding and long-term changes in one or all of them. Ability to understand of the risks and benefits of surgery, knowledge of the surgical procedure, expectations for weight loss, health outcomes, and BS psychosocial impact, are accepted as being important factor [1-3]. There is some evidence of a worse postoperative outcome in individuals with preoperative psychopathology, and we need more information regarding the psychosocial variables associated with weight loss and mental health after surgery. This information is essential for detecting patients in need of psychological support after BS [4]. So the standard clinical guidelines for BS enclose a preoperative Psychological Evaluation (PE) as an important element to make a correct selection of BS candidates and to identify patients with a contraindication for surgery and to decrease psychosocial disturbances after surgery [5-11]. Current illicit drug use, active symptoms of schizophrenia, severe mental retardation, and lack of knowledge about the surgery were the most commonly cited contraindications for BS. PE is also important in the detection of emotional, psychiatric, cognitive and behavioral factors that can influence the surgery’s success and long-term weight loss. PE is not only aimed at identifying predictors of BS success but also includes the development of an individually tailored intervention to increase the patients’ post-surgery success [12- 14]. In fact, the literature suggests that psychiatric comorbidity may be more prevalent in morbid obese patients longing for BS, especially if we include binge eating disorders, affective disorders, anxiety, bulimia, tobacco addiction and personality disorders [12].
There is no standardized PE protocol, but the most common procedure is a clinical interview accompanied by objective measurement of several variables through self-administered questionnaires [1,12,15]. These measures range from questionnaires specifically developed for MO, like the Boston Interview for Gastric By-pass [14], to a variety of questionnaires specific to assess eating disorders (BITE-2, EAT), depression and anxiety (BDI, STAI, HADS) and instruments for personality assessment (MMPI-2, MCMI) [12]. In Spain there are also specific proposals referring to patient selection from a psychological point of view [16] as well as in a broader sense [11,16-18].
Generally, the presence of psychiatric disorders in the candidates recommends waiting approximately one year before BS [19], and the binge eating disorder must be treated before BS because it is considered a negative predictive factor for weight loss [20]. According other studies, gender is important, sustaining that women have higher values in all studied psychopathological parameters, like depression, paranoid ideation, interpersonal sensitivity, social anxiety and a greater number of prior treatments for mental health [21-22].
In any case, in spite of the frequency of such assessments, there is no consensus about what it is that may constitute a very appropriate assessment or what might be the reasons for denying surgery a candidate; but there is a general agreement that a PE is necessary (but is not sufficient) and on the factors to assess: eating behaviors, stress and coping, social support, capacity to consent and understanding of the risks and benefits of surgery, knowledge of the surgical procedure, and expectations for weight loss, health outcome, and psychosocial impact [3-4,23].
Other studies, examining the rates for psychological denial of BS, state that the refusals for psychosocial reasons range from 2% to 6% [3,24]; or show that between 3% and 20% of the candidates are excluded due to psychiatric reasons. However it is also well established that the sole presence of psychiatric disorders must not be taken as an absolute exclusion criterion for BS [13]. In any case, the psychological variables have not been predictors of weight loss in the majority of studies [12]. We only can find limited evidence indicating that anxiety and depression symptoms can be positive predictors for weight loss [18,23,25-26]. There is also limited evidence that binge eating disorder before BS is a negative predictor for weight loss following surgery, as it only appears in retrospective studies but not in prospective ones [12,27]. The lack of findings with psychological predictors may be due to the use of small and too selective samples.
In spite of all this, it seems useful to evaluate BS candidates on the basis of psychological and socio-demographic variables, in order to establish if there are differences that may be important in order to pre-surgery or post-surgery. So, the purpose of present study was to analyze medical and psychosocial variables in a population of morbidly obese patients attending BS at the Multidisciplinary Unit of Obese Patient Comprehensive Care (UMAIO) in the University General Hospital of Alicante (HGUA), Spain, in order to investigate if there are differences among them.
Method
Participants
During the 60 months the program operated, 463 of the 521 candidates complied with the entire assessment protocol, resulting in a participation level of 88.8%. Of these, 353 (76.2%) patients were apt to begin the program directly following the initial assessment, 35 (7.7%) were apt but with the recommendation of undertaking a preliminary monitored diet, 63 (13.6%) were apt under the condition of continuing their mental health treatment, and 12 (2.5%) patients were initially refused, with a subsequent reassessment proposed for them.
The inclusion criteria were: 1) Age between 18 and 60 years; 2) BMI > 40 kg/m2 or BMI ≥ 35 kg/m2 with specific comorbidities to undergo bariatric surgery; 3) Evolution of morbid obesity >5 years refractory to properly supervised conservative treatments; 4) Absence of endocrine pathology; 5) Absence of severe or acute psychiatric disorders; and 6) Ability to understand the mechanisms of weight loss through bariatric surgery and the commitment to adhere to a postoperative monitoring regimen.
