- Biomedical Research (2010) Volume 21, Issue 3
Psychometric properties of depression in university students of Turkey
K. Ongel1*, H. Mergen2, S. Tan3, A.N. Kisioglu4, E. Katırcı5, D. Cadırcı6, B.K. Arslan1, T. Gurbuz1 and N. Gumral71Suleyman Demirel University Faculty of Medicine, Department of Family Medicine, Isparta, Turkey.
2Uludag University Faculty of Medicine, Bursa, Turkey.
3Uludağ University Faculty of Education, Department of Measurement & Assessment, Bursa, Turkey.
4Suleyman Demirel University Faculty of Medicine, Department of Rural Health, Isparta, Turkey.
5Aglasun Goverment District Hospital, Burdur, Turkey.
6Yazıhan Goverment District Hospital, Malatya, Turkey.
7Suleyman Demirel University Faculty of Medicine, Department of Physiology, Isparta, Turkey.
- *Corresponding Author:
- Dr. Kurtulus Ongel
Suleyman Demirel University
Faculty of Medicine
Department Head of Family Medicine
32240 Cunur-Isparta Turkey
Accepted Date: March 31 2010
Abstract
It is aimed to utilize a factor model for Beck Depression Inventory-II (BDI-II) and Zung Self-depression Scale (SDS) and to compare which scale is more decisive in gradation of depression for our study group. In addition, the depression prevalence in the mentioned population was detected. In January 2008, 83 medical faculty freshmen in Suleyman Demirel University Faculty of Medicine have been included in the study. Beck Depression Inventory- II Turkish translation (BDI-II-T) and Zung Self-depression Scale Turkish translation (SDST) were applied simultaneously to subjects. Bivariate correlation tests were used for comparison of item score versus total score. Student’s t test was used for imposing sexual differences. Kaiser-Meyer-Olkin measure of sampling adequacy and Bartletts test of sphericity, principal component analysis and varimax rotation were used for factor analysis. The number of students taking part in the research was 83. 42.2% of whom were male and 57.8% female. Mean age was 18.5±0.89. 3 factors [factor 1(depressive), factor 2 (negative attitudes towards self), factor 3(somatic)] for BDI-II and 3 factors [factor 1(depressive), factor 2 (anxiety), factor 3 (somatic)] for SDS were found to be interpretable. Between two tests; correlation was found for total test scores, but an inverse association was found for item scores (d:0.027, p:0.014, r:0.503). According to BDI-II-T; moderate depression ratio was 50.6%, serious depression was 42.2% and very serious depression was 7.2%. According to SDS-T, ratios were 25.3%, 12% and 1.2%. BDI is proper to assess severity of depressive symptoms. Moreover, SDS is an excellent screening test in the outpatient setting.
Keywords
Depression, Scale, Factor analyse.
Introduction
Depression is a common mood disorder affecting many peoples lives by profoundly disturbing their daily functions for many years. According to World Health Organization (WHO) data, globally it is still a prevalent condition and a leading cause of decreased quality of life and increased mortality [1]. Although, it is seen in both genders, especially in their life time 20% of all women are affected by this illness [2].
The Diagnostic and Statistical Manual of Mental Disorders 4th. Ed. (DSM-IV) labels depressive disorders as a cluster of mood disorders and categorizes it under 4 groups: a) major depressive disorder, b) dysthymic disorder, c) depressive disorder and d) not otherwise specified [3]. Among those, major depressive disorder is the most severe and life treating group and occurs in 2-4% of people in the community, in 5-10% of primary care patients and 10%-14% of medical inpatients [4].
It is challenging for physicians to classify and label patients with varying degrees of depression by using only intervention techniques. It is suggested that diagnostic tools can assist physicians to predict the depression prevalence in randomly selected samples. These scales not only enable physicians to save time and effort but they also play a significant role in the accuracy of diagnoses [5]. Even though there are numerous scales; during the past three decades, Beck Depression Inventory (BDI) has become the most widely used self-report instrument for measuring depressive symptom severity in both research and clinical settings [6]. Another important scale; Zung Self-Rating Depression Scale (SDS) is not very useful in the research or inpatient setting [7].
