Research Article - Journal of Cancer Immunology & Therapy (2019) Volume 2, Issue 1
Primary leiomyosarcoma of the adrenal gland: A review and update of literature.
Anthony Kodzo-Grey Venyo*
Department of Urology, North Manchester General Hospital, Manchester, United Kingdom
- *Corresponding Author:
- Anthony Kodzo-Grey Venyo
Department of Urology
North Manchester General Hospital
Crumpsall, Manchester, M8 5RB
United Kingdom
E-mail: akodzogrey@yahoo.co.uk
Accepted date: January 21, 2019
Citation: Venyo AKG. Primary leiomyosarcoma of the adrenal gland: A review and update of literature. J Cancer Immunol Ther. 2019;2(1): 7-18.
Abstract
Primary leiomyosarcoma of the adrenal gland (PLAG) is an uncommon non adrenal hormone producing malignant tumour of smooth muscle origin. PLAG has been sporadically reported more often in the female in comparison with in the male and hence PLAG would tend to be more commonly encountered in females in comparison with males. PLAG can also affect the younger age group contemporaneously with acquired immunodeficiency syndrome and Epstein-Barr virus infection. Patients who have PLAG may present with pain/discomfort in the loin or flank and or upper abdomen or as an incidental finding of an abdominal mass that has been present for many months and getting bigger. PLAG may also present with inferior vena cava syndrome when the tumour has invaded and obstructed the inferior vena emanating in the development of bilateral oedema of the lower limbs and angiomata on the abdominal wall. Basic or routine blood haematology and biochemistry test results tend to be normal as well as blood and urine adrenal hormone levels fall within normal range indicating a non-hormone secreting tumour. Radiology imaging investigations that are utilized to illustrate the adrenal gland position of the tumour and no other lesion in the abdomen include: ultrasound scan of abdomen and pelvis, CT scan of abdomen and pelvis, and MRI scan of abdomen and pelvis. If there is suspicion of obstruction of the IVC then inferior vena cavogram could be undertaken. Diagnosis can be obtained from histology and immunohistochemistry examination of biopsy and or adrenalectomy specimens which in most cases of the classical PLAG show: intersecting and sharply margined fascicles of spindled-cell; characteristic long and blunt ended tumour cell; cytoplasm of the tumours cells that vary from brightly eosinophilic fibrillar to pale cytoplasm; hyperchromatic nuclei; and generally pleomorphism. Positive immunohistochemistry staining for Smooth Muscle Actin (SMA), Desmin, H-caldesmon; Immunohistochemistry studies of primary leiomyosarcoma of the adrenal gland tend to show focally positive staining for: CD34, EMA, Keratin, and S100. With regard to PLAG in Immunocompromised patients, immunohistochemistry studies of the tumour do show that Desmin is less expressed. The main treatment for localized PLAG has been surgery (Adrenalectomy plus excision of adjacent involved organs and if there is tumour in the IVC up to the atrium the tumour is removed). Advanced and metastatic PLAG tumours have been treated by surgery and chemotherapy. The short-term and medium-term outcome of localized PLAG has been good; nevertheless, the long- term outcome is not well documented. With regard to advanced PLAGs, despite surgical removal of the primary tumour and chemotherapy the prognosis has not been good in that the patients generally do not tend to have good medium-term and long-term survival outcomes. In conclusion PLAG is an uncommon tumor which when diagnosed as a localized disease tends to be associated with good initial outcome but advanced PLAGs tend to be associated with inferior outcome. It would appear that the establishment of a global multi-centre trial of various chemotherapy treatment options that would identify treatment options that would improve the prognosis of advanced PLAG is needed.
Keywords
Leiomyosarcoma, Adrenal gland, Smooth muscle, Smooth muscle actin, Desmin, H-caldesmon, Spindle cells, Adrenalectomy, Chemotherapy, Renal vein, Inferior vena cava
Introduction
Primary leiomyosarcoma of the adrenal gland (PLAG) is a very uncommon malignant smooth muscle tumour that has been reported sporadically in the global literature. Because primary leiomyosarcoma of the adrenal gland (PLAG) is rarely encountered there is the possibility that diagnosis of the disease may be delayed because most clinicians would not be familiar with its presentation, diagnosis and management. This review article on primary leiomyosarcoma of the adrenal gland (PLAG) is divided into two parts (A) Overview and (B) Miscellaneous narrations and discussions from some reported cases, case series as well as studies related to primary leiomyosarcoma of the adrenal gland (PLAG).
Aim
To review the literature related to primary leiomyosarcoma of the adrenal gland.
Methods
Internet data bases were searched including: Yahoo; PUBMED; Google, and Google Scholar. The ensuing search words were used including: Leiomyosarcoma of the adrenal gland, adrenal leiomyosarcoma, and leiomyosarcoma of the suprarenal gland. Twenty four references were identified which were utilized to write the article.
Results/Literature Review
(A) Overview
General comments and definition: Leiomyosarcoma is a terminology that is used for a malignant tumour that has smooth muscle differentiation.
Only 30 cases of Leiomyosarcoma of the adrenal gland have been reported in the literature to the knowledge of the author [1].
The basic features of leiomyosarcoma include:
• A malignant tumour which on pathology examination exhibits pure smooth muscle differentiation.
• Leiomyosarcoma is characterised by microscopic examination finding of the tumour showing the typical intersecting fascicles of spindled blunt-ended cells.
• Immunohistochemistry staining studies of the tumour tend to show that in most of the cases, the tumour cells stain positively with Smooth Muscle Actin (SMA), Desmin, and h-caldesmon.
• Leiomyosarcomas that arise in patients that are immunocompromised tend to be associated with distinct characteristic features [2].
Epidemiology: Leiomyosarcomas of the adrenal gland are very uncommonly encountered tumours globally with only about 30 cases reported in the literature [1].
Leiomyosarcoma of the adrenal gland is most often found in elderly individuals [1,2].
Leiomyosarcoma of the adrenal gland does not have preference for any particular side of the body in that it tends to affect the left adrenal gland and the right adrenal gland equally [1].
It was previously stated that leiomyosarcoma of the adrenal gland has not been found to have preference for any sex in that it tends to affect the male and female equality [1,2]. However, out of 22 cases of PLAGs documented in PUBMED 6 cases of PLAG were documented in males who were aged 28 years, 49 years, 48 years, 63 years, 34 years, and 28 years and on the other hand 16 cases of PLAG were reported in females who were aged 73 years, 75 years, 49 years, 73 years, 60 years, 65 years, 23 years, 47 years, 47 years, 64 years, 61 years, 57 years, 68 years, 49 years, 64 years, 78 years, and 29 years which had indicated that PLAG has been found more commonly in the female that constituted about 72.7% of cases in comparison with about 27.3% for males. It would therefore be said that PLAG so far has been reported in females more preponderantly than in males.
Leiomyosarcoma of the adrenal gland tends to affect one adrenal gland only but few cases of bilateral leiomyosarcoma of the adrenal gland have been reported [1].
Presentation: Majority of patients who have leiomyosarcoma of the adrenal gland do present with pain in the abdomen and / or pain in the flank or loin pain [2].
Treatment: Surgery in the form of adrenalectomy has been the main option of treatment that had been adopted with regard to the treatment of leiomyosarcoma of the adrenal gland (LAG) especially for leiomyosarcomas of the adrenal gland (LAGs) that have been confined to the adrenal gland [1,2].
