- Biomedical Research (2015) Volume 26, Issue 1
Prognostic value of highly sensitive C-reactive protein and plaque morphology in coronary artery disease in China.
Xing-Wei Zhang1, Jian-Min Yang2*, Ning-Fu Wang2, Xian-Hua Ye2, Liang Zhou2, Guo-Xin Tong2, Hao Pan2, Jian Xu21Hangzhou Cardiovascular Institute, Affiliated Hospital of Hangzhou Normal University, Hangzhou 310015, China
2Department of Cardiology, Hangzhou No. 1 Municipal Hospital and Affiliated Hangzhou Hospital of Nanjing Medical University, Hangzhou 310006, China
- *Corresponding Author:
- Jianmin Yan
Department of Cardiology
Hangzhou No. 1 Municipal Hospital and Affiliated Hangzhou Hospital of Nanjing Medical University
126# Huansha Road, Hangzhou 310006
China
Accepted date: June 07 2014
Abstract
Inflammation contributes to the initiation and progression of coronary atherosclerosis. A highly sensitive C-reactive protein (hs-CRP) can be used as a predictor of future coronary events in healthy populations and in patients with angina. However, the relationship between hs-CRP and coronary lesion characteristics as well as their associations with clinical outcomes in Chinese patients with coronary artery diseases has not been well described. This study aimed to investigate the prognostic value of coronary lesion characteristics and hs-CRP in Chinese patients with coronary artery disease. Coronary lesion characteristics were characterized by intravascular ultrasound. Serum hs-CRP and pro-matrix metalloproteinase-1 (ProMMP-1) concentrations were measured by sandwich enzyme-linked immunosorbent assay in 184 patients. Among these patients, 101 suffered from acute coronary syndrome (ACS) and 83 suffered from stable angina (SA). These patients were followed up for one year to monitor subsequent major adverse cardiac events (MACE). Patients with ACS exhibited an increased external elastic membrane cross-sectional area, plaque burden, lipid pool burden, and remodeling index compared with the patients with SA (P < 0.05). Rupture and vulnerable plaques were more frequently observed in patients with ACS than in patients with SA (40.59% vs. 1.20% and 42.57% vs. 3.61%, respectively; P < 0.001). Serum hs-CRP and proMMP-1 concentrations were higher in patients with ACS (18.17 [6.32, 22.10] mg/L vs. 3.75 [1.86, 4.32] mg/L, P < 0.001 and 1.56 [0.72, 1.82] ng/ml vs. 1.14 [0.75, 1.14] ng/ml, P = 0.012]. Strong associations were found between hs-CRP, proMMP-1 and plaque type. Univariate analysis found that ACS, Troponin I and hs-CRP were associated with MACE, while multivariate logistic regression found that only hs-CRP was independently associated with MACE for one year. An increase in hs-CRP is correlated with rupture and vulnerable plaques. hs-CRP but not plaque morphology is associated with poor prognosis in Chinese patients with coronary artery disease.
Keywords
Coronary artery disease, C-reactive protein, plaque, major adverse cardiac events
Introduction
Inflammation contributes to the initiation and progression of coronary atherosclerosis; this condition may also trigger plaque rupture and thrombosis, which are the common mechanisms of acute coronary syndrome (ACS) [1-4]. In systemic inflammation, C-reactive protein (CRP) functions as a non-specific marker; CRP also accumulates in plaques, impairs endothelial function, and promotes smooth muscle cell proliferation and migration [5-8]. A highly sensitive CRP (hs-CRP) is used as a predictor of future coronary events in healthy populations and in patients with angina [9-12], which may occur by
promoting plaque rupture [13]. Plaque characteristics, such as severe calcification, erosion, and severe stenosis, can be used to predict death, heart failure, and myocardial infarction [14-18]. However, no consensus has been reached based on the opposite results of the prognostic value of hs-CRP in coronary artery disease (CAD) [19-22], so it needs further study to gain a common view on Chineses CAD patients, especially [23]. Therefore, we studied the relationship between hs-CRP, pro-matrix metalloproteinase-1 (ProMMP- 1), and graphical characteristics of coronary artery culprit lesion as well as their associations with major adverse cardiac events (MACE) of coronary artery diseases in Chinese patients for one year.