Beck Depression Inventory was first developed by Beck et al. in 1961 (BDI-I) and revised in 1996 (BDI-II) [8,9]. Reliability and validity of Turkish translation of BDI-II (BDI-II-T) was conducted by Hisli [10]. The Zung Self- Rating Depression Scale (SDS) was developed by Zung in 1965 [11] and was improved by Hedlund and Vieweg in 1979 [12]. A scale is unidimensional if all its items measure one common latent factor. This is important for the unambiguous interpretation of a scale and has the practical advantage that scale scores can consist of summed item scores. It is therefore important to examine which factors underlie the scale and whether each factor can be measured with a unidimensional subset of items [13].
Many studies suggest that adolescents and college students are the main two groups that suffer from some degrees of depression [14-16]. In this study two primary purposes were explored:
1. to utilize a factor model for BDI-II and SDS scales that fits our data well.
2. to compare and predict which scale is more decisive in gradation of depression for our study group.
3. to find out the prevalence of depression in the mentioned population.
Methods
In January 2008, first year students of Süleyman Demirel University Faculty of Medicine (n:96) contributed to the study. All these students were informed about the study orally. 83 students volunteered and accepted to take part in the study by their own consents (participation rate: 86.45%). Subjects were applied concurrently BDI-II-T and Turkish translation of SDS (SDS-T). Besides; students were asked to fill up a questionnaire enquiring sociodemographic characteristics and their families’ psychological backgrounds.
In the assessment of BDI-II-T, each item are scored 0 to 3. Maximum score that one can get for BDI-II-T is 63. According to Burns classification [17]; points between 11-16 are accepted as mild depression; points between 17-29 are accepted as borderline/moderate depression; points between 30-39 are named as serious depression and points over 40 are called as very serious depression.
In the assessment of SDS-T, each item are scored 1 to 4. Maximum score that one can get for SDS-T is 80. This score, later, is converted to 100. Therefore; points between 50-59 are considered as minimal/mild depression; points between 60-69 are called as moderate/marked depression; points over 70 are named as serious depression [18] .
Because cross-cultural validity and reliability of BDI-II-T and SDS-T in Turkish population were proved [10], translation and back-translation of both tests were not performed. Related with clinical depression; cut-off value was 17 for BDI-II-T [11] and 50 for SDS-T [12] in Turkish population. Therefore; in the study these values were accepted as the reference assessment rates.
Data were computed and analyzed by Statistical Package for the Social Sciences (SPSS 16.0, Chicago, IL) statistical programe. Numerical data were expressed as means ± standard deviations (SD) and percentages. Bivariate correlation tests were used for comparison of item score versus total score. Student’s t test was used for imposing sexual differences. Kaiser-Meyer-Olkin measure of sampling adequacy and Bartlett’s test of sphericity, principal component analysis and varimax rotation were used for factor analysis. P-value less then 0.05 and for varimax rotated iterated principal factor analysis, values greater than 0.40 for item weights were considered statistically significant.