Adjuvant radiotherapy or adjuvant chemotherapy has been utilized in cases of primary leiomyosarcomas of the adrenal gland (PLAGs) especially in cases of invasive tumours that have invaded near-by organs including: the renal vein as well as the inferior vena cava [2].
Gross examination findings on pathology examination of primary leiomyosarcoma of the adrenal gland
Macroscopic pathology examination of primary leiomyosarcoma of the adrenal gland (PLAG) tends to show a fleshy grey-white tan adrenal mass [2].
Macroscopic pathological examination of a specimen of primary leiomyosarcoma of the adrenal gland (PLAG) may show a whorled appearance.
Macroscopic pathology examination of primary leiomyosarcoma often shows that the tumour has a wellcircumscribed border.
Microscopy (histological) examination features of primary leiomyosarcoma of the adrenal gland (PLAG)
The findings on histology examination of primary leiomyosarcoma of the adrenal gland have been summarized as follows:
• Microscopic (histological) examination of primary leiomyosarcoma of the adrenal gland (PLAG) tends show intersecting and sharply margined fascicles of spindledcells.
• Microscopic examination of the specimen of adrenal gland tumour also shows characteristic long and blunt ended tumour cells.
• Microscopic examination does show that the cytoplasm of the leiomyosarcoma tumours cells do vary from brightly eosinophilic fibrillar to pale cytoplasm.
• Histopathology (microscopical) examination of primary leiomyosarcoma of the adrenal gland (PLAG) also does show nuclei that are hyperchromatic as well as the examination also does generally show pleomorphism.
• Histopathology (microscopical) examinations of primary leiomyosarcoma of the adrenal gland (PLAGs) do show that majority of the primary leiomyosarcoma tumours of the adrenal gland (PLAGs) are the conventional type of leiomyosarcoma [2].
• Uncommon cases of pleomorphic type of primary leiomyosarcoma of the adrenal gland (PLAG) have been reported [3,4].
• With regard to leiomyosarcoma of the adrenal gland in patients who are HIV positive or in post-transplant patients who are Immunocompromised, histology examination of the adrenal tumours that are relatively bland but they could have primitive looking round cell components [2].
Cytological (cytology) examination characteristic features of primary leiomyosarcoma of the adrenal gland (PLAG)
Cytology examination of specimens of primary leiomyosarcoma of the adrenal gland do show the following:
• Fascicles that contain dispersed cells or stripped nuclei.
• Spindled tumour cells that have long, blunt-ended, segmented nuclei, or round polygonal cells that have round or indented nuclei.
Immunohistochemistry Studies findings
Positive Immunohistochemistry staining: Immunohistochemistry studies of primary leiomyosarcoma of the adrenal gland (PLAG) do exhibit positive immunohistochemistry staining for:
• Smooth Muscle Actin (SMA)
• Desmin
• H-caldesmon
Immunohistochemistry studies of primary leiomyosarcomas of the adrenal gland (PLAG) tend to show focally positive staining for:
• Keratin
• EMA
• CD34
• S100
With regard to primary leiomyosarcomas of the adrenal gland (PLAGs) in immunocompromised patients, immunohistochemical staining studies of the tumour do show less immunohistochemistry expression for (or less positive staining for) Desmin.
Negative Immunohistochemistry staining: Primary leiomyosarcomas of the adrenal gland (PLAGs) do exhibit negative immunohistochemistry staining with CD117.
Molecular/Cytogenetics description of primary leiomyosarcoma of the adrenal gland (PLAG)
It has been stated that with regard to primary leiomyosarcoma of the adrenal gland (PLAG), molecular and cytogenetic studies had demonstrated that the Karyotype often tends to be highly complex and also tends to be associated with genomic instability.
Differential diagnoses: Some of the differential diagnoses of primary leiomyosarcoma of the adrenal gland include:
• Retroperitoneal or metastatic leiomyosarcoma that has invaded or affected the adrenal gland (supra-renal gland).
• Primary rhabdomyosarcoma of the adrenal gland but in rhabdomyosarcoma of the adrenal gland immunohistochemistry studies of the tumour would show positive staining for myogenin and MyoD.
• Undifferentiated pleomorphic sarcoma but in such tumours immunohistochemistry studies would show lack of uniform desmin and SMA immunohistochemistry staining characteristics.
Prognostic factors:
• Primary leiomyosarcomas of the adrenal gland (PLAGs) have been stated generally to be associated with poor outcome.
• Primary leiomyosarcomas of the adrenal gland (PLAGs) are said to be have the tendency to develop local recurrent disease or distant metastases.
• The indicators of prognosis with regard to primary leiomyosarcoma of the adrenal gland include: the size of the tumour and the histological grade of the tumour in that large tumours and high histology grade tumours would tend to have worse prognosis in comparison with small-sized tumours and low histologically graded tumours.
• It had been documented that tumours that arise in immunocompromised individuals at times tend exhibit a better biological behaviour [2].
(B) Miscellaneous narrations and discussions from some reported cases, case series, and studies on primary leiomyosarcoma of the adrenal gland
Zhou et al. [1] reported a case of primary leiomyosarcoma of the adrenal gland (PLAG) and they did discuss extensively case series and studies on primary leiomyosarcoma of the adrenal gland as follows:
Zhou and associates [1] reported a 49-year-old woman who had a 10-year history of left-sided abdominal and back pin. Apart from having a medical history of hypertension she did not have any significant contributory past medical past history. With the exception of mild tenderness on the left side of her abdomen during palpation of her abdomen her physical examination was otherwise normal. She had a computedtomography (CT) scan of her abdomen which demonstrated a well-demarcated or a well-circumscribed heterogeneous mass which measured 6 x 5 x 5 cm in the region of her left adrenal. The CT scan did not demonstrate any thrombosis of vein or any metastasis. She had 24 hour urine collections which were tested for catecholamine’s and cortisol and the results were within normal range. The levels of her serum aldosterone and ACTH were within normal range. A diagnosis of nonfunctional let adrenal tumour was made. A laparoscopic left adrenalectomy was performed. Macroscopic (Gross) pathological examination of the specimen did reveal a roundlooking, grey-white that measured 8 x 6 x 5 cm. The tumour was found to have abutted tightly to the identifiable normal left adrenal gland that had been stretched by the tumour. Haemorrhagic areas and necrotic areas were observed within the tumour. Microscopic histology examination of the adrenal tumour showed a hyper-cellular (highly cellular) tumour that contained intersecting fascicles of spindle cells. The microscopic examination of the tumour also showed enlargement of nucleus and occasional giant cells. No tumour was identified within the surgical resection margins. Immunohistochemistry studies of the tumour showed that the tumour cells did stain positively for desmin, Smooth Muscle Actin, vimentin, and the tumour cells stained negatively for: Bcl-2, CD34, CD117, Gog1, as well as S100. The ki67 proliferation index was greater than 60 percent (60% which was high. The microscopy examination features and the immunohistochemistry study characteristics of the tumour were consisted with the diagnosis of primary leiomyosarcoma of the adrenal gland (PLAG). She did not receive any adjuvant therapy. At her 6-month post-operative follow-up, she was well and free of local recurrence and distant metastasis. Zhou et al. [1] stated the following:
• Primary leiomyosarcoma of the adrenal gland (PLAG) is very uncommon and that primary adrenal leiomyosarcoma (PLAG) was first documented by Choi and Liu in 1981 [5].
• It is understood that primary leiomyosarcoma of the adrenal gland does originate from smooth muscle wall of the central adrenal vein as well as the branches of the central adrenal vein [1].
