Case Report - Current Pediatric Research (2019) Volume 23, Issue 3
Pseudoprecocious puberty associated with adrenocortical tumor in young child: A Case report.
Shahd E Kafi1, Eid Abdulmoein Al-Agha1*, Mohamed Abdel-Maksoud Shazly2, Abdulmoein E Al-Agha31Department of Pediatric Endocrinology, King Abdulaziz University Hospital, Saudi Arabia
2Department of Pediatrics, King Abdulaziz University Hospital, Saudi Arabia
3Department of General Paediatrics, King Abdulaziz University Hospital, Saudi Arabia
- *Corresponding Author:
- Yavisheva TM
Department of General Paediatrics
King Abdulaziz University Hospital
Saudi Arabia
Tel: 0096664083061
E-mail: aagha@kau.edu.sa
Accepted Date: October 3rd, 2019
Abstract
Precocious puberty presents commonly in pediatric practice due to different causes including adrenal tumors. Adrenocortical tumors are rare in children, characterized by androgenic hormonal excess causing pseudoprecocious puberty. We present a 4-year-old boy, with history of penile enlargement, associated with growth of pubic hair, facial acne, and advanced bone age by 3 years. His hormonal assays were confirming diagnosis of Pseudoprecocious puberty. Abdominal magnetic resonance imaging revealed a right-sided retroperitoneal well-defined adrenal tumor. This case report emphasizes the aim to increase the awareness of adrenocortical tumor as a rare cause of pseudoprecocious puberty in young children.
Keywords
Adrenal tumor, Young children, Pseudoprecocious, Puberty
Introduction
Adrenocortical tumors (ACT) are rare in childhood, which could be seen at any age [1]. First case of childhood ACT was reported in 1865 [2]. Although ACT is a rare neoplasm, its account for about 0.2% of all tumors affecting children and approximately 6% of all adrenal tumor seen in pediatric group [3]. The annual incidence of ACT in children under 15 years of age is an extremely rare ranging from 0.3-0.5 cases per million [4]. However, incidence are variable across various geographical regions, for example in the United States and Europe its accounts about 0.3-0.38 cases per million [4,5]. In comparison to a higher incidences in Brazil of 10-15 times more cases diagnosed than were in worldwide [6,7]. Syndromes reported with ACT were seen in almost 50% of the cases included two main syndromes, Li-Fraumeni syndrome resulted from alterations of the tumor suppressor gene p53 in chromosome 17 and Beckwith-Weidman syndrome from the effect of the region located in 11p15 [2,8,9]. ACT are categorized as either functional (hormone-secreting) which is most commonly seen in children and adolescents or nonfunctional (silent) tumor which is usually found in adults with symptoms of abdominal discomfort or back pain caused by the large mass effect of the tumor [10,11]. They could be benign or malignant tumors [3]. The most common clinical presentation of ACT in children is pseudo-precocious puberty seen in approximately 50-84.2% of cases or as Cushing’s syndrome in other remaining cases [12,13]. Malignancy should not be underestimated in this age group [2]. We report A 4- year-old boy who has presented with pseudoprecocious puberty caused by ACT as a rare cause in children.
Case Report
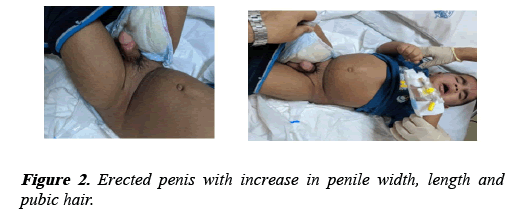
A 4-year-old boy brought to the pediatric endocrinology clinic because of the appearance of pubic hair in conjunction with increase in penile length for the last 2 months. He is a product of full term, vaginal delivery, with uneventful past medical or surgical histories. No family history of endocrine tumors or early puberty. Systemic examinations including vital signs were unremarkable. He had facial acne all over his forehead and cheeks (Figure 1), with no skin hyperpigmentation.