Results
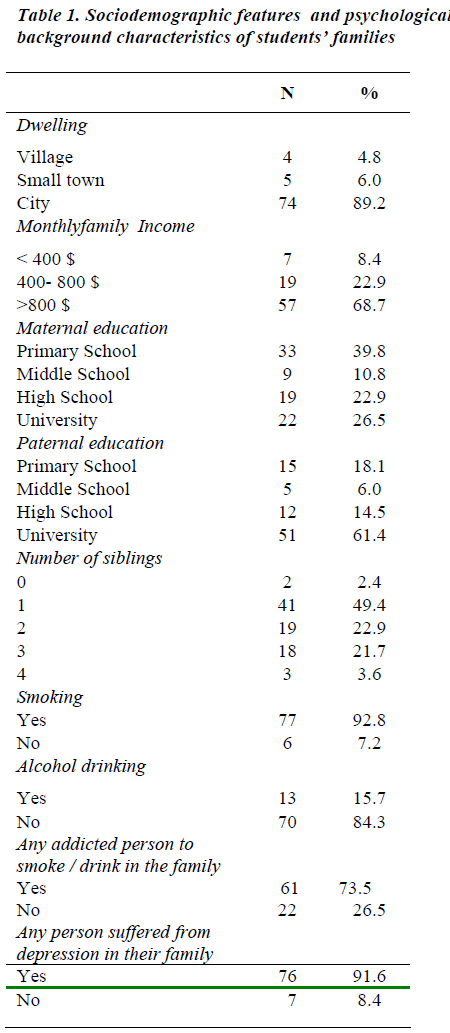
The number of students taking part in the research was 83. 42.2% of whom were male and 57.8% female. Their average age was 18.5±0.89. Dissociation of the research group according to sociodemographic features and psychological characteristics of their families were given in Table 1.
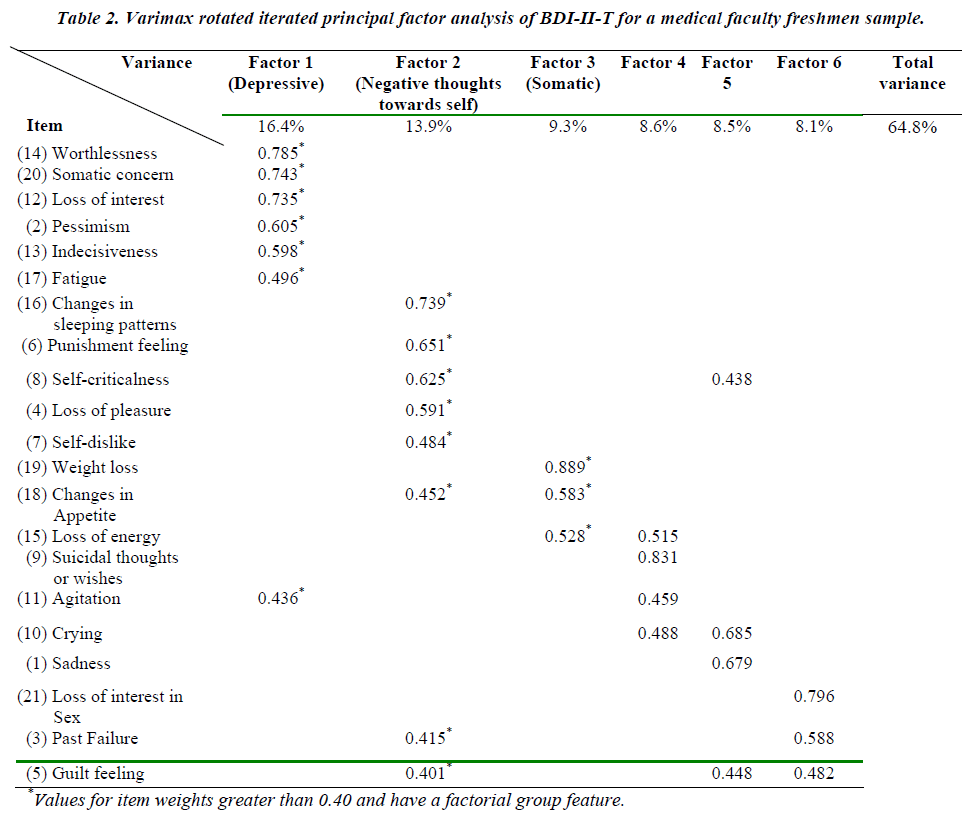
For BDI-II-T; α Cronbach was 0.875, Kaiser-Meyer- Olkin measure of sampling adequacy was 0.768 and Bartlett’s test of sphericity (p=0.000) allowed us to do factor analysis. With principal component extraction and varimax rotation method with Kaiser Normalization, we found 6 factors. After the rotation, the eigenvalues over 1 were found as 3.439, 2.925, 1.966, 1.797, 1.787 and 1.705. Among these 6 factor weights, 0.40 was considered as criteria value. According to this criteria value, only 3 factors [factor 1(depressive), factor 2(negative attitudes towards self) and factor 3(somatic)] were found to be interpretable. Other factors were found dispersedly related to this main factors. Totally explained variance was 64.8%. Factor loads of factor 1,2 and 3 were respectively 16.4%, 13.9% and 9.3% of total variance. Varimax rotated iterated principal factor analysis of BDI-II-T was given on table 2.
