Research Article - Biomedical Research (2017) Volume 28, Issue 21
Preventive activities of Lactobacillus plantarum YS4 in oxazolone-induced BALB/c mice colitis
Yu Qian1,2,3, Ruokun Yi2,3, Peng Sun2,3, Guijie Li2,3* and Xin Zhao1,2,3*
1Beijing Advanced Innovation Center for Food Nutrition and Human Health, Beijing Technology and Business University (BTBU), Beijing, P.R. China
2Chongqing Collaborative Innovation Center for Functional Food, Chongqing University of Education, Chongqing, P