Subjects and MethodsSubjects and Methods
Patients
A total of 101 patients with ACS and 83 patients with stable angina (SA) were recruited consecutively from inpatients that underwent coronary arteriography and intravascular ultrasound (IVUS). Among the patients with ACS, 78 (77.23%) suffered from non-ST elevation acute myocardial infarction (NSTEMI) and 23 (22.77%) suffered from unstable angina. NSTEMI defined by the presence of symptoms consistent with cardiac ischemia within 24 hours of hospital presentation and troponin I levels above the 99th percentile but not include (a) persistent ST segment elevation of ≥1 mm in two contiguous electrocardiographic leads or (b) the presence of a new or presumably new left bundle branch block. Unstable angina was classified as new onset angina within the previous one month before admission, accelerated pattern of angina, angina at rest, or STsegment depression with normal cardiac biomarkers. SA was defined as no change in frequency, duration, or intensity of symptoms and normal cardiac biomarkers. All SA patients were of classified grade Canadian Cardiovascular Society III-IV or positive stress electrokardiogram test. Exclusion criteria included the following: ST elevation acute myocardial infarction, previous percutaneous coronary intervention; previous coronary artery bypass grafting; chronic occlusion; stenosis of left main artery ≥50%; New York Heart Association Class ≥ III; rheumatic heart disease; infective endocarditis; concomitant systemic inflammatory or autoimmune disease; major operation or external injury within three months; gastrointestinal hemorrhage within two weeks; or concomitant cancer or bleeding disease. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Hangzhou No. 1 Municipal Hospital. Written informed consent was obtained from all participants.
Assessment of hs-CRP and ProMMP-1
Blood samples were collected from the femoral artery before coronary angiography was performed and then stored at -80 °C until assay. Sandwich enzyme-linked immunosorbent assay was performed to determine the following: hs-CRP, with a minimum detectable dose of 1.60 ng/mL (DSL-10-42100Us CRP ELISA Kit, Diagnostic Systems Laboratories, Inc., Webster, USA) and ProMMP-1, with a minimum detectable dose of 0.02 ng/mL (Quantikine human pro-MMP-1, Research & Diagnostics Systems, Inc., Minneapolis, Minnesota, USA).
IVUS imaging and analysis
Coronary angiography was performed using the femoral approach. After intracoronary administering 0.2 mg of nitroglycerin, IVUS examinations (with a 3.2 F, 30 MHz mechanical transducer, Boston Scientific Galaxy I and II, USA) were performed immediately. The culprit vessle examined by IVUS was determined by operators according to the manisfestion of electrokardiogram, stress electrokardiogram test and angiography. The 3 vessels examined only when requested for more evidence. IVUS images were qualitatively and quantitatively analyzed by two independent experienced physicians who were blinded from angiographic and clinical data [24]. The following parameters were measured: external elastic membrane cross-sectional area; minimal lumen crosssectional area; plaque area; plaque burden; lipid pool area; lipid pool burden; and remodeling index.
Remodeling index > 1.05 was classified as positive remodeling and remodeling index < 0.95 was classified as negative remodeling. Plaque morphology was classified into three types: ruptured, vulnerable, and stable plaque. Ruptured plaque was defined as follows: 1) lesions with fissure/dissection or 2) lesions without fissure/dissection; contrast medium injection was performed to demonstrate the communication between plaque and coronary artery lumen. Plaque with lipid pool burden >20% was defined as vulnerable plaque [25, 26].
Patient follow-up period
All of the patients were treated on the basis of standard medications (aspirin and/or clopidogrel, nitrate, angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, β-receptor blocker, and statins). Patients were followed up for one year and recommended for subsequent MACE after coronary angiography. Adverse events were characterized by death, myocardial infarction, and revascularization.
Statistical analysis
The distribution of continuous data was determined using the 1-sample Kolmogorov- Smirnov test. Normally distributed data (presented as mean ± standard deviation [SD]), and non-parametric data (as median and inter-quartile range [IQR]) were compared using the Student's t test and Mann–Whitney U test, respectively. Categorical variables were expressed as frequency percentages and by chi-square statistics. Relationships between hs-CRP, ProMMP-1, and intravascular ultrasound parameters were analyzed by Pearson correlation tests. Baseline patient characteristics, intravascular ultrasound parameters, hs- CRP, and ProMMP-1 were considered for univariate analysis for MACE first, and then the associated index was considered for multivariate logistic regression for MACE. Statistical analysis was performed using SPSS version 15.0 (SPSS Inc., Chicago, Illinois, USA). P < 0.05 was considered statistically significant.