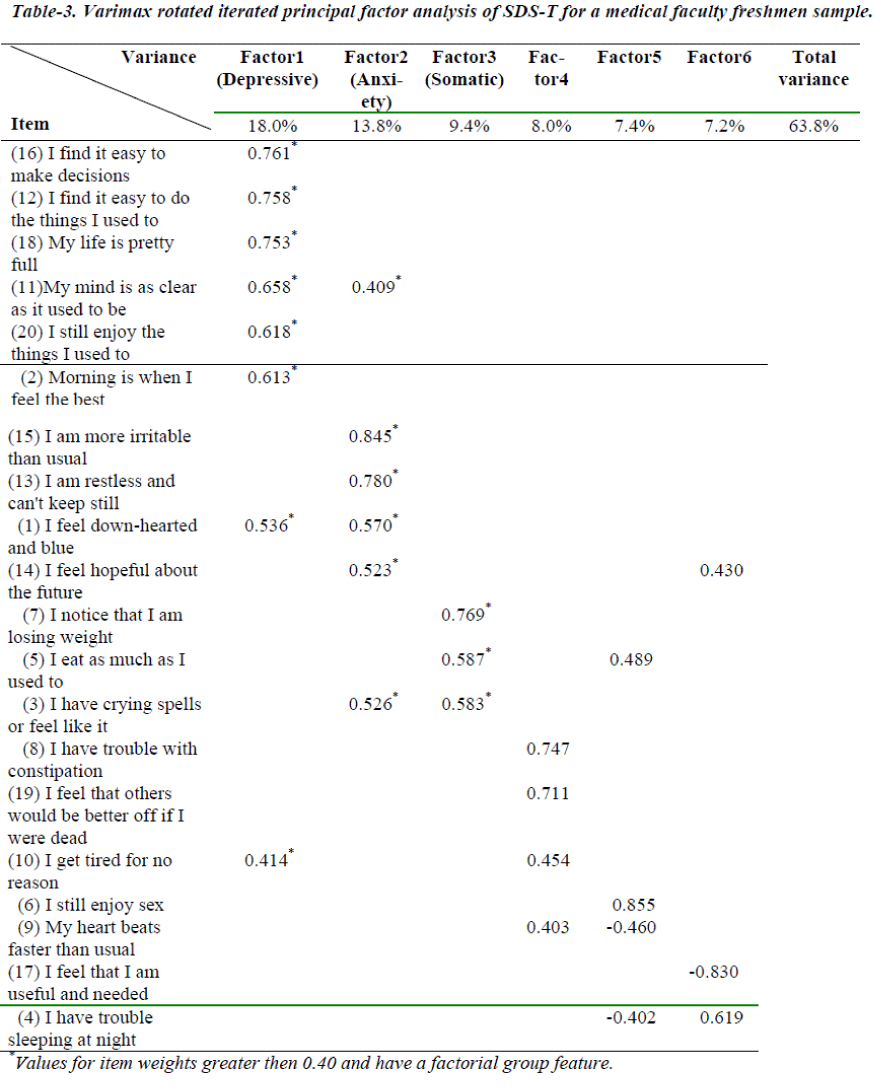
For SDS-T; α Cronbach was 0.779, Kaiser-Meyer-Olkin measure of sampling adequacy was 0.726 and Bartlett’s test of sphericity (p=0.000) allowed us to do factor analysis. With principal component extraction and varimax rotation method with Kaiser Normalization, we have found 6 factors. After the rotation, the eigenvalues over 1 were found as 3.598, 2.767, 1.887, 1.609, 1.481 and 1.441. Among these 6 factor weights, 0.40 was considered as criteria value. According to this criteria value, only 3 factors [factor 1(depressive), factor 2 (anxiety) and factor 3(somatic)] were found to be interpretable. Other factors were found dispersedly related to this main factors. Totally explained variance was 63.8%. Factor loads of factor 1, 2 and 3 were respectively 18%, 13.8% and 9.4% of total variance. Varimax rotated iterated principal factor analysis of SDS-T was given on Table 3.