• They had ascertained that only 30 cases of primary leiomyosarcoma of the adrenal gland (PLAG) had been reported in the literature [1].
• Majority of cases of primary leiomyosarcoma of the adrenal gland (PLAG) had been reported in elderly patients who did have large adrenal tumours [1].
• Majority of the previously reported patients had presented with pain in the abdomen or flank pain and patients who were diagnosed with tumours that had invaded into the inferior vena cava also had oedema of the lower limbs as well as spider angiomata [1].
• The primary leiomyosarcomas of the adrenal gland (PALs) had occurred in equal extent with regard to site of tumour whether left or right adrenal gland as well as the distribution of the tumour with regard to sex was equal in both female and male sexes [1].
• There were only two reported cases of bilateral adrenal gland leiomyosarcomas (BLAGs) [6,7].
• Majority of the reported cases of leiomyosarcomas of the adrenal gland (LAGs) were of the conventional type of leiomyosarcoma and 0nly 5 reported cases of primary leiomyosarcoma of the adrenal gland (PLAGs) had been of the pleomorphic type of tumour [3,4,8,9,10].
• Four of the patients who were reported to have primary leiomyosarcoma of the adrenal gland (PLAG) were immune-deficient because of HIV or Epstein-Barr virus infection; therefore, it would appear that primary leiomyosarcoma of the adrenal gland (PLAG) would likely occur in an immunosuppressive situation. The pathogenetic involvement of HIV and Epstein-Barr virus in primary leiomyosarcoma of the adrenal gland (PLAG) is not known for certain [6,11,12].
• Radical surgery is the main option of treatment for primary leiomyosarcoma of the adrenal gland (PLAG) but the outcome of the disease is not predictable [1].
• It has been stated that with regard to patients who have invasive primary leiomyosarcoma of the adrenal gland (PLAG) disease including: venous thrombosis, invasion of an adjacent organ, and distant metastases, the outcome is very poor or grim [1,13].
• Their review of all the 29 previously reported cases had shown that 12 patients who did not have any recurrent disease or metastatic disease were almost without invasive tumours and none of them had received any adjuvant of chemotherapy or radiotherapy [1].
• Strander et al. [14] did show in a systematic overview study that post-operative adjuvant radiotherapy was recommended for the treatment of locally advanced malignant tumours in soft tissue sarcomas.
• Radiotherapy and / or chemotherapy could be helpful with regard to shrinking the tumour and destroying the remaining tumoral cells [1].
Etten, et al. [15] reported a 73-year-old lady who had been referred from another hospital. She did report that 3 months prior to her admission she had noticed swelling of both of her legs and slight distension of her abdomen as well as intermittent pain in her abdomen. She had also lost appetite and she was fatigued over the preceding 3 months. She did have in the past, a gun-shot injury wound, which had resulted in laceration of the right lobe of her liver for which he had laparotomy and partial resection of her liver and cholecystectomy. On examination she was found to be pale and her blood pressure was within normal range. Her abdomen was visibly distended as well as on the abdominal wall there was a visible and obviously enlarged abdominal wall veins. A large and firm mass was palpated in the right upper part of her abdomen. There was also bilateral pitting oedema of her legs as well as distended veins on both of her legs which was consistent with inferior vena cava syndrome. The results of her routine haematology and biochemistry laboratory blood test investigations were summarized as follows:
Erythrocyte sedimentation rate 47 mm/hour (normal range 10 to 20 mm/hour).
Leucocytes showing leucocytosis with a count of 22.4 x 109/L (normal range 4-10 x 109/L).
Haemoglobin concentration 6.6 m-mole/litre (normal range 7.3-9.3 m-mols/litres).
Alkaline phosphatase 193 U/L (normal range 25-75 U/L).
Alkaline aminotransferase 33 U/L (normal range 5-30 U/L).
Aspartate aminotransferase 58 U/L (normal range (5-30 U/L).
Gamma glutamyl transpeptidase 79 U/L (normal range 5-35 U/L).
Lactate dehydrogenase 730 U/L (normal range 160-320 U/L).
Total bilirubin 22 micromoles/l (normal range 4-14 micromoles/l).
Creatinine 155 micromoles/l (normal range 60-110 micromoles/l).
Urea 2.3 micromoles/l (normal range 2.5-8 micromoles/litre).
She had computed tomography (CT) scan of the abdomen that showed a large mass possibly within the right kidney. She had inferior venacavogram investigation, which did demonstrate complete occlusion of inferior vena cava and also insertion of a stent inside the inferior vena cava was not technically feasible. She had magnetic resonance imaging (MRI) scan of her abdomen which showed that the large 25 cm longitudinal dimension mass had originated from the right adrenal gland and not from the right kidney. She had angiography study which demonstrated that the arterial blood supply to the tumour was from the right adrenal artery which had confirmed the adrenal origin of the tumour. She had radiology imagingguided percutaneous biopsy of the mass in the referring hospital and histology examination of the specimen showed a spindle tumour with characteristics of smooth muscle differentiation for which the differential diagnoses of leiomyoma and leiomyosarcoma were considered. Both her radiology imaging observations from the CT scan and the MRI scan did not show any evidence of metastasis to the brain, the lung or lymph nodes. She underwent laparotomy and during the procedure it was found that the tumour was very large and fixed to the under-surface of the liver and it was not possible to separate the tumour from the liver and the tumour was inoperable. The patient was provided palliative care and she died 3 months later. Her post-mortem examination revealed a 27 cm tumour that was attached to the liver but a normal right adrenal gland could not be found. The left adrenal gland (suprarenal gland) was found to be normal and there was thrombosis of the inferior vena cava due to external compression of the tumour as well as atelectasis of the right lung base. Her radiology images did not show any evidence of metastatic lesion anywhere in her body. Histology examination of the adrenal tumour showed a spindled cell tumour which had moderate degree of a typical with up to 10 mitoses per 2 mm, and areas of coagulative necrosis. The cells of the tumour were noted to be elongated, and they had blunt-ended nuclei, and the cytoplasm which had a fibrillar appearance was eosinophilia. Immunohistochemical staining study of the tumour showed that the tumour cells had stained positively for smooth muscle actin (SMA) which confirmed smooth muscle origin of the tumour.
Wang et al. [16] did report a 64-year-old lady who had presented with a heterogeneous mass in the region of her right adrenal gland that had extended into the inferior vena cava (IVC) and into the right atrium that measured 13.6 x 6.5 x 6.6 cm. The results of her biochemical work up showed that she had a non-hormonal functional adrenal tumour and her multiple tumour marker work up were negative. Wang et al. [16] did report the novel utilization of deep hypothermic circulatory arrest (DHCA) in the resection of the right adrenal vein leiomyosarcoma which had extended into the inferior vena cava and the right atrium. Wang et al. reported that the patient had remained free of disease at her 10-month follow-up pursuant to her surgery. Wang et al. [16] iterated that DHCA did afford a bloodless operative field for optimal resection of tumoral disease from the inferior vena cava. Wang et al. [16] made the following conclusions:
• The diagnosis of leiomyosarcoma of the adrenal gland (LAG) is undertaken by means of exclusion of other diseases or tumours and the process does involve preoperative radiology imaging, and biochemical assessments to exclude other functional tumours of the adrenal gland.s
• The adoption of aggressive surgical resection of leiomyosarcoma of the adrenal gland (LAG) tends to be associated with improved survival and could be best achieved through collaborative multi-disciplinary team involvement of different surgical subspecialties.