Results
Subject characteristics
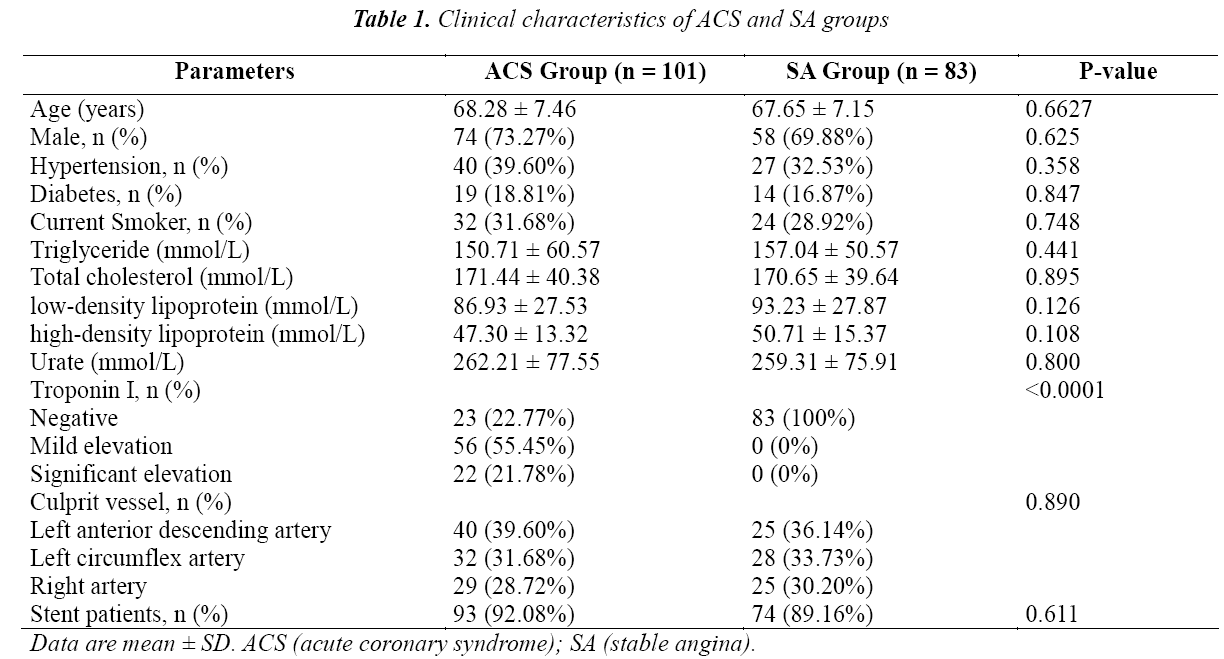
Our study population consisted of 101 patients with ACS and 83 patients with SA. The clinical characteristics are presented in Table 1. Patients with ACS and SA exhibited similar age, gender, current smoking status, and distriour study population consisted of 101 patients with ACS and 83 patients with SA. The clinical characteristics are presented in Table 1. Patients with ACS and SA exhibited similar age, gender, current smoking status, and distribution of culprit vessels. These patients also suffered from adverse diseases, including hypertension, hyperlipidemia, and diabetes. The culprit lesion or vessel was determined according to the manifestation of electrokardiogram, angiography and IVUS results, stents were implanted according the operator`s choice. In both groups, stents were implanted in approximately 90% of the patients.