For BDI-II-T, correlation was found between item score and total test score (p=0.000) (correlation coefficient r varied from 0,180 to 0,698). Likewise, for SDS-T, correlation was found (p<0.05) between item score and total test score except 4th and 9th items. (correlation coefficient r varied from 0,246 to 0,779). Despite the correlation between total test scores of the two tests, an inverse association was found to be between item scores of the two tests (d:0.027, p:0.014, r:0.503).
When the items for both of the tests were analyzed; these items were found to be significant (it means these items are harmonious); sadness (first item of both tests) (p<0.01); satisfaction (item no.4 of BDI-II-T and item no.20 of SDS-T) (p<0.01); self-accusation (item no.8 of BDI-II-T and item no.2 of SDS-T, item no.8 of BDI-II-T and item no.17 of SDS-T) (respectively, p=0.04 and p=0.05); suicidal wish and thoughts (item no.9 of BDI-IIT and item no.19 of SDS-T); crying (item no.10 of BDIII- T and item no.3 of SDS-T) (p<0.01); nervousness (item no.12 of BDI-II-T and item no.18 of SDS-T) (p<0.01); difficulty on giving decision (item no.13 of BDI-II-T and item no.11 of SDS-T) (p<0.01); sleeping problem (item no.16 of BDI-II-T and item no.4 of SDS-T) (p<0.01); fatigue (item no.17 of BDI-II-T and item no.10 of SDST); appetite change (item no.19 of BDI-II-T and item no.7 of SDS-T) (p<0.01).
Insignificant items (it means these items are discordant; p>0.05) were: hopelessness (item no.2 of BDI-II-T and item no.14 of SDS-T); difficult working (item no.15 of BDI-II-T and item no.11 and item no.12 of SDS-T) and sexual problems (item no.21 of BDI-II-T and item no.6 of SDS-T).
All of the 83 subjects were found to be depressed in different grades by BDI-II-T. (moderate depression 50.6%, serious depression 42.2%, very serious depression 7.2%). Meanwhile; 32 students (38.5%) were found to be depressed by SDS-T. (mild depression 25.3%, moderate depression 12%, serious depression 1.2%).
Discussion
The first purpose of the study was to utilize a factor model for BDI-II and SDS that fits our data; 3 factors [factor 1(depressive), factor 2(negative attitudes towards self), factor 3(somatic)] for BDI-II and 3 factors [factor 1(depressive), factor 2(anxiety), factor 3(somatic)] for SDS were found to be interpretable. However; different outcomes obtained from various studies were summarized below.
The study wherein cross-cultural validity of BDI-II was assessed in Japan, internal consistency α Cronbach found as 0.87. In the factor analysis, 2 factors (cognitive and somatic-affective) were found significant [19]. In another study that validity test for BDI-II was carried out in Brazil, internal consistency was found as 0.82 and 2 factors (cognitive-affective and somatic) were found as principal components [20]. Again; among Brazilian college students internal consistency of BDI-II was found as 0.86 and 3 factors (low self-esteem, cognitive-affective and somatic factors) were determined in factor analysis [21]. In another study wherein BDI-II Spanish version was implemented to 292 outpatients; internal consistency, α Cronbach was found 0.89. Factor analysis indicated 4 factors (somatic, sadness/hopelessness, low self-esteem and negative thoughts) [22]. In the study wherein reliability and validity analysis of BDI-II translated to Persian was assessed, internal consistency α Cronbach was found as 0.87 and test-retest correlation (r=0.74). In the factor analysis, affective-cognitive and somatic-vegetative factors were significant [23]. In the study carried out in San Antonio, internal consistency of BDI-II α-Cronbach found as 0.92. In the factor analysis; somatic and cognitive- affective factors were obtained [24].