Absolute exclusion criteria included the presence of an active eating disorder, substance abuse, unstable severe psychiatric disorders and severe mental retardation (IQ<50). Relative exclusion criteria included moderate mood disorders, severe personality disorders and lack of family support.
Procedure
The “Pre-surgery Group Intervention Multidisciplinary Program” is performed by the UMAIO at the HGUA. Once patients are admitted and assessed by the HGUA service of endocrinology and it is confirmed that they comply with the specific basic medical requirements to be included in the program, they are derived to UMAIO and their mental health is assessed.
After all the tests are completed, each case is evaluated and accepted by the Committee for Bariatric Surgery. Then the admitted patients carrying out the "Group Intervention Multidisciplinary Pre-surgery Program", implemented by the Department of Endocrinology (to achieve significant weight loss before surgery), the Department of Surgery (for information about surgical process and consequences), and the Unit of Clinical Health Psychology (UCHP), which is responsible for the psychological intervention program in order to establish and maintain a post-surgery healthy eating behavior [28].
All subjects reviewed and signed a statement of informed consent detailing the purpose, procedures, and goals of the study. The Ethical Committee of the hospital approved this study with code PI 2009/50.
Variables and instruments
PE tests given to the patients during their first contact with the UCHP are the following: A socio-medical record to assess socio-demographic variables (sex, age, education level, profession, marital status, living arrangements, and monthly income), medical and psychopathological history, and anthropometric data (weight and height).
The State-Trait Anxiety Inventory (STAI) by Spielberger et al. (Spanish adaptation by Seisdedos [29]) to measure anxiety. A Spanish version of the STAI was also reported to have good internal consistency (0.9-0.93 for state anxiety, and 0.84-0.87 for trait anxiety).
The Beck Depression Inventory (BDI) for depression assessment. The 13-item abbreviated version was used, adapted to Spanish by Conde and Useros [30]. The correlation between the short and long form is r=0.96.
The Eating Disorder Inventory (EDI-2) [31], Spanish adaptation by Garner [32] for an assessment of the severity of the symptomatology of eleven dimensions that is clinically relevant in the case of eating behavior disorders: DT: Drive for Thinness; B: Bulimia; BD: Body Dissatisfaction; I: Ineffectiveness; P: Perfectionism; ID: Interpersonal Distrust; IA: Interoceptive Awareness; MF: Fear of Maturity; A: Asceticism; IR: Impulse Regulation, and; SI: Social Insecurity. The instrument reliability for this adaptation by Garner as evaluated through Cronbach's alpha ranges from 0.83 to 0.93.
Statistical analyses
Statistical analyses were conducted using IBM SPSS Statistics 19 software (SPSS, Inc., Chicago, IL, USA). Descriptive statistics were expressed as frequencies, percentages, means, and standard deviations for variables as appropriate. The t-tests were used to determine differences in anthropometric characteristics, symptoms associated with eating disorders, anxiety and depression by gender. The level of statistical significance was set at p<0.05.
Results
Descriptive
The 463 patients have an average age of 42.3 ± 9.9 years. The gender distribution is 308 women (66.5%) with an average age of 42.5 ± 10.5 years, and there were 155 men (33.5%) whose average age was 42 ± 8.8 years.
Table 1 shows the distribution of the principal demographic variables. As can be seen, the majorities of the patients shown is married and lives with their own family, have completed either primary or secondary education, are actively employed and earn average monthly incomes between 500 and 2000 Euros.
| Variables | n | % |
|---|---|---|
| Marital status | ||
| Single | 97 | 21 |
| Married | 292 | 63 |
| Widowed | 14 | 3 |
| Separated/Divorced | 60 | 13 |
| Living arrangements | ||
| Alone | 31 | 6.7 |
| Family of origin | 83 | 17.9 |
| Own family | 342 | 73.9 |
| Other | 7 | 1.5 |
| Education | ||
| None | 32 | 6.9 |
| Primary | 207 | 44.7 |
| Secondary | 157 | 33.9 |
| Post-secondary | 67 | 14.5 |
| Monthly income | ||
| <500 € | 50 | 10.8 |
| 500-1000 € | 159 | 34.3 |
| 1000-2000 € | 164 | 35.4 |
| >2000 € | 89 | 19.2 |
| Employment situation | ||
| Employed | 211 | 45.6 |
| Temporary disability | 25 | 5.4 |
| Permanent disability | 18 | 3.9 |
| Retired | 8 | 1.7 |
| Unemployed | 128 | 27.6 |
| Homemaker | 73 | 15.8 |
| Diseases | ||
| Diabetes Mellitus | 116 | 25 |
| Hypertension | 173 | 37.4 |
| Dyslipidemia | 137 | 29.6 |
| Hyperuricemia | 48 | 10.4 |
| Ischemic heart disease | 36 | 7.8 |
| Osteoarthritis | 113 | 24.4 |
| OSA | 204 | 44 |
| Asthma | 45 | 9.7 |
| Amenorrhea/ | 52 | 11.2 |
| Infertility* | ||
| Psychopathological antecedents | ||
| Depression | 99 | 21.4 |
| Anxiety | 122 | 26.3 |
| Physical/sexual abuse | 29 | 6.3 |
Table 1. Descriptive statistics (frequencies and percentages) of demographic variables and comorbidities.