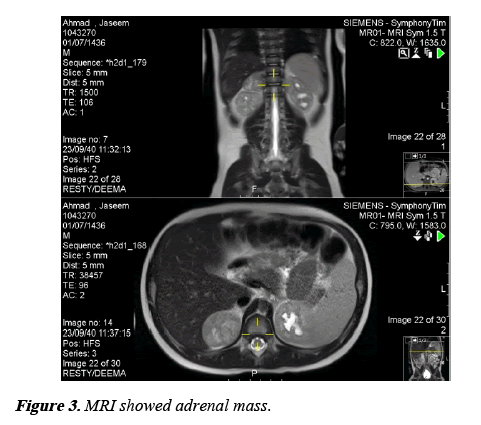
His Tanner staging of both pubic hair and genitalia was stage III. Volume of both testes were of 2 ml and his stretched penile length (SPL) was 7.5 cm (Figure 2). His serum hormonal assays were presented in Table 1, with low basal levels of Follicle-stimulating hormone (FSH), luteinizing hormone (LH) and 17- hydroxyprogesterone, while an elevated levels of testosterone and Dehydroepiandrosterone sulfate (DHEA-S) were revealed. Gonadotropin releasing hormone “ GNRH ” stimulation test showed negative response. Bone age assessment was advanced by 3 years. All of which confirms the diagnosis of pseudoprecocious puberty. Magnetic resonance imaging of the Abdomen revealed a right-sided retroperitoneal adrenal mass (Figure 3). Based on this clinical picture and imaging, the diagnosis of adrenocortical tumor was made.
| Test | Date | Result | |
|---|---|---|---|
| FSH | 17/4/2019 | 0.2 | |
| 18/4/2019 | 0 min | 0.2 | |
| 15 min | 0.4 | ||
| 30 min | 0.3 | ||
| 45 min | 0.4 | ||
| 60 min | 0.3 | ||
| 90 min | 0.5 | ||
| 120 min | 0.6 | ||
| LH | 17/4/2019 | 0.2 | |
| 18/4/2019 | 0 min | 0.2 | |
| 15 min | 0.3 | ||
| 30 min | 0.2 | ||
| 45 min | 0.2 | ||
| 60 min | 0.2 | ||
| 90 min | 0.2 | ||
| 120 min | 0.2 | ||
| testosterone | 17/4/2019 | 39 | |
| 18/4/2019 | 33 | ||
| 17 OH progesterone | 18.8 ng/ml | Normal | |
| Alfa fetoprotein (AFP) | 4.45 ng/ml | normal | |
| beta human chorionic gonadotropin (BHCG) | <1.2 iu/ml | normal | |
Table 1. Showed hormonal assay result.
Discussion
Precocious puberty is defined as the presence of secondary sex characteristics before the age of 8 in girls and 9 in boys. These limits represent 2 to 2.5 standard deviations (SD) below the mean age of the onset of puberty [14]. Precocious puberty have two main types of either central (CPP) - gonadotropin dependent - caused by an early activation of the hypothalamicpituitary- gonadal axis, or pseudoprecocious puberty - gonadotropin independent - results from excess secretion of sex hormones either from the gonads or adrenal glands [15]. There are several causes of pseudoprecocious puberty including adrenal tumors, non-classical congenital adrenal hyperplasia, testicular tumors, germ cell tumors, McCune- Albright syndrome, familial male-limited precocious puberty (testotoxicosis) or exogenous sex steroid hormone usage. Clinical presentations could be markedly suspicious to the types of Precocious puberty as CPP often present with gonadal enlargement either testicular in males or ovarian in females, in contrast to pseudoprecocious puberty which presents mainly with early development of pubic and/or axillary hair. Dynamic stimulating test of the hypothalamic-pituitary-gonadal axis by using of gonadotropin releasing hormone agonist has an essential and golden role in differentiation between the two types of precocious puberty. Pubertal response by increasing hormonal level of luteinizing hormone (LH) and follicular stimulating hormone (FSH) usually seen in CPP, while no response usually confirms pseudoprecocious puberty as seen in this case.
ACT could cause pseudoprecocious puberty by secretion of excess androgenic hormones leading to virilization, which is the most common presenting symptoms of the tumor in childhood; however, late presentation of ACT could be seen with CPP secondary to the maturation of hypothalamicpituitary- gonadal axis. Female children noticed to be more affected than males, with peak age of younger than 4 years [12]. Management of this disease is still challenging because of the limited numbers of reported cases.