In a study in primary care setting where SDS was applied to 1049 patients, mild depression rate was found to be 17.6%, moderate depression 33.8% and severe depression 44.5%. Factor analysis of SDS determined 4 factors [factor 1(depressive), factor 2(cognitive), factor 3(anxiety), factor 4 (somatic)]. They excluded two items from scales because of low factor loadings [25]. In a study in Japan; SDS was distributed to 28,588 first-year university students and factor analysis using Promax rotation revealed three factors interpretable as affective, cognitive, and somatic symptoms [26]. In a study that use SDS for screening cancer patients; a four-factor solution emerged, consisting of a cognitive symptom factor, a manifest depressed mood factor, and two somatic factors (eating and non-eating related)[27].
These differences can be associated with the particular features of the study group. Study group was consist of young medical faculty freshmen who succeeded lots of difficult examinations for our country and has high level of education. Thus, we can foresight that factor analyse mustn’t be evaluated just according to countries; at the same time, the other factors like educational status must taken into account.
In the studies from literature; cognitive, affective and somatic factors were found to be the main factors for BDI-II. Dissimilarly; ‘negative attitudes towards self’ was found to be an important factor group in our study. This situation can be related with the young population of the study group who mostly, give importance to physical appearance.
The second purpose of the study was to compare and decide which scale was more decisive in gradation of depression for our study group. when the internal consistency of BDI-II-T and SDS-T were analyzed by α- Cronbach , no statistically significant difference was found between two tests (p>0.01). Despite the correlation between total test scores , an inverse association was found between item scores of the two tests (d:0.027, p:0.014, r:0.503). Likewise, in Tulane University Medical Center wherein BDI-II and SDS were administered to psychiatric patients; both tests showed good correlation (p<0.001). When the depression scores compared, only SDS significantly differentiated the depressive group (F=12.51, p<0.001) [28].
As a result, all of the 83 subjects were found to be depressed in different grades by BDI-II-T (moderate depression 50.6%, serious depression 42.2%, very serious depression 7.2%). Moreover, according to SDS-T, 61.5% of the same students were determined as normal. It is agreed that BDI-II-T is more decisive in gradation of depression than SDS-T.
Conclusion
BDI is probably the widest used self-report measure to assess severity of depressive symptoms in major research studies [29]. Moreover, SDS is an excellent screening test in the outpatient setting, especially for use by nonpsychiatric physicians [7].
References
- Demyttenaere K, Bruffaerts R, Posada-Villa, Gasquet I, Kovess V, Lepine JP et al. Prevalence, severity, and unmet need for treatment of mental disorders in the world health organization: World mental health surveys. JAMA 2004; 292: 2581-2590.
- Sangeeta S, Sanjay V, Singh PN, Gaur RK. Serotonergic influence on the levels of prolactin in depressed females. Biomed Res 2008; 19 (1): 45-48.
- American Psychiatric Association. The diagnostic and statistical manual of mental disorders. 4th ed. Skyscape 1994.
- Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry 1992; 14 (4): 237- 247.
- Mergen H, Mergen BE, Tan S, Ongel K. Evaluating depression and related factors among the students of the faculty of education at Celal Bayar University. The New Journal of Medicine 2008; 25 (3): 169-173.
- Mergen H, Ongel K. Factors associated with depression among Turkish faculty of education freshmen by Beck depression inventory-II-Turkish. Zdravniski Vestnik 2009 Nov; 78: 548-554.
- Gold MS, Pottash ALC. Diagnostic and Laboratory Testing in Psychiatry: Critical Issues in Psychiatry. Plenum Publishing Corporation. New York: 1986; 174.
- Beck AT, Ward C, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry 1961; 4: 561-571.
- Beck AT, Steer RA, Brown GK. Beck depression inventory- Second edition manual. San Antonio (TX): The Psychological Corporation 1996.