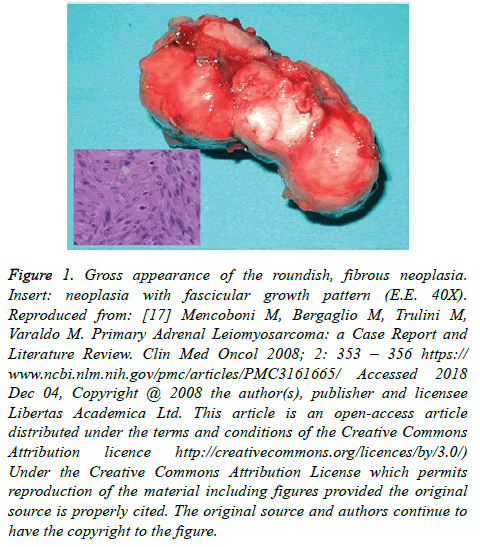
Mencoboni et al. [17] did report a 75 year-old Caucasian woman who had been having persistent and progressive epigastric and right loin pain for about one month. She had a medical history of hypertension. With the exclusion of mild tenderness in her abdomen which was found during her examination her examination was generally normal. She had ultrasound scan of her abdomen which showed a mass in her right adrenal gland. The results of her routine haematology and biochemistry blood tests were normal the results her other investigations were normal including: urinary levels of Vanillylmandelic acid, catecholamine, and plasma levels of aldosterone. She had chest radiograph and ECG which were normal, She had upper gastrointestinal endoscopy which showed hiatus hernia and reflux oesophagitis. She had a computed tomography (CT) scan of the whole body which showed a mass in her right adrenal gland that measured 5 x 4 cm which was considered to be an adrenal carcinoma. She underwent resection of a roundish mass from her right adrenal gland site. Normal adrenal gland could not be seen in the excised mass (Figure 1).
Figure 1: Gross appearance of the roundish, fibrous neoplasia. Insert: neoplasia with fascicular growth pattern (E.E. 40X). Reproduced from: [17] Mencoboni M, Bergaglio M, Trulini M, Varaldo M. Primary Adrenal Leiomyosarcoma: a Case Report and Literature Review. Clin Med Oncol 2008; 2: 353 – 356 https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC3161665/ Accessed 2018 Dec 04, Copyright @ 2008 the author(s), publisher and licensee Libertas Academica Ltd. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution licence http://creativecommons.org/licences/by/3.0/) Under the Creative Commons Attribution License which permits reproduction of the material including figures provided the original source is properly cited. The original source and authors continue to have the copyright to the figure.
Three days after her operation she developed a drop in her haemoglobin to 7.7 gm/dl for which she was transfused and she also developed pulmonary embolism and a thrombus in her inferior vena cava and she required intravenous anticoagulant treatment as well as warfarin treatment in the intensive care unit. She did recover well and was discharged on the 18th postoperative day after Doppler ultrasound scan had confirmed normal venous flow through her inferior vena cava. She did not receive any adjuvant therapy in the form of radiotherapy or chemotherapy but she remained well and was disease-free at her 12 month follow-up. Macroscopic pathology examination of the surgical specimen showed a roundish, neoformation of 8 x 4 x 5 cm. A thrombus was found in the adrenal vein on macroscopic examination of the specimen even though it was previously stated that there was no evidence of a thrombus in the adrenal vein in the pre-operative CT scan images. Upon sectioning of the tumour, no normal adrenal tissue was visible and the surgical resection was free of tumour.
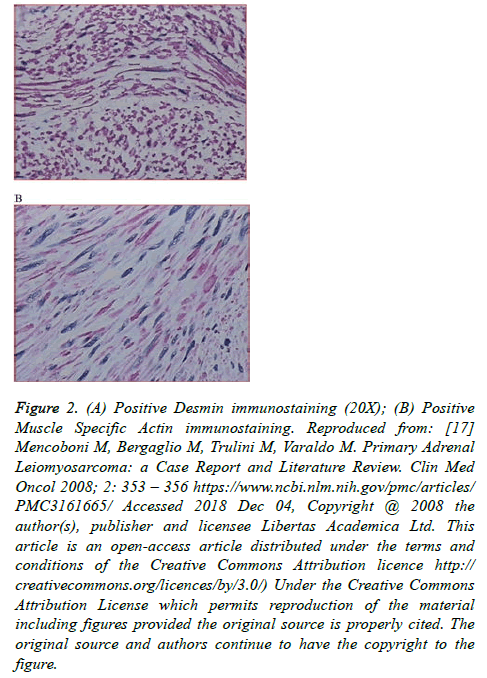
Histopathology microscopy examination of the tumour showed elongated tumour cells that had eosinophilic cytoplasm and elongated nuclei that had rounded ends, small nucleoli with moderate polymorphism. The cells of the tumour were seen on microscopy examination to be arranged in fascicles. Microscopic examination of the specimen showed on average 16 mitoses per 50 high-power field and no necrosis was seen (Figure 1). Immunohistochemistry staining studies of the tumour showed that the tumour cells were strongly and diffusely positively stained for desmin (Smooth Muscle Actin (SMA) (Figure 2A) using Primary body Antibody, and actin (HHF3 Muscle-Specific Actin, HHF35- Primary Antibody) (Figure 2). Immunohistochemistry staining showed that the tumour cells were negative for CD34 and CD117. The result of the Ki-67 nuclear antigen (monoclonal (MIB1) Antibody) was documented as 20%. The microscopic and immunohistochemistry features of the tumour were consistent with the diagnosis of primary leiomyosarcoma of the adrenal gland (PLAG) origin pT2/G2 based upon the UICC criteria.
Figure 2: (A) Positive Desmin immunostaining (20X); (B) Positive Muscle Specific Actin immunostaining. Reproduced from: [17] Mencoboni M, Bergaglio M, Trulini M, Varaldo M. Primary Adrenal Leiomyosarcoma: a Case Report and Literature Review. Clin Med Oncol 2008; 2: 353 – 356 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3161665/ Accessed 2018 Dec 04, Copyright @ 2008 the author(s), publisher and licensee Libertas Academica Ltd. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution licence http://creativecommons.org/licences/by/3.0/) Under the Creative Commons Attribution License which permits reproduction of the material including figures provided the original source is properly cited. The original source and authors continue to have the copyright to the figure.