For anthropometric indicators, values superior to 40 on the Body Mass Index (BMI) were obtained in 55.1% of the sample (255 participants), thereby complying with the criteria for a morbid obesity diagnosis. Another 39.5% (183 participants) presented values superior to 50 (super morbid obesity). The BMI value ranged from 35.3 to 83.5.
Statistically significant differences were found between the BMI>40 (M=18.9, SD=6.4) and BMI>50 (M=20.2, SD=6.0) groups. On the other hand, in the 11 scales of the EDI-2 statistically significant differences only in the scale of Body Dissatisfaction (BD) t (-2.2), p<0.05 were obtained.
Table 2 shows the data distribution by gender. Statistically and clinically significant differences were found between men and women in terms of weight and height, but not in terms of BMI. Following the criteria of Cohen [33], these logical differences are great, just as the r coefficient of effect size in both cases reflects (0.67 and 0.57, respectively).
| Height | M (SD) | t | r |
|---|---|---|---|
| Total | 165.1 (9.7) | - | - |
| Male | 174.3 (6.7) | 19.3* | 0.67 |
| Female | 160.5 (7.5) | - | - |
| Weight | |||
| Total | 135.3 (25.4) | - | - |
| Male | 152.8 (26.5) | 10.9* | 0.57 |
| Female | 126.7 (19.8) | - | - |
| BMI | |||
| Total | 49.6 (8.5) | - | - |
| Male | 50.2 (8) | 1.1 | 0.05 |
| Female | 49.3 (8.8) | ||
| STAI-E | |||
| Total | 18.1 (10.7) | - | - |
| Male | 17.2 (9.6) | -1.5 | 0.08 |
| Female | 18.6 (11.2) | ||
| STAI-R | |||
| Total | 23.4 (11.5) | - | - |
| Male | 21.0 (10.9) | -3.2* | 0.15 |
| Female | 24.6 (11.7) | - | - |
| BDI | |||
| Total | 7.5 (5.3) | - | - |
| Male | 7 (4.8) | -1.7 | 0.09 |
| Female | 7.8 (5.5) | - | - |
| M: Mean; SD: Standard Deviation; t: t-test; r: Effect size. *p<0.05 | |||
Table 2. Comparison the anthropometric characteristics and anxiety/ depression symptoms by gender.
Table 1 shows that the diseases most frequently affecting our patients are OAS (44%), hypertension (37.4%), dyslipidemia (29.6%), diabetes mellitus (25%), osteoarthritis (24.4%) and nonalcoholic fatty liver disease (22%). Among women, 11.2% suffer from amenorrhea or infertility, with another 9% from polycystic ovary. Regarding psychopathological antecedents, it is worth pointing out that 26.3% suffer from anxiety and 21.4% depressive symptoms, while 15.8% present comorbidity.
The sample presents a very low index in psychoactive substances (three subjects consume only alcohol, one subject consumes alcohol, cannabis and other stimulants; one subject consumes cannabis and stimulants; one cannabis and another stimulants). Regarding psychotropic drug consumption, those most utilized are antidepressants (19.2%) and anxiolytics (17.9%), in addition to the consumption of antipsychotics (1.5%) and mood stabilizers (1.1%). 15% of the patients are found to be in outpatient treatment at a mental health unit, and seven subjects have undergone some psychiatric hospitalization.
Anxiety and depression
Women score slightly higher in state and trait anxiety, although these differences are neither statistically significant nor clinically relevant in the case of state anxiety (Table 2).
Comparing with the normative scales of adults of the Seisdedos Spanish adaptation [29], our patients do not present state anxiety nor trait anxiety clinical levels.
On the other hand, by comparing the scores obtained in the BDI with the cutoffs established by Conde and Usero 30, we find that the sample average (7.5 ± 5) is found between the cutoff proposed by light depression and moderate depression (range BDI total score 5-7 for light depression and 8-15 for moderate depression). According to these criteria, 33.5% of patients either do not suffer from depression or their levels are minimum (0-4), 24.2% suffer light depression (5-7), 34.3% moderate depression levels (8-15), and 8% severe depression. We did not find differences significant or clinically relevant between men and women on the depression score.