- Hisli N. Beck depresyon envanterinin üniversite ögrencileri için geçerliligi ve güvenilirligi. Psikoloji Derg 1989; 7 (23):3-13.
- Zung W. A self-rating depression scale. Arch Gen Psychiatry 1965; 12: 63-70.
- Hedlund JL, Vieweg BW. The Zung self-rating depression scale: A comprehensive review. J of Operational Psych 1979; 10: 51-64.
- Vanheule S, Desmet M, Groenvynck H, Rosseel Y, Fontaine J. The Factor Structure of the Beck Depression Inventory-II. Assessment 2008; 15
- Klomek AB, Marrocco F, Kleinman M, Schonfeld IS, Gould MS. Peer victimization, depression and suicidiality in adolescents. Suicide Life Threat Behav 2008; 38 (2): 166-180.
- Thurber S, Snow M, Honts CR. The Zung self-rating depression scale: Convergent validity and diagnostic discrimination. Assessment 2002; 9 (4): 401-405.
- Kim YS, Koh YJ, Leventhal B. School bullying and suicidal risk in Korean middle school students. Pediatrics 2005; 115 (2): 357-363.
- Burns DD. Feeling Good. The New Mood Therapy. New York. Morrow.1980.
- Tavakoli-Tabasi S, Rowan P, Abdul-Latif M, Kunik ME, El-Serag HB. Utility of a depression score to predict candidacy for hepatitis C virus therapy in veterans: a prospective longitudinal study. Alimentary Pharmacology & Therapeutics 2005;21 (3):235-242.
- Kojima M, Furukawa TA, Takahashi H, Kawai M, Nagaya T, Tokudome S. Cross-cultural validation of the Beck Depression Inventory-II in Japan. Psychiatry Res 2002; 110(3): 291-299.
- Wang YP, Andrade LH, Gorenstein C. Validation of the Beck Depression Inventory for a Portuguesespeaking Chinese community in Brazil. Braz J Med Biol Res 2005; 38 (3): 399-408.
- Gorenstein C, Andrade L, Vieira Filho AH, Tung TC, Artes RI. Psychometric properties of the Portuguese version of the Beck Depression Inventory on Brazilian college students. J Clin Psychol 1999; 55 (5): 553-562.
- Azocar F, Areán P, Miranda J, Muñoz RF. Differential item functioning in a Spanish translation of the Beck Depression Inventory. J Clin Psychol 2001; 57 (3): 355-365.
- Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persianlanguage version of the Beck Depression Inventory Second Edition: BDI-II Persian. Depress Anxiety 2005; 21(4):185-192.
- Osman A, Barrios FX, Gutierrez PM, Williams JE, Bailey J. Psychometric properties of the Beck Depression Inventory-II in nonclinical adolescent samples. J Clin Psychol 2008; 64 (1): 83-102.
- Romera I, Delgado-Cohen H, Perez T, Caballero L, Gilaberte I. Factor analysis of the Zung self-rating depression scale in a large sample of patients with major depressive disorder in primary care. BMC Psychiatry 2008; 8: 4.
- Kitamura T, Hirano H, Chen Z, Hirata M. Factor structure of the Zung Self-rating Depression Scale in first-year university students in Japan. Psychiatry Res. 2004;128 (3):281-287.
- Passik SD, Lundberg JC, Rosenfeld B, Kirsh KL, Donaghy K, Theobald D, et al. Factor analysis of the Zung Self-Rating Depression Scale in a large ambulatory oncology sample. Psychosomatics 2000;41(2):121-127
- Griffin PT, Kogut D. Validity of orally administered Beck and Zung Depression Scales in a state hospital setting. J Clin Psychol 1988; 44 (5): 756-759.
- Nezu AM, Ronan GF, Meadows EA, McClure KS. Practitioner?s Guide to Empirically Based Measures of Depression: AABT Clinical Assessment Series. Kluwer Academic/Plenum Publishers. New York: 2003; 31.