IVUS Findings
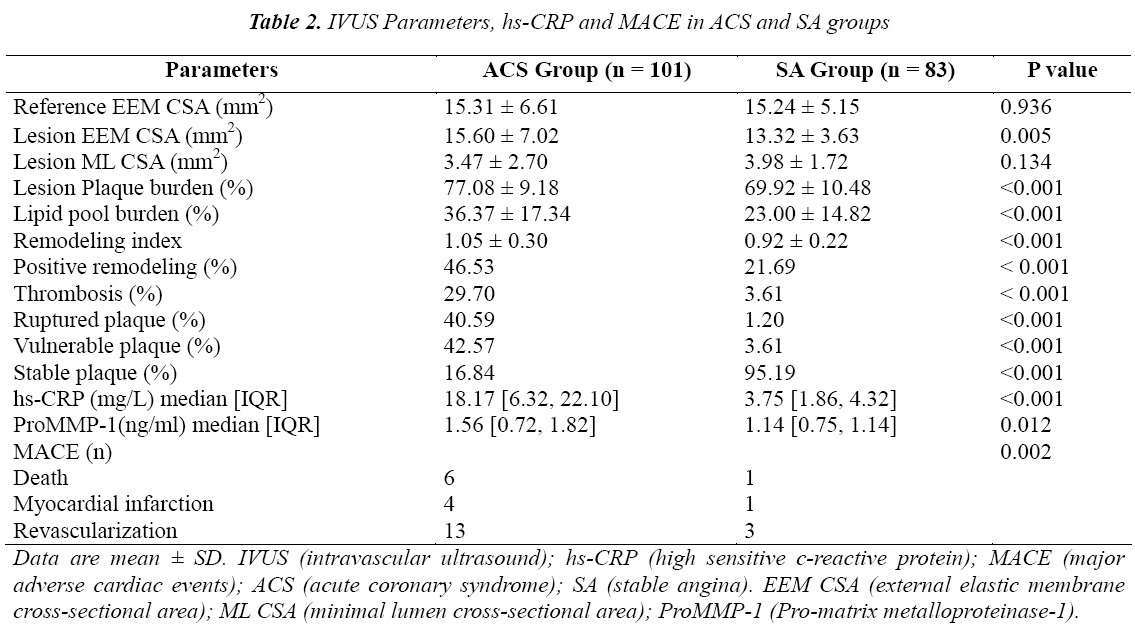
The IVUS parameters are shown in Table 2. Rupture plaques were observed more frequently in the ACS group than in the SA group (40.59% vs. 1.20%; P < 0.001). Similar results were found in vulnerable plaque (42.57% vs. 3.61%; P < 0.001); by comparison, stable plaques were observed more frequently in the SA group (16.84% vs. 95.19%; P < 0.001). The external elastic membrane cross-sectional area [15.60 ± 7.02 mm2 vs. 13.32 ± 3.63 mm2; P = 0.005] and lipid pool burden [36.37 ± 17.34% vs. 23.00 ± 14.82%, P < 0.001] were increased in the ACS group compared with the SA group. Positive remodeling (46.53% vs. 21.69%; P < 0.001) and thrombus (29.70% vs. 3.61%; P < 0.001) were more frequently observed in the ACS group than in the SA group.
Relationship between hs-CRP and IVUS parameters
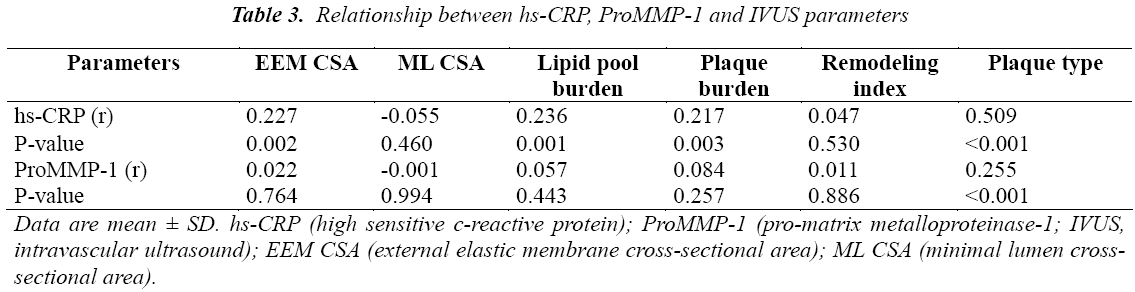
The results of hs-CRP and proMMP-1 are shown in Table 2. hs-CRP concentration in the ACS group was five times higher than that in the SA group (18.17 [6.32, 22.10] mg/L vs. 3.75 [1.86, 4.32] mg/L; P < 0.001). Similar results were found in ProMMP-1 (1.56 [0.72, 1.82] ng/mL vs. 1.14 [0.75, 1.14] ng/mL; P = 0.012). Correlation analysis results showed that hs-CRP was strongly associated with plaque type (r = 0.509, P < 0.001). hs- CRP was also correlated with the external elastic membrane cross-sectional area, lipid pool plaque, and plaque burden (r = 0.227, P = 0.002; r = 0.236, P = 0.001; and r = 0.217, P = 0.003, respectively). No significant association was observed between ProMMP-1 and intravascular ultrasound parameters except plaque type (r = 0.255, P < 0.001). (Table 3).