Symptoms related with eating disorders
The results of the principal descriptive statistics of scores from EDI-2 are shown in Table 3.
| DT | M (SD) | t | r |
|---|---|---|---|
| Total | 10.7 (5.1) | - | - |
| Male | 9.7 (5.2) | -2.9* | 0.13 |
| Female | 11.2 (5.1) | - | - |
| B | |||
| Total | 1.8 (3.0) | - | - |
| Male | 1.9 (3.1) | 0.5 | 0.02 |
| Female | 1.8 (3.0) | - | - |
| BD | |||
| Total | 19.2 (6.4) | - | - |
| Male | 17.6 (7.0) | -3.7* | 0.22 |
| Female | 20.0 (5.9) | - | - |
| I | |||
| Total | 4.0 (4.7) | - | - |
| Male | 3.3 (4.2) | -2.5* | 0.12 |
| Female | 4.5 (5.0) | - | - |
| P | |||
| Total | 3.7 (3.5) | - | - |
| Male | 4.4 (3.7) | 3.1* | 0.14 |
| Female | 3.4 (3.1) | - | - |
| ID | |||
| Total | 3.0 (3.7) | - | - |
| Male | 3.2 (3.8) | 0.7 | 0.03 |
| Female | 3.0 (3.7) | - | - |
| IA | |||
| Total | 4.7 (4.9) | - | - |
| Male | 4.3 (4.8) | -1.2 | 0.06 |
| Female | 4.9 (4.9) | - | - |
| MF | |||
| Total | 6.3 (4.6) | - | - |
| Male | 6.5 (4.8) | 0.5 | 0.02 |
| Female | 6.3 (4.5) | - | - |
| A | |||
| Total | 5.0 (3.5) | - | - |
| Male | 5.4 (3.6) | 0.6 | 0.03 |
| Female | 5.0 (3.4) | - | - |
| IR | |||
| Total | 2.3 (4.0) | - | - |
| Male | 2.3 (4.2) | -0.2 | 0 |
| Female | 2.4 (3.9) | - | - |
| SI | |||
| Total | 3.3 (3.9) | - | - |