Gulpinar et al. [18] did report a 48-year-old man who presented with symptoms related to his lower urinary tract. His father was diagnosed with carcinoma of the prostate gland. A mass was palpated in the right upper quadrant of his abdomen. Digital rectal examination revealed a normal benign feeling prostate gland. He did have ultrasound scan of the abdomen which showed a mass in his right adrenal gland which measured 86 x 83 cm. He had magnetic resonance imaging (MRI) scan of his abdomen which showed 90 x 65 mm hypervascular contrast-enhancing solid mass in his right adrenal gland which had extended to the right lobe of the liver. He had a Chest X-ray which was normal. He had 24-hour urine for Vanillylmandelic acid, metanephrine, and nor-metanephrine as well as urinary free cortisol which were normal. He underwent right adrenalectomy which was started as a laparoscopy procedure and was converted to open right adrenalectomy. His post-operative recovery was unremarkable. Gross pathology examination of the right adrenalectomy specimen showed a 110 x 80 x 65 mm mass that weighed 370 grams. Macroscopic inspection of sections of the tumour did show a yellowcreamy- white, solid, mass that contained a central necrotic area. Histopathology (microscopic) examination of the specimen revealed a thick fibrous capsule, and it also revealed that the tumour itself contained spindled cells that were associated with mostly diffuse plasma cell infiltration which was prevalent in the areas of necrosis. The cells of the tumour were characterized by occasional bizarre giant cells, wide spread apoptosis, and patchy areas of mitoses. Immunohistochemistry studies of the tumour showed mainly negative staining for the following tumour markers: pancytokeratin, inhibin, synaptophysin, chromogranin, CD30, CD31, CD34, CD117, S100, ALK, myogenin, lambda, and kappa light chain proteins. However, immunohistochemistry staining studies did show that the tumour cells stained strongly and diffusely positive for vimentin, and moderately and diffuse positive staining for Smooth Muscle Actin (SMA), as well as Ki-67 also showed 4% immunopositivity. The microscopy examination features and the immunohistochemistry features of the tumour were consistent with the diagnosis of low-grade leiomyosarcoma of the adrenal gland. He had been undergoing clinical follow-up and at his 8-months follow-up there was no clinical evidence of local recurrence or distant metastasis and also he had a CT scan at his 6-month follow-up which did not show any evidence of metastatic disease.
Lee et al. [19] reported a 28-year-old man who had persistent and stabbing right flank pain, and weight loss. He did not have any symptoms and signs of HIV infection or Epstein-Barr virus infection. He did have a computed tomography scan which showed a well-circumscribed, heterogeneous, and contrastenhancing in the region of his right adrenal gland that measured 13.8 cm. A review of the computed tomography (CT) scan did not reveal any metastatic disease. The results of his white blood cell count and differential eosinophil count were within normal range. He had a biochemistry evaluation which showed that the results had confirmed that the adrenal tumour was a non-functioning tumour. He did undergo open right adrenalectomy. Macroscopic pathology examination of the right adrenalectomy revealed a large and lobulated mass that measured 15 x 13 x 6 cm and which weighed 792 grams. The tumour which was a well circumscribed and partially encapsulated on visualization had replaced almost the entire adrenal gland. Histopathology (microscopy) examination of the tumour did show a spindle cell tumour that had a rim of fibrous tissue and entrapped atrophic adrenal cortical cells as well as geographic coagulative necrosis in addition to encompassing fibrosis and observation of frequent mitotic figures which amounted to 25 mitotic figures per 10 high-power fields.
The adrenal gland tumour was graded as grade 3 based on the Fédéracion Nationale des Centres de Lutte Contre le Cancer (FNCLCC) classification of tumour gradin. Immunohistochemistry studies of the tumour showed that the tumour cells had demonstrated strongly cytoplasmic positive staining for Smooth Muscle Actin (SMA), and for desmin. Furthermore, immunohistochemistry studies of the tumour showed that tumour cells had stained negatively for the following antibodies: pan-cytokeratin, CD117, S-100 protein, and human melanoma black protein. Additionally, histology examination of the tumour showed tissue eosinophilia. It was observed that the eosinophilic infiltration was mainly found in the viable tumour cells. The centre of the area that was necrotic did not have eosinophils or inflammatory cells. A few pleomorphic tumour cells that had hyperchromatic nuclei were seen. Majority of the tumour cells of the tissue eosinophilia had vesicular nuclei, shrinkage of cytoplasm, as well as the occasional pink, rounded nucleoli. The Histology features and the immunohistochemistry study characteristics of the tumour were consistent with the diagnosis of primary leiomyosarcoma of the adrenal gland. The patient remained alive and well without any evidence of recurrence of disease at his 18 month follow-up. Whilst it had previously been stated that primary leiomyosarcoma of the adrenal gland (PLAG) does affect the elderly, this case report would remind clinicians and patients that primary leiomyosarcoma of the adrenal gland can also affect younger adults and perhaps the disease could also affect children.
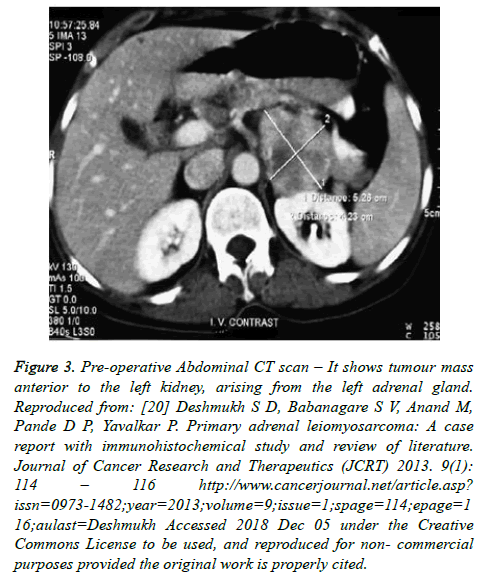
Deshmukh et al. [20] did report a 60-year-old lady who presented with a 5-months history of left upper quadrant abdominal mass which had been painful with pain in her left flank and gradually increasing in size. On examination a mass was palpated in her left hypochondrium that measured 5 x 4 x 3 cm. Her routine laboratory haematology and biochemistry investigations were normal. The result of her 24 hour urine vanillylmandelic acid was normal and her HIV-1 and HIV-2 antibody tests were non-reactive as well as HBsAg. She had computed tomography (CT) scan which showed a well-defined heterogeneous contrast-enhancing left adrenal gland tumour that measured 5.2 x 4.5 x 3.8 cm, posterior to the body of the pancreas and anterior to the left kidney (Figure 3). There was no evidence of any other tumour anywhere on demonstrated on the CT scan. She did undergo laparotomy which revealed a left retroperitoneal mass that arose from the left adrenal gland which was completely excised by open left adrenalectomy. At her 21-month post-operative follow-up, she was well without any evidence of local recurrence or distant metastases.
Figure 3: Pre-operative Abdominal CT scan – It shows tumour mass anterior to the left kidney, arising from the left adrenal gland. Reproduced from: [20] Deshmukh S D, Babanagare S V, Anand M, Pande D P, Yavalkar P. Primary adrenal leiomyosarcoma: A case report with immunohistochemical study and review of literature. Journal of Cancer Research and Therapeutics (JCRT) 2013. 9(1): 114 – 116 http://www.cancerjournal.net/article.asp? issn=0973-1482;year=2013;volume=9;issue=1;spage=114;epage=1 16;aulast=Deshmukh Accessed 2018 Dec 05 under the Creative Commons License to be used, and reproduced for non- commercial purposes provided the original work is properly cited.