Patient outcomes
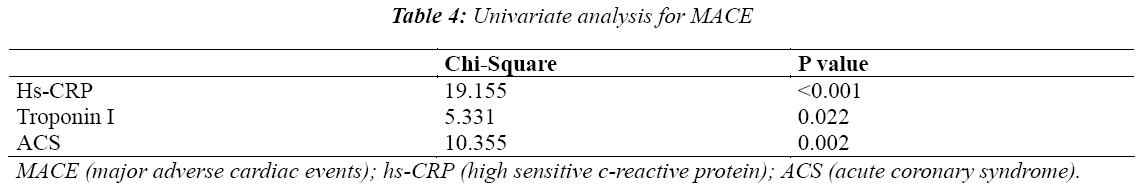
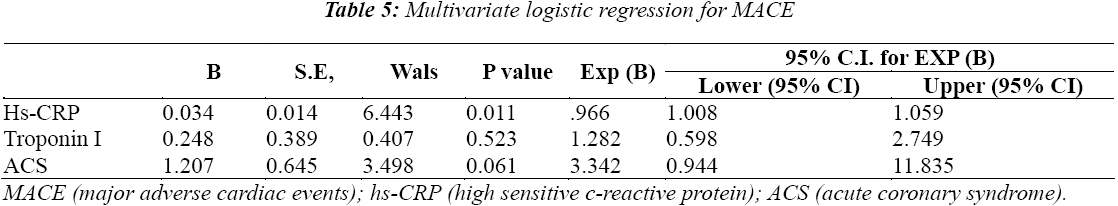
Major adverse cardiac events (MACE) were observed in 28 patients (15.22%), including 7 death cases, 5 myocardial infarction cases and 16 revascularization cases (Table 2). Patients with ACS revealed higher frequencies of MACE compared with the patients with SA (22.77% vs. 6.02%, P = 0.002). All of the patients suffering from MACE were treated on the basis of standard medication (aspirin and/or clopidogrel, nitrate, angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, β-receptor blocker, and statins). This standard medication was similar to that administered in patients without MACE. Patients’ characteristics, IVUS parameters, hs-CRP, and proMMP-1 were used in the univariate analysis for MACE and found that ACS, Troponin I and hs-CRP were associated with MACE (Table 4), while multivariate logistic regression found that only hs-CRP was independently associated with MACE for one year (Table 5).
Discussion
This study found that rupture and vulnerable plaques were more frequently observed in patients with ACS than in patients with SA. Serum hs-CRP and proMMP-1 were higher in patients with ACS than in patients with SA. Strong associations were found between hs-CRP, proMMP-1, and plaque type. hs-CRP but not plaque morphology was independently associated with MACE for one year.
Some studies found that hs-CRP could predict coronary events in coronary artery disease and even in healthy populations [9-12], however the controversy about the prognostic value of hs-CRP still remains [19-22], and because of different inclusion criteria of different studies, none of the conclusions was credited as universal. Most previous studies focused on the plaque characteristic and troponin concentration [14-18, 27, 28], whether there’s any predictive value of inflammatory markers as well as plaque indexes of IVUS independent on troponin remains unclear. In this study, the relationship between hs-CRP and IVUS findings with MACE was determined and has given an affirmative answer, which was based on Chinese CAD patients.
Though no further benefit was obtained in SA in COURAGE trial by stenting plus ideal medication therapy compared with ideal medication therapy alone, it is definitely clear that it would be of benefit in patients with extensive ischemia and of high risk. All the SA patients enrolled in the study were of classified grade Canadian Cardiovascular Society III-IV or positive stress electrokardiogram test, so most have stent implantation.
The disruption of vulnerable plaques is a common pathophysiology leading to ACS [29, 30]. Our study found that rupture and vulnerable plaques were more frequently found in patients with ACS than in patients with SA. This result is similar to that in a previous study [31]. Patients with ACS also showed an increased remodeling index, plaque area, lipid pool, and thrombus compared with patients with SA.