| Male | 3.0 (3.5) | -1 | 0.05 |
| Female | 3.4 (4.0) | - | - |
| M: Mean; SD: Standard Deviation; t: t-test; r: Effect size. *p<0.05 | |||
Table 3. Comparison of symptoms associated with eating disorder by gender.
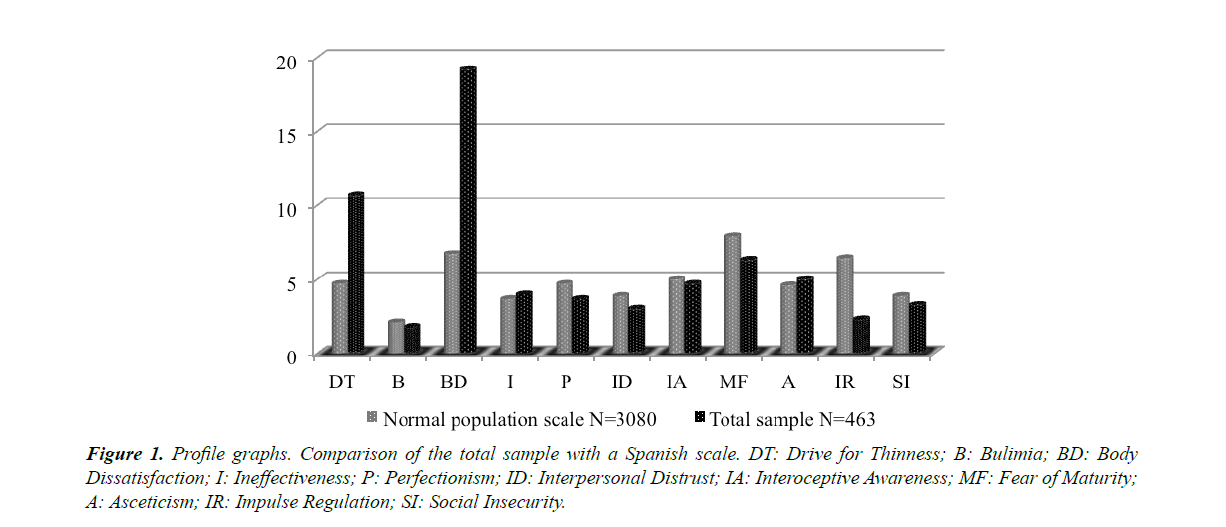
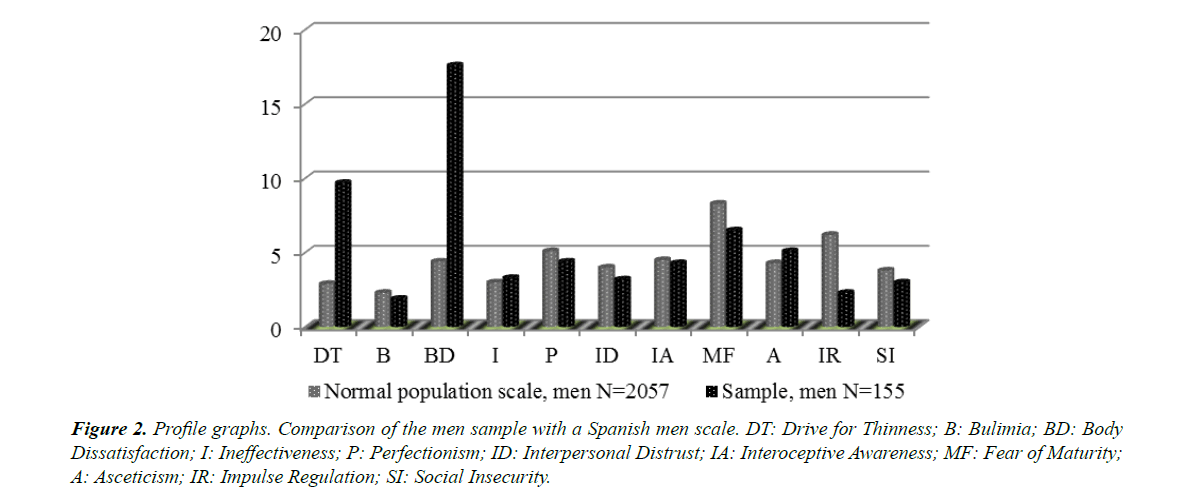
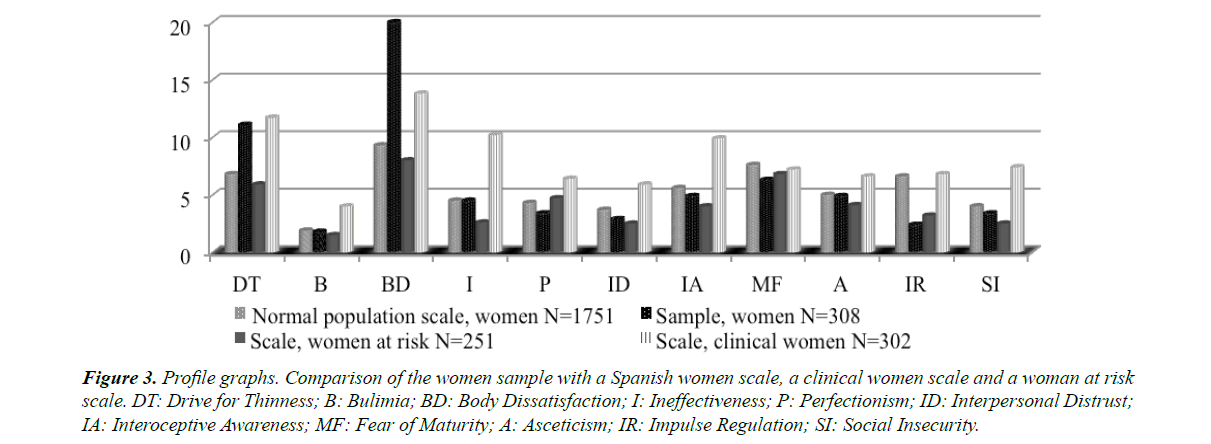
Statistically significant and clinically relevant differences were found between both sexes on the scales of DT, BD and I. Women obtain a higher score and men received a higher score in P. The effect sizes of such differences are medium-low (0.13, 0.22, 0.12 and 0.14, respectively) (Figures 1-3).
Figure 1. Profile graphs. Comparison of the total sample with a Spanish scale. DT: Drive for Thinness; B: Bulimia; BD: Body Dissatisfaction; I: Ineffectiveness; P: Perfectionism; ID: Interpersonal Distrust; IA: Interoceptive Awareness; MF: Fear of Maturity; A: Asceticism; IR: Impulse Regulation; SI: Social Insecurity.
Figure 2. Profile graphs. Comparison of the men sample with a Spanish men scale. DT: Drive for Thinness; B: Bulimia; BD: Body Dissatisfaction; I: Ineffectiveness; P: Perfectionism; ID: Interpersonal Distrust; IA: Interoceptive Awareness; MF: Fear of Maturity; A: Asceticism; IR: Impulse Regulation; SI: Social Insecurity.