Non classical congenital adrenal hyperplasia (NCAH) causes androgen over secretion which lead to pseudoprecocious puberty with the development of earlier signs of puberty, including pubic hair, acne and accelerating skeletal maturation [16], this disease could be detected early in the neonatal period by screening for an elevated serum level of 17- hydroxyprogesterone, however, in this case NCAH was excluded because of the normal levels of 17- hydroxyprogesterone, cortisol and adrenocorticotropic hormone (ACTH). Abdominal MRI finding of unilateral tumor of the right adrenal gland confirms the diagnosis of ACT.
Literature review of case reports revealed that virilization was considered as a good clue for suspecting diagnosis of ACT, similar to the presentation in this case [11,12,13]. Razavi reported a 10 month old boy diagnosed with ACT who presented with sexual pubic hair, acne and seborrhea dermatitis [3]. Another case of a 2 years old Indian boy was presented with pubic hair and penile enlargement [1]. Ghazizadeh reported virilization seen in 2 years old girl associated with ACT in 2013 [17]. However, discriminating benign tumor from malignant is not depending on hormonal secretions. A comprehensive evaluation of precocious puberty including clinical manifestation, laboratory testing and imaging is very important for reaching the final diagnosis.
Conclusion
Virilization of both sexes is an important manifestation of adrenocortical tumors which should be considered as one of the rare causes of Pseudoprecocious puberty. High index of suspicion and increase awareness of pediatricians has important role in early diagnosis and treatment.
References
- Meshram RM, Bhongade S, Patil S, et al. Precocious puberty associated with an adrenal tumor: A case report. American Journal of Medical Case Reports 2016; 4: 354-356.
- Ribeiro RC, Michalkiewicz EL, Figueiredo BC, et al. Adrenocortical tumors in children. Braz J Med Biol Res 2000; 33: 1225-1234.
- Zahra-Razavi MD, Rastgoo-Haghi MD. Precocious puberty associated with an adrenal tumor: A case report. Iran J Ped Hematol Oncol 2016; 6: 136-141.
- Shirata NK, Sredni ST, Castelo A, et al. Texture image analysis in differentiating malignant from benign adrenal cortical tumors in children and adults. Anticancer Res 2009; 29: 3365-3368.
- Ciftci AO, Senocak ME, Tanyel FC. Adrenocortical tumors in children. J Pediatr Surg 2001; 36: 549-554.
- Ribeiro R, Figueiredo B. Childhood adrenocortical tumours. Eur J Cancer. 2004; 40: 1117-1126.
- Figueiredo BC, Sandrini R, Zambetti GP, et al. Penetrance of adrenocortical tumours associated with the germline TP53 R337H mutation. J Med Genet 2006; 43: 91-96.
- Wiedemann HR. Complexe malformatif familial avec hernie umbilicale et macroglossie, un "syndrome nouveau". Journal de Genetique Humaine 1964; 13: 223.
- Li FP, Fraumeni JF, Mulvihil JJ, et al. A cancer family syndrome in twenty-four kindreds. Cancer Research 1998; 48: 5358-5362.
- Faizah M, Zuhanis A, Rahmah R, et al. Precocious puberty in children: A review of imaging findings. Biomed Imaging Interv J 2012; 8: e6.
- Kim SM, Yang EJ, Cho HD, et al. Virilizing adrenocortical carcinoma advancing to central precocious puberty after surgery. Korean J Fam Med 2015; 36: 150-153.
- Michalkiewicz E, Sandrini R, Figueiredo B, et al. Clinical and outcome characteristics of children with adrenocortical tumors: a report from the International Pediatric Adrenocortical Tumor Registry. J Clin Oncol 2004; 22: 838-845.
- Cacciari E, Cicognani A, Pirazzoli P, et al. Adrenocortical tumors in children: Our experience with nine cases. Acta Endocrinol Suppl. (Copenh) 1986; 279: 264-274.
- Faizah M, Zuhanis A, Rahmah R, et al. Precocious puberty in children: A review of imaging findings. Biomed Imaging Interv J 2012; 8: e6.
- Harrington J, Palmert MR. Definition, etiology, and evaluation of precocious puberty. Up-to-date, H266911694.
- Witchel SF, Azziz R. Nonclassic congenital adrenal hyperplasia. International Journal of Pediatric Endocrinology, 2010.
- Ghazizadeh F, Ebadi M, Alavi S, et al. Adrenocortical carcinoma presenting with heterosexual pseudoprecocious puberty shortly after birth: case report and review. Ecancer Medical Science. 2013; 7: 289.