Recent advances showed that atherosclerosis might be a chronic inflammatory process; a pivotal role of inflammation is evident from initiation through progression and complication of atherosclerosis. CRP is considered as a major acute phase reactant in humans; this protein is mainly synthesized and secreted by hepatocytes. A 1000-fold increase in plasma CRP level occurs rapidly in response to inflammatory stimuli. Epidemiological studies have shown that hs-CRP plasma level is a strong, independent predictor of the risk of future cardiovascular disease events even in healthy individuals. hs-CRP level is also associated with thin-capped atheromas and rupture plaque [32-34]. CRP is one of the substances present in atherosclerotic plaque, particularly in the vascular intima, where CRP is co-localized with monocytes, monocytederived macrophages, and lipoproteins; this colocalization allows a direct contribution to the atherosclerotic process [35, 36]. CRP may also contribute to the development of atherosclerosis via complement activation; as a result, several processes, such as cell adhesion and recruitment, thrombosis, regulatory cytokines, and vascular cell apoptosis, are promoted. Our study found that hs-CPR in ACS was five times higher than that in SA. hs-CRP was positively related to the external elastic membrane cross-sectional area, lipid pool plaque, and plaque vulnerability; this result is consistent with that in other studies.
Studies have shown the following characteristics of vulnerable plaque [25, 26]: 1) lipid pool area > 1 mm2, lipid pool burden > 20%; 2) fibrous caps < 0.7 mm; and 3) strong inflammation reaction at the plaque cap. The thickness and collagen content of the fibrous cap are important to ensure the stability of a plaque. Plaque rupture occurs most frequently at a point where fibrous cap is the thinnest and most heavily infiltrated by macrophage foam cells. Matrix metalloproteinase (MMP) system is critical to determine the thickness of the fibrous cap and collagen of plaque; MMPs can also degrade virtually all of the components of the extracellular matrix [37, 38]. These substances are secreted in a latent zymogen form requiring extracellular activation. Several studies have identified MMPs in human coronary plaques. For instance, Brawn et al. [39] found that the macrophages and smooth muscle cells of plaque express an increased MMP-9 concentration in ACS; MMP concentrations in atherosclerotic plaque is higher than those in the normal artery wall. MMPs are also expressed in all parts of plaque, particularly in the lipid pool and rupture-prone part [40, 41]. MMP concentration and activity are increased in vulnerable plaques. Studies have also found that MMPs in plaque can be activated without any reactivators and degrade collagen IV and gelatinum. Inflammation factors influencing ACS can also promote the secretion of MMPs. This study found that Pro-MMP-1 was higher in the ACS group than in the SA group. Pro- MMP-1 was positively associated with plaque vulnerability. This result indicated that the imbalance of the MMP system might promote plaque rupture.
Several factors influence the prognosis of coronary heart disease. The results of ultivariate analysis for MACE revealed that ACS, hs-CRP, and troponin I were associated with MACE, while multivariate logistic regression revealed that only hs-CRP could be used as a predictor of MACE. This result could be attributed to coronary artery atherosclerosis as the mechanism of chronic inflammation; hence, inflammation may occur not only in one artery or one part of the artery but in all coronary arteries. Considering that IVUS was conducted only in one artery, we did not find any rupture or vulnerable plaque, but this result did not indicate the absence of such plaques in other coronary arteries. Although the culprit lesion was treated with stents in the study, other vulnerable or rupture plaques may remain untreated with stents. In vivo or in vitro factors, such as increased blood pressure, artery spasm, and anxiety, may promote the rupture of vulnerable plaques and lead to acute cardiac events. Several vulnerable and rupture plaques may form in one or several vessels [34]. Although IVUS is considered as a strong examination tool used to detect vulnerable and rupture plaque, this technique is not as powerful as other detection methods. Previous studies have found that troponin concentration, reflecting the degree of the death and damage of myocardial cell, has prognostic value in coronary heart disease [14-18], which was not observed in our study and might limited to study size. Hence, studies should be conducted in which a higher number of patients should be enrolled. Plaque morphology in all coronary arteries should be examined by optical coherence tomography to evaluate the prognostic value of plaque further. This study also indicated that a stronger drug therapy is necessary to treat lesions in addition to the culprit lesion treated with stent to avoid MACE. Indexes, such as hs-CRP indicated that inflammation in all of the coronary arteries and not local plaque morphology exhibited a prognostic value.
In conclusion, our results indicated that the increase in hs- CRP concentration is correlated with rupture and vulnerable plaques. Furthermore, hs-CRP and not plaque morphology is associated with poor prognosis of coronary artery disease in Chinese patients.
Study limitations
Our study also showed some limitations. For instance, IVUS is a reasonable but not an ideal tool that can be used to detect rupture and vulnerable plaque because IVUS cannot measure the thickness of a fabric cap less than 100 μm. This parameter is very essential in defining the type of plaque. In addition, a long-term follow-up (four to five years) period is possibly more accurate than the follow-up period considered in this study. Patients with ACS and stable patients should be grouped separately to improve prognosis.