Figure 3. Profile graphs. Comparison of the women sample with a Spanish women scale, a clinical women scale and a woman at risk scale. DT: Drive for Thinness; B: Bulimia; BD: Body Dissatisfaction; I: Ineffectiveness; P: Perfectionism; ID: Interpersonal Distrust; IA: Interoceptive Awareness; MF: Fear of Maturity; A: Asceticism; IR: Impulse Regulation; SI: Social Insecurity.
We found important differences when comparing the different scales, as shown by the following results obtained from EDI-2
- DT: 10.7 ± 5.1. This supposes a very high value with respect to the general Spanish population (4.7 ± 5.4) and to the sample of cases of women at risk (5.9 ± 5.5), although closer to the normative sample of clinical cases of women (11.7 ± 7).
- B: 1.8 ± 3.0. This is a value very similar to the normative sample of the normal population (2.1 ± 2.8) and to the sample of women at risk (1.5 ± 2.6). It is located a bit farther from the value of the sample of clinical cases of women (3.9 ± 5).
- BD: 19.2 ± 6.4. This has the highest value compared to normative samples, although closer to the clinical cases of women (13.8 ± 8.8) than to women at risk (8.1 ± 7.3) and the normal population (6.7 ± 6.8).
- I: 4.0 ± 4.7. This constitutes a value very similar to the normative sample of the normal population (3.7 ± 4.2) and to the sample of women at risk (2.6 ± 3.2). It is found farther from the value of the sample of clinical cases of women (10.3 ± 7.9).
- P: 3.7 ± 3.5. This is the lowest value compared to the normative samples, although it is closer to the normal population sample (4.7 ± 3.6) and to that of women at risk (4.7 ± 3.8) than to clinical cases of women (6.4 ± 4.5).
- ID: 3.0 ± 3.7. This is a value more similar to that of the cases of women at risk (2.5 ± 2.8) and to the normal population (3.9 ± 3.4). More differentiated from the clinical cases of women (5.9 ± 5).
- IA: 4.7 ± 4.9. This is the lowest value compared to the normative samples. It is closer to the normal population sample (5 ± 4.5) and to women at risk (3.8 ± 4.1) than to the clinical cases of women (10 ± 7.2).
- MF: 6.3 ± 4.6. In this case, this value is similar to the remaining normative values, women at risk (6.8 ± 4.5), clinical cases of women (7.2 ± 5.5) and the normal population (7.9 ± 4.6).
- A: 5.0 ± 3.5. This value is very similar to the normal population (4.6 ± 3.3) and to women at risk (4.1 ± 3). It is farther from the average value of women with clinical values (6.6 ± 4.7).
- IR: 2.3 ± 4.0. This is the lowest value when compared to normative samples, the normal population (6.4 ± 5.2), women at risk (3.2 ± 4) and clinical cases of women (6.8 ± 6.1).
- SI: 3.3 ± 3.9. This is closer to the normal population (3.9 ± 3.8) and women at risk (2.5 ± 3.1) than to clinical cases of women (7.4 ± 5.4).
Generally, our sample profile is more similar to the general population for the complete group as well as for men and women specifically, except for the case of the scales of DT and BD, where higher scores are reached, approaching more the pattern of the population of clinical cases of women. However, we must highlight that the average BMI of the sample to the EDI-2 Spanish adaption was 20.7 ± 3.4 in men and 20.1 ± 2.5 in women, quite distant from the data obtained in our patients.
Discussion
This study analyzed medical and psychosocial variables in obese patient candidates for BS.
We did not find differences in any variable between patients with either MO or super MO (BMI>50). This result is normal in the majority of reviewed studies. Only one of them found that the EAT and SCL-90-R scores, that refer to eating disorders and general psychopathology respectively, are greater in the morbidly obese patients than in the super morbid ones [22].
Of the total patients, 25% suffer from anxiety and 20% depressive symptoms. These values are within the lower range of the results described in the literature, within which, as we already presented, have been described psychopathological in Axis I of the DSM-IV-TR between the 20% to 60% of the patient samples with OM sent to BS [13,22]. The data obtained in the STAI indicate that there are no statistically significant or clinically relevant differences in state anxiety between men and women, but they do exist in the case of trait anxiety. These results agree with the idea that men tend to negate trait anxiety, and so this scale generally shows values elevated more in women than in men [29].
Regarding EDI-2 scores, patients present a profile very similar to that found in the literature. So, we found statistically significant differences and clinically relevant between men and women in the EDI-2 scales (DT, BD, I and P), similarly to results obtained in the Spanish questionnaire adaptation [32]. The authors found that males and females reflected different attitudes towards personal, physical and social aspects related with eating behavior, and, particularly, women stood out significantly by their bigger scores in DT, BD, I and IA, while males only stood out slightly in P.