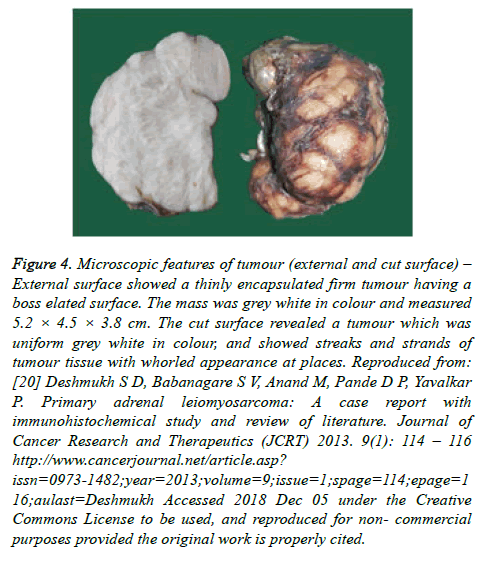
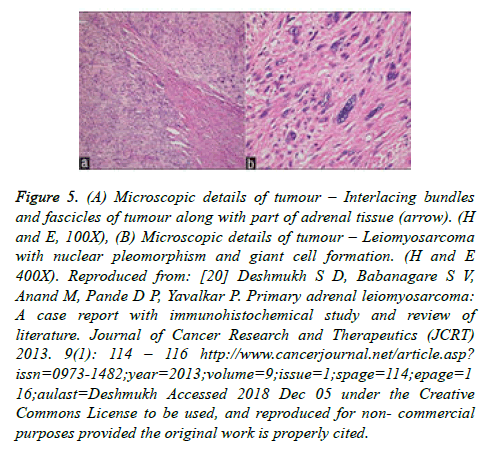
Macroscopic pathology examination of the tumour revealed a 5.2 x 4.5 x 3.8 cm, firm tumour mass with a thin capsule and a boss elated appearance which had almost completely replaced the entire adrenal gland (Figure 4). Upon sectioning the tumour, the cut surface of the tumour showed uniform, greywhite colour that had streaks, and strands as well as whorled looking features in some places. There was no area of necrosis or haemorrhage. Microscopy examination of the specimen showed a tumour that was thinly encapsulated which had comprised of spindled tumour cells that were arranged in interlacing bundles and fascicles that were variable in size. The individual tumour cells did have moderate eosinophilic cytoplasm as well as cigar-shaped nuclei and dispersed chromatin. Part of normal looking adrenal cortical tissue was found in the peripheral area of the tumour from which the tumour had arisen (Figure 5A). The tumour cells exhibited nuclear pleomorphism, formation of giant cells, and 10 to 12 abnormal mitotic figures per 10 high-power fields were seen (Figure 5B). Many congested blood vessels were seen in the stroma; nevertheless, no areas of necrosis or lympho-vascular invasion were found in the tumour. Immunohistochemistry staining studies of the tumour demonstrated that the tumour cells showed strong cytoplasmic positive staining for Smooth Muscle Actin (SMA) (Figure 6A), desmin (Figure 6B), and vimentin. Immunohistochemistry study also showed that the tumour cells were negatively stained for: Cytokeratin (CK), CD117, and CD34, HMB-45, and S100 protein. Based upon the histology features and the immunohistochemistry features of the tumour a final diagnosis of primary leiomyosarcoma of the adrenal gland was made.
Figure 4: Microscopic features of tumour (external and cut surface) – External surface showed a thinly encapsulated firm tumour having a boss elated surface. The mass was grey white in colour and measured 5.2 × 4.5 × 3.8 cm. The cut surface revealed a tumour which was uniform grey white in colour, and showed streaks and strands of tumour tissue with whorled appearance at places. Reproduced from: [20] Deshmukh S D, Babanagare S V, Anand M, Pande D P, Yavalkar P. Primary adrenal leiomyosarcoma: A case report with immunohistochemical study and review of literature. Journal of Cancer Research and Therapeutics (JCRT) 2013. 9(1): 114 – 116 http://www.cancerjournal.net/article.asp? issn=0973-1482;year=2013;volume=9;issue=1;spage=114;epage=1 16;aulast=Deshmukh Accessed 2018 Dec 05 under the Creative Commons License to be used, and reproduced for non- commercial purposes provided the original work is properly cited.
Figure 5: (A) Microscopic details of tumour – Interlacing bundles and fascicles of tumour along with part of adrenal tissue (arrow). (H and E, 100X), (B) Microscopic details of tumour – Leiomyosarcoma with nuclear pleomorphism and giant cell formation. (H and E 400X). Reproduced from: [20] Deshmukh S D, Babanagare S V, Anand M, Pande D P, Yavalkar P. Primary adrenal leiomyosarcoma: A case report with immunohistochemical study and review of literature. Journal of Cancer Research and Therapeutics (JCRT) 2013. 9(1): 114 – 116 http://www.cancerjournal.net/article.asp? issn=0973-1482;year=2013;volume=9;issue=1;spage=114;epage=1 16;aulast=Deshmukh Accessed 2018 Dec 05 under the Creative Commons License to be used, and reproduced for non- commercial purposes provided the original work is properly cited.
Figure 6: Immunohistochemical findings - (A) Tumour cells showing strong immunoreactivity for smooth muscle actin (SMA) (400X), and (B) immunoreactivity for desmin (400X). Reproduced from: [20] Deshmukh S D, Babanagare S V, Anand M, Pande D P, Yavalkar P. Primary adrenal leiomyosarcoma: A case report with immunohistochemical study and review of literature. Journal of Cancer Research and Therapeutics (JCRT) 2013. 9(1): 114 – 116 http://www.cancerjournal.net/article.asp? issn=0973-1482;year=2013;volume=9;issue=1;spage=114;epage=1 16;aulast=Deshmukh Accessed 2018 Dec 05 under the Creative Commons License to be used, and reproduced for non- commercial purposes provided the original work is properly cited.
Zetler and associates [11] did report a primary leiomyosarcoma of adrenal gland (PLAG) in a 30-year-old man, who had tested positive for human immunodeficiency virus (HIV++). Zetler and associates [11] indicated that their reported case was the first case of primary leiomyosarcoma of the adrenal gland (PLAG) to be reported in an adult male who had acquired immunodeficiency syndrome. They also stated that the smooth muscle origin of the leiomyosarcoma of the adrenal gland was obvious based upon their microscopic examination finding on examination of the tumour which was confirmed by positive immunohistochemistry staining of the tumour cells for smooth muscle actin (SMA). Zetler and associates [11] also did report that the patient was well without any evidence of local recurrence of tumour or distant metastases. Zetler and associates alluded to the reported rising incidence of smooth muscle origin tumours in human immunodeficiency infected patients and the associated aetiological role of Epstein-Barr virus in the pathogenesis of leiomyosarcoma [11].
Bhalla et al. [21] did report a 45-year-old man, who presented with pain in his back and right groin. His radiology imaging evaluation showed a heterogeneous 11 cm mass in his right adrenal gland as well as multiple liver metastases, and an enlarged aortocaval lymph node. There was no evidence of any mass in the retroperitoneum. The core-needle biopsies of the “tumour-mass,” and pathology examination of the biopsy specimen showed a malignant mesenchymal tumour which was composed of atypical spindle shaped cells that were arranged in intersecting fascicles as well as the microscopy examination of the specimen showed high mitotic activity, and focal necrosis of tumour. Immunohistochemistry staining studies of the tumour showed positive staining for smooth muscle actin (SMA) and desmin. Immunohistochemical staining of the tumour also showed that the tumour cells stained negatively for S-100 and c-kit stains. The histological examination characteristic features of the tumour, was consistent with the diagnosis of primary leiomyosarcoma of the adrenal gland (PLAG) with liver metastases, and that the tumour was an aggressive tumour which was diagnosed at an advanced stage. Bhalla et al. [21] stated that: at the time of the report of their case of leiomyosarcoma of the adrenal gland with metastases to the liver, 25 cases of primary leiomyosarcoma of the adrenal gland (PLAG), had been reported, and that none of the previously reported cases had been diagnosed based upon the results of core-needle -biopsy. Their case was therefore the first case of primary leiomyosarcoma of the adrenal gland (PLAG) to be diagnosed based upon core needle-biopsy of the tumour. Bhalla et al. [21] emphasised that definitive diagnosis of primary leiomyosarcoma of the adrenal gland (PLAG), in cases of advanced disease, should obviate the need for surgical biopsies.