Authors’ contributionsAuthors’ contributions
All authors listed in this manuscript participated in the design and coordination of the study and made substantial contribution to the intellectual content of the project to be included as authors. All authors read and approved the manuscript.
Competing interestsCompeting interests
The authors declare that they have no competing interests.
References
- Ross R. Atherosclerosis: an inflammation disease. N Engl J Med 1999; 340: 115-126.
- Tsujita K, Kaikita K, Soejima H, et al. Acute coronary syndrome-initiating factors. Nihon Rinsho 2010; 68: 07-614.
- Wang M, Jin W, Guo AM, Stubbe J. Cardiovascular inflammation. Mediators Inflamm 2013; 2013: 123513.
- Fiechter M, Ghadri JR, Jaguszewski M, et al. Impact of inflammation on adverse cardiovascular events in patients with acute coronary syndromes. J Cardiovasc Med (Hagerstown) 2013; 14: 807-814.
- Wynants M, Quarck R, Ronisz A, et al. Effects of Creactive protein on human pulmonary vascular cells in chronic thromboembolic pulmonary hypertension. Eur Respir J 2012; 40: 886-894.
- Chen Y, Wang X, Mai J, et al. C-reactive protein promotes vascular endothelial dysfunction partly via activating dipose tissue inflammation in hyperlipidemic rabbits. Int J Cardiol 2013; 168: 2397-2403.
- Jialal I, Kaur H, Devaraj S, Smith G. Human Creactive protein induces endothelial dysfunction in biobreeding diabetic rats. Diab Vasc Dis Res 2013; 10: 550-553.
- Wang CH, Li SH, Weisel RD, et al. C-reactive protein up-regulates angiotensin type1 receptors in vascular smooth muscle. Circulation 2003; 107: 1783-1790.
- Ridker PM, Cushman M, Stampfer MJ, et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 1997; 336: 973-979.
- Lukin A, Novak K, Polić S, Puljak L. Prognostic value of low and moderately elevated C-reactive protein in acute coronary syndrome: A 2-year follow-up study. Med Sci Monit 2013; 20: 777-786.
- Koenig W. High-sensitivity C-reactive protein and atherosclerotic disease: From improved risk prediction to risk-guided therapy. Int J Cardiol 2013; 168: 5126-5134.
- Puri R, Nissen SE, Libby P, et al. C-Reactive Protein, but not Low-Density Lipoprotein Cholesterol Levels, Associate with Coronary Atheroma Regression and Cardiovascular Events Following Maximally Intensive Statin Therapy. Circulation 2013; 128: 2395-2403.
- Devaraj S, Singh U, Jialal I. The evolving role of Creactive protein in atherothrombosis. Clin Chem 2009; 55: 229-238.
- Kim KH, Kim WH, Park HW, et al. Impact of plaque composition on long-term clinical outcomes in patients with coronary artery occlusive disease. Korean Circ J 2013; 43: 377-383.
- Marso SP, Mercado N, Maehara A, et al. Plaque composition and clinical outcomes in acute coronary syndrome patients with metabolic syndrome or diabetes. JACC Cardiovasc Imaging 2012; 5: S42-52.
- Calvert PA, Obaid DR, O'Sullivan M, et al. Association between IVUS findings and adverse outcomes in patients with coronary artery disease: the VIVA (VH-IVUS in Vulnerable Atherosclerosis) Study. JACC Cardiovasc Imaging 2011; 4: 894-901.
- Okura H, Kataoka T, Matsushita N, et al. Culprit lesion remodelling and long-term prognosis in patients with acute coronary syndrome: an intravascular ultrasound study. Eur Heart J Cardiovasc Imaging 2013; 14: 758-764.
- Yun KH, Mintz GS, Farhat N, et al. Relation between angiographic lesion severity, vulnerable plaque morphology and future adverse cardiac events (from the Providing Regional Observations to Study Predictors of Events in the Coronary Tree study). Am J Cardiol 2012; 110: 471-477.
- Rietzschel E, De Buyzere M. High-sensitive Creactive protein: universal prognostic and causative biomarker in heart disease? Biomark Med 2012; 6: 19-34.