Garner et al. [31] applied the EDI to a group of obese women and another group who had been obese, and found that the obese scored higher than the original non-clinical group in DT, BD and B scales, and additionally scored higher than those who had been obese in the BD scale.
Calderón et al. [34] found that adolescents with severe obesity presented an elevated concern for their physical aspect (BD and DT) and for their social surroundings (ID), as well as a moderate presence of subjective tension (S-A and T-A). Britz et al. [35] reached similar results with a sample of young adolescents between 15 and 21 with extreme obesity, presenting more affective, somatoform and eating disorders when compared to the control group with normal weight.
So, it seems that MO leads to social and occupational isolation, as well as the development of severe comorbidity [36]. Therefore it is logical that obese individuals feel rejected by society and may develop serious emotional and psychological problems. BS usually leads to a significant improvement of psychopathological parameters in patients, for the decrease in the social stigma with weight loss, as well as for the increase in social recognition. This leads to a decrease in anxiety and fear of social interaction, as well as the appearance of new positive plans for the future [13,37-38].
Regarding patient rejection, our data are at the lower limit of those described by Sarwer et al. [13], who establishes a percentage of rejection between 3% and 20% for psychiatric reasons. In our case, the low percentage of excluded patients can also be explained because the most of our patients have already undergone a previous assessment by their zone mental health unit, although they are assessed again at the UMAIO with a specific protocol to unify the assessment of all patients from the different health zones; by the scarce presence of patients with psychoactive substance abuse in the sample, that is one of the primary reasons for exclusion [12]; and also because the patients having psychiatric pathologies are being treated by mental health services, which allows for a stabilization of the symptoms that do not contraindicate BS. Thirteen percent of the patient candidates were in treatment by their mental health unit of reference, and if we add the 2.5% of excluded patients, we find that 15.5% of the sample is in treatment due to mental health.
The uses of substances among our patients were equally very low. It is possible that these low levels can be explained by the mentioned previous assessment by their mental health unit of reference, and the presence of high social desirability, given the patients’ interest in presenting a good image of them to be included in the UMAIO surgical program.
The use of an incidental sample, although representative, may be considered a limitation of this study.
Conclusion
According our results, we feel that it is important to delve deeper into the influence that psychological variables have upon the medium and long-terms results of BS, in order to protocolize systematically models and assessment instruments. Finally, we have found a differential psychosocial profile for women, and we think it can be taken into account to design and implement specific programs of BS preparation and follow-up. As part of that team, psychiatrists and psychologists can formulate specific recommendations and provide feedback that may significantly improve the probabilities for success after surgery.
References
- Snyder AG. Psychological Assessment of the patient undergoing bariatric surgery. Ochsner J. 2009;9(3):144-8.
- Van Hout G, Van Heck G. Bariatric psychology, psychological aspects of weight loss surgery. Obes Facts. 2009;2(1):10-15.
- Heinberg LJ, Ashton K, Windover A. Moving betond dichotomous psychological evaluation: the Cleveland Clinic Behavioral Rating System for weight loss surgery. Surg Obes Relat Dis. 2010;6:185-90.
- Pull B. Current psychological assessment practices in obesity surgery programs: what to assess and why. Curr Opin Psychiatry. 2010;23:30-6
- Devlin MJ. Surgical management of obese patients with eating disorders: a surve of current practice. Obes Surg. 2004;14:252-7.
- Bauchowitz AU, Gonder-Frederick LA, Olbrisch ME, et al. Psychosocial evaluations of bariatric surgery candidates: a survey of present practices. Psychosom Med. 2005;67:825-32.
- Fried M, Hainer V, Basdevant A, et al. Inter-disciplinary European guidelines on surgery of severe obesity. Int J Obes. 2007;31:569-77.
- Caicoya MJ. Evaluación psiquiátrico-psicológica. In Martin A, Díaz del Val I. Cirugía de la obesidad mórbida. Madrid: Aran Ediciones. 2007:135-41.
- Mechanick JI, Kushner RF, Sugarman HJ, et al. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic and Bariatric Surgery Medical. Guidelines for Clinical Practice for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient. Endocr Pract. 2009;17:S1-S70.
- Melissas J. IFSO Guidelines for Safety, Quality, and Excellence in Bariatric Surgery. Obes Surg. 2008;18:497-500.
- De la Viuda Suárez ME, Costa Trigo R, Coto Lesmes R. Análisis de variables psicológicas en un grupo de pacientes candidatos a cirugía bariátrica. Bariátrica & Metabólica Ibero-Americana. 2016;6(2):1014-23.