Wei et al. [22] reported a 57-year-old lady, who was found incidentally to have a space occupying lesion in her left adrenal gland. She had computed tomography (CT) scan of her abdomen which showed a 6.4 x 7.7 cm soft tissue mass in her left adrenal gland. She did undergo left radical nephroadrenalectomy (excision of left kidney and left adrenal gland). Histological examination of the tumour revealed malignant spindled cells that were arranged in interlacing fascicles and whorls. The histology examination also showed nuclear pleomorphism, tumour giant cells, necrosis and abnormal mitotic figures. Immunohistochemistry studies of the tumour showed that the tumour cells were strongly positively stained for smooth muscle actin (SMA), desmin and vimentin. Immunohistochemistry studies of the tumour also showed that the tumour cells were negatively stained for: cytokeratin, CD117, CD34, CD68, Myoglobin, S100, and HMB-45. The histopathology features and the immunohistochemistry characteristics of the tumour were consistent with the diagnosis of primary leiomyosarcoma of the adrenal gland.
Hamada et al. [7] did report a 62-year-old lady, who had presented with right loin pain. She had computed tomography (CT) scan of her abdomen which showed bilateral adrenal gland tumours that measured 8 cm in the right adrenal gland, and 4 cm in the left adrenal gland. Her general and systematic examinations were normal. The biochemistry test results of the adrenal hormone levels in her serum and urine were within the normal ranges. She had radiology imaging studies, which revealed a right adrenal tumour that contained: intra-tumoral haemorrhage, a cystic tumour in the left adrenal gland, and no evidence of distant metastasis. The tumours were considered to be non-functional adrenal tumours because of the normal serum and urine levels of her adrenal hormones. She underwent surgical removal of the right adrenal gland tumour. The histopathological (microscopic) examination features of the excised adrenal gland, was consistent with primary leiomyosarcoma of the adrenal gland (PLAG). She did have post-operative computed tomography (CT) scan of her thorax, which showed pleural metastatic lesions in the right chest wall. She received combination systemic chemotherapy that included cyclophosphamide, vincristine, Adriamycin, dacarbazine. The pleural metastases were also treated with radiofrequency ablation (RFA). Despite receiving two courses of combination chemotherapy, the left adrenal tumour continued to grow rapidly; therefore, the left adrenal tumour was surgically removed. Following the removal of the left adrenal leiomyosarcoma, the patient developed right iliac bone metastasis which was treated with radiofrequency ablation (RFA) and radiotherapy. She had positron emission tomography (PET-CT) scan, which showed bilateral femoral metastases which were treated with radiotherapy in combination with low dose cisplatin chemotherapy. She subsequently developed liver metastasis and a small metastasis in her left kidney, which were treated with radiofrequency ablation (RFA). She additionally developed metastasis in the tail of her pancreas which required removal of the tumour surgically by distal pancreatectomy. Sixteen months pursuant to her right adrenalectomy she died due to disseminated systemic spread of metastases of the leiomyosarcoma. Hamada et al. [7] intimated that: multiple local treatments including radiofrequency ablation (RFA), radiotherapy, and resection of tumour were effective with regard to the local control of metastatic lesions of leiomyosarcoma of the adrenal gland. The outcome of the patient would alert clinicians about the fact that the combination systemic chemotherapeutic agents that the patient received were not effective in destroying the leiomyosarcoma tumour cells and for this reason, it would be suggested that clinicians and oncologists globally should identify chemotherapeutic agents and chemotherapeutic regimens that would be capable of destroying leiomyosarcoma of adrenal gland tumours in order to prolong life and increase the disease-free survival of individuals who have advanced leiomyosarcoma of adrenal gland. This can be achieved by establishing multi-centre global chemotherapy trials for patients who have leiomyosarcoma of the adrenal gland.
Lujan and Hoang [8] did report a 63-year-old man, who presented with a 1 year history of enlarging mas in the right upper quadrant of his abdomen. He did have computed tomography (CT) scan, which showed a mass in the region of his right adrenal gland. The tumour had extended into the upper pole of his right kidney and the posterior aspect of the right lobe of his liver. A pulmonary mass was also identified on the computed tomography (CT) scan. A computed tomography – (CT) guided biopsy of the mass was undertaken, and a histological diagnosis of metastatic pulmonary carcinoma to the adrenal gland was made. He received pre-operative chemotherapy with paclitaxel which resulted in considerable reduction of the pulmonary mass; nevertheless, the adrenal mass had continued to grow bigger. A composite resection of the tumours was attempted that included: resection of the right lobe of the liver, cholecystectomy (excision of the gall bladder), right adrenalectomy with a large tumour, and right radical nephrectomy. The patient died soon after the surgical operation; nevertheless, autopsy was not performed. Macroscopic pathology examination of the surgically excised specimens revealed a large haemorrhagic, multi-nodular mass that measured 25 x 12 x 12 cm and which had completely replaced the right adrenal gland. The tumour had extended into the right lobe of the liver as well as the upper pole of the right kidney. The tumour had been well demarcated both the parenchyma of the liver and the parenchyma of the kidney by a thick fibrous capsule. Histopathological (microscopic) examination of the surgical specimens, revealed a diffuse proliferation of pleomorphic tumour cells. The cells of the tumour were noted to be large and polygonal and they had prominent nucleoli. In certain areas of the tumour, the pleomorphic tumour cells and bizarre mitotic figures were observed. Microscopic examination of the tumour also showed perivascular growth of neoplastic cells as well as large irregular areas of necrosis. Typical characteristic features of smooth muscle tumours that are typified by presence of spindled tumour cells with cigar-shaped nuclei that had been arranged in fascicles were not seen on microscopy examination of the tumour. Immunohistochemical staining of the tumour showed that the tumour cells had exhibited strongly positive staining for: calponin, desmin, neuron-specific enolase, and vimentin. Immunohistochemistry staining studies of the tumour also showed that the tumour cells had stained negatively for: CD117, cytokeratin (AE1/AE3), carcinoembryonic antigen, epithelial membrane antigen (EMA), chromogranin, CD34, CD31, HMB-45, musclespecific- actin, myoglobin, myogenin, S100 protein, and smooth muscle actin (SMA). Additionally, Ki-67 did label about 80% of the tumour cells. It has been learnt from this study that: majority of the classic leiomyosarcoma of the adrenal gland tumours would tend to stain positively for smooth muscle actin (SMA); the pleomorphic variant of leiomyosarcoma has its own microscopic features and it may also not stain positively for smooth muscle actin (SMA). Another lesson learnt from this case report is that the tumour did not clearly respond to the paclitaxel chemotherapy in that the adrenal gland tumour continued to grow bigger whilst the patient was receiving chemotherapy. This lesson should alert clinicians to accept that there is no clearly identified chemotherapeutic agent that would quickly and satisfactorily destroy leiomyosarcoma of adrenal gland tumour cells. In view of this knowledge there is clearly a need for oncologists and clinicians globally to identify chemotherapeutic agents and appropriate chemotherapeutic regimen that would quickly and clearly kill leiomyosarcoma tumour cells and thus lead to prolongation of life and disease-free survival of patients who have extensive and advanced leiomyosarcoma of the adrenal gland. A global multicentre trial would be needed to achieve the aforementioned aim.
Shao et al. [23] reported a 66-year-old man, who was a hepatitis B virus carrier, and who was found to have a huge left adrenal gland mass on ultrasound scanning and upon CT scanning of his abdomen. He had radiology imaging which showed a large tumour in his left supra-renal region as well as a markedly engorged left adrenal vein were identified during his adrenalectomy operation. The tumour thrombus had extended into the left renal vein, close to the inferior vena cava. The left adrenal gland together with the entire tumour thrombus was removed completely. Microscopy examination of the tumour specimen showed that the adrenal gland had been compressed by but it had not been invaded by the spindled cell tumour that had consisted of interlacing fascicles of malignant smooth muscle cells. The tumour had been localized within the left adrenal vein and had arisen from the wall of the vein. At his 18 months post-operative follow-up patient was well and had not developed any local recurrence pursuant to en bloc excision of his tumour. Shao et al. recommended that en bloc excision with a clear and adequate surgical margin would be the most important curative surgical procedure for adrenal gland leiomyosarcoma.
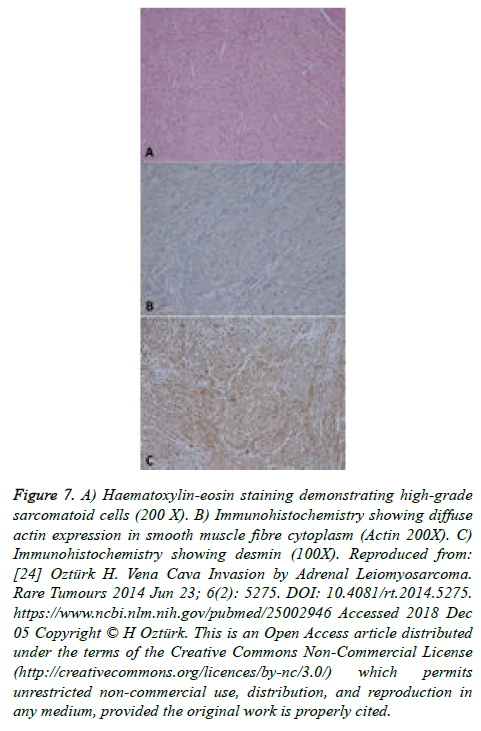
Oztürk [24] reported a 70-year-old lady, who had presented with right loin pain. She had computed tomography scan of abdomen and pelvis which showed aright adrenal mass that had a diameter of 7.8 cm, and which had exerted pressure upon the inferior vena cava. She underwent right adrenalectomy as well as inferior venacavatomy and excision of the invasive part of the tumour. Tumour extension or infiltration was seen in the wall of the excised inferior vena cava. Histology examination of the specimen at 10X magnification showed 8 to 10 mitotic figures (Figure 7A). Immunohistochemical staining studies of the tumour, showed that the tumour cells had stained positively for smooth muscle actin (SMA) (Figure 7B), and for desmin (Figure 7C). Immunohistochemical staining studies of the tumour also showed that the tumour cells had stained negatively with cytokeratin, and Bcl-2. Furthermore, the Ki67 proliferation index was 70%. The patient developed widespread metastases six months after she had undergone her adrenalectomy operation. The lesson learnt from this case report, is that if a leiomyosarcoma of the adrenal gland or vein has invaded the inferior vena cava, even if the part of inferior vena cava that is invaded is successfully excised with a clear surgical margin, that tumour should be regarded as one that potentially could metastasize in the near future due to the fact that tumour micro-emboli may have been disseminated prior to the operation and these tumour micro-emboli would grow in the future. For this reason the ensuing issues should be considered: Ideally patients with such types of tumours should be treated with adjuvant therapy, especially, with chemotherapy; But so far, it would appear as if there is no consensus opinion on the best chemotherapy treatment that would kill leiomyosarcoma tumour cells and prolong life as well as result in long-term disease free survival. In view of this, it is the view of the author that a global multi-centre trial of various adjuvant therapies versus no adjuvant therapy should be undertaken to establish the best chemotherapy treatment that should be provided for such types of leiomyosarcomas of the adrenal gland.
Figure 7: A) Haematoxylin-eosin staining demonstrating high-grade sarcomatoid cells (200 X). B) Immunohistochemistry showing diffuse actin expression in smooth muscle fibre cytoplasm (Actin 200X). C) Immunohistochemistry showing desmin (100X). Reproduced from: [24] Oztürk H. Vena Cava Invasion by Adrenal Leiomyosarcoma. Rare Tumours 2014 Jun 23; 6(2): 5275. DOI: 10.4081/rt.2014.5275. https://www.ncbi.nlm.nih.gov/pubmed/25002946 Accessed 2018 Dec 05 Copyright © H Oztürk. This is an Open Access article distributed under the terms of the Creative Commons Non-Commercial License (http://creativecommons.org/licences/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Conclusion
PLAG is an uncommon malignant tumour of smooth muscle origin that affects both sexes and more often in the older age group but younger males and females can also be affected especially patients who have acquired immunodeficiency syndrome. It would appear that despite utilization of surgery and chemotherapy in the treatment of advanced PLAG the prognosis of advanced PLAG has generally not been good. It also does appear that there is need for a global multi-centre trial of surgery plus various combinations of chemotherapeutic regimens to establish the options of treatment that would improve the long-term disease free survival of the advanced disease.
Conflict of Interest
None
Acknowledgement
Acknowledgements to Rare tumours, Journal of Cancer Research and Therapeutics (JCRT), and Clin Med Oncol for granting copy right permission for reproduction of figures from their Journals to be reproduced under the Creative Commons Attribution License provided the original work is properly cited.
References
- Zhou Y, Tang Y, Tang J, et al. Primary adrenal leiomyosarcoma: a case report and review of literature. Int J Clin Exp Pathol. 2015;8(4): 4258–63.
- Gellert LL. Adrenal gland and paraganglia: Other adrenal malignancies Leiomyosarcoma. PathologyOutlines.com, Inc. 2016.
- Kanthan R, Senger JL, Kanthan S. Three Uncommon adrenal incidentalomas: a 13-year surgical pathology review. World J Surg Oncol. 2012;10: 64.
- Mohanty SK, Balani JP, Parwani AV. Pleomorphic leiomyosarcoma of the adrenal gland: case report and review of the literature. Urology. 2007;70(3): 591.
- Choi SH, Liu K. Leiomyosarcoma of the adrenal gland and its angiographic features: a case report. J Surg Oncol. 1981;16(2):145–8.
- Linos D, Kiriakopoulos AC, Tsakayannis DE, et al. Laparoscopic excision of bilateral adrenal primary adrenal leiomyosarcomas in a 14-year-old girl with acquired immunodeficiency syndrome (AIDS). Surgery. 2004;136(5):1098 -100.
- Hamada S, Ito K, Tobe M, et al. Bilateral adrenal leiomyosarcoma treated with multiple local therapies. Int J Clin Oncol. 2009;14(4):356–60.
- Lujan MG, Hoang MP. Pleomorphic leiomyosarcoma of the adrenal gland. Arch Pathol Lab Med. 2003;127(1):e32 – 5.
- Kato T, Kato T, Sakamoto S, et al. Primary adrenal leiomyosarcoma with inferior vena cava thrombosis. Int J Clin Oncol. 2004;9(3):189–92.
- Gonzalez FAC, Chavez TV, Vazquez AC. Pleomorphic leiomyosarcoma of the adrenal gland with osteoclast-like giant cells. Endocr Pathol. 2005;16(1):75–81.
- Zetler PJ, Filipenko JD, Bilbey JH, et al. Primary adrenal leio