- Correia LC, Esteves JP. C-Reactive protein and outcomes in acute coronary syndromes: a systematic review and meta-analysis. Arq Bras Cardiol 2011; 97: 76-85.
- Hemingway H, Philipson P, Chen R, et al. Evaluating the quality of research into a single prognostic biomarker: a systematic review and metaanalysis of 83 studies of C-reactive protein in stable coronary artery disease. PLoS Med 2010; 7: e1000286.
- D'Ascenzo F, Agostoni P, Abbate A, et al. Atherosclerotic coronary plaque regression and the risk of adverse cardiovascular events: a metaregression of randomized clinical trials. Atherosclerosis 2013; 226: 178-185.
- He B, Gai L, Gai J, et al. Correlation between major adverse cardiac events and coronary plaque characteristics. Exp Clin Cardiol 2013; 18: e71-76.
- Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2001; 37: 1478-1492.
- Ge J, Baumgart D, Haude M, et al. Role of intravascular ultrasound imaging in identifying vulnerable plaques. Herz 1999; 24: 32-41.
- Nissen SE. Application of intravascular ultrasound to characterize coronary atrtery disease and assess the progression or regression of atherosclerosis. Am J Cardiol 2002; 89: 21B-31B.
- Omland T, Pfeffer MA, Solomon SD, et al. Prognostic value of cardiac troponin I measured with a highly sensitive assay in patients with stable coronary artery disease. J Am Coll Cardiol 2013; 61: 1240-1249.
- Melki D, Lind S, Agewall S, Jernberg T. Prognostic value of combining high sensitive troponin T and terminal pro B-type natriuretic peptide in chest pain patients with no persistent ST-elevation. Clin Chim Acta 2012; 413: 933-937.
- Virmani R, Kolodgie FD, Burke AP, et al. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 2000; 20: 1262-1275.
- Akasaka T, Kubo T, Mizukoshi M, et al. Pathophysiology of acute coronary syndrome assessed by optical coherence tomograp. J Cardiol 2010; 56: 8-14.
- Zhang XW, Ge JB, Yang JM, et al. Relationship between hs-CRP, ProMMP-1, TIMP-1 and Coronary Plaque Morphology: Intravascular Ultrasound Study. Chin Med J 2006; 119: 1689-1694.
- Sano T, Tanaka A, Namba M, et al. C-reactive protein and lesion morphology in patients with acute myocardial infarction. Circulation 2003; 108: 282- 285.
- Hong YJ, Jeong MH, Choi YH, et al. Relation between high-sensitivity C-reactive protein and coronary plaque components in patients with acute coronary syndrome: virtual histology-intravascular ultrasound analysis. Korean Circ J 2011; 41: 440-446.
- Tanaka A, Shimada K, Sano T, et al. Multiple plaque rupture and C-reactive protein in acute myocardial infarction. J Am Coll Cardiol 2005; 45: 1594-1599.
- Torzewski J, Torzewski M, Bowyer DE, et al. Creactive protein frequently colocalizes with the terminal complement complex in the intima of early atherosclerotic lesions of human coronary arteries. Arterioscler Thromb Vasc Biol 1998; 18: 1386-1392.
- Zwaka TP, Hombach V, Torzewski J. C-reactive protein-mediated low density liprotein uptake by macrophages: implications for atherosclerosis. Circulation 2001; 103: 1194-1197.
- Siasos G, Tousoulis D, Kioufis S, et al. Inflammatory mechanisms in atherosclerosis: the impact of matrix metalloproteinases. Curr Top Med Chem 2012; 12: 1132-1148.
- Ogita M, Miyauchi K, Morimoto T, et al. Association between circulating matrix metalloproteinase levels and coronary plaque regression after acute coronary syndrome--subanalysis of the JAPAN-ACS study. Atherosclerosis 2013; 226: 275-280.
- Brown DL, Hibbs MS, Kearney M, et al. Identification of 92-KDgelatinase in human coronary atherosclerotic lesions. Circulation 1995; 91: 2125- 2131.
- Galis ZS, Sukhova GK, Lark MW, Libby P. Increased expression of matrix metalloproternases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Invest 1994; 94: 2493-2503.
- Pasterkamp G, Schoneveld AH, van der Wal AC, et al. Inflammation of the atherosclerotic cap and shoulder of the plaque is a common and locally observed feature in unruptured plaques of femoral and coronary arteries. Arterioscler Thromb Vasc Biol 1999; 19: 54-58.