- Grothe KB, Dubbert M, O`Jile JR. Psychological assessment and management of the weight loss surgery patient. Am J Med Sci. 2006;4:201-6.
- Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obes Res. 2005;13:639-48.
- Sogg S, Mori DL. The Boston interview for gastric by-pass: determining the psychosocial suitability of surgical candidates. Obesity Surgery. 2004;14:370-80.
- Ruiz MA, Berrocal C, Valero L. Cambios psicológicos tras cirugía bariátrica en personas con obesidad mórbida. Psicothema. 2002;14(3):577-82.
- Pérez J, Gastañaduim MJ. Valoración psicológica y psiquiátrica de los candidatos a cirugía bariátrica. Papeles del Psicólogo. 2005;90:10-14.
- Luján JA, Parrilla P. Selección del paciente candidato a cirugía bariátrica y preparación preoperatoria. Cir Esp. 2004;75(5):232-5.
- Pérez E, De la Torre M, Tirado S, van-der Hofstadt C. Valoración de candidatos a cirugía bariátrica: descripción del perfil sociodemográfico y variables psicológicas. Cuadernos de Medicina Psicosomática y Psiquiatría de Enlace. 2011;99:29-34.
- Black DW, Goldstein RB, Mason EE. Psychiatric diagnosis and weight loss following gastric surgery for obesity. Obes Surg. 2003;13:746-51.
- Greenberg I, Perna F, Kaplan M, Sullivan MA. Behavioral and Psychological Factors in the Assessment and treatment of Obesity Surgery Patients. Obes Res. 2005;13:244-9.
- Mahoney D. Psychological gender differences in bariatric surgery candidates. Obes Surg. 2008;18:607-610.
- Martín MJ, Messeguer C. Análisis de variables psicopatológicas y demográficas en una población de pacientes remitidos para valoración psiquiátrica previa a cirugía de obesidad mórbida. Cuadernos de Psicosomática y Psiquiatría de Enlace. 2008;86-87:52-9.
- Van-der Hofstadt C, Tirado S, Escribano S, et al. Changes in quality of life in patients undergoing bariatric surgery. Bariátrica & Metabólica Ibero-Americana. 2016;6(1):954-61.
- Fabricatore AN, Crerand CE, Wadden TA, et al. How do mental health professionals evaluate candidates for bariatric surgery? Survey results. Obes Surg. 2006;16:567-73.
- Herpetz S, Kielmann R, Wolf AM, et al. Do psychosocial variables predict weight loss or mental health after obesity surgery? A systematic review. Obes Res. 2004;12:1554-69.
- Van-der Hofstadt C, Pérez E, Tirado S, et al. Psychological effects of a structured program for preparing bariatric surgery patients. Ansiedad y Estrés. 2012;18(2-3):231-9.
- Aubert N, Lyon-Pagès I, Carrard I, et al. The predictive value of psychological assessment of candidates for gastric bypass: A medical chart review. Eur J Psychiat. 2010;24(2):114-23.
- Van-der Hofstadt CJ, Pérez E, Abad AL, et al. Programa multidisciplinar de intervención grupal pre cirugía bariátrica. Cuadernos de Psicosomática y Psiquiatría de Enlace. 2010;93-94:34-44.
- Seisdedos M. STAI. Cuestionario de Ansiedad Estado-Rasgo. Adaptación Española. Madrid: TEA; 1988.
- Conde V, Useros E. Adaptación castellana de la Escala de Evaluación Conductual para la Depresión de Beck. Rev Psiquiatr y Psicol Med Eur Am Lat. 1975;12:217-36.
- Garner DM, Olmsted MP, Polivy J. Development and validation of a multidimensional Eating Disorder Inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2:15-34.
- Garner DM. Eating Disorder Inventory-2 (EDI-2). Madrid: TEA Ediciones. 1998.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. ed., Hillsdale, N.J., Erlbaum; 1988.
- Calderón C, Forns M, Varea V. Obesidad infantil: ansiedad y síntomas cognitivos y conductuales propios de los trastornos de alimentación. An Pediatr (Barc). 2009;71(6):489-94.
- Britz B, Siegfried W, Ziegler A, et al. Rates of psychiatric disorders in a clinical study group of adolescents with extreme obesity and in obese adolescents ascertained via a population based study. Intl J Obes. 2000;24:1707-14.
- Martin LF. The biopsychosocial characteristics of people seeking treatment for obesity. Obesity Surgery. 1999;9:235-43.
- Dixon JB, Dixon ME, O`Brien PE. Depression in association with severe obesity: changes with weight loss. Arch Int Med. 2003;163:2058-65.
- Malone M, Alger-Mayer S. Binge status and quality of life after gastric by-pass surgery: a one year study. Obes Res. 2004;12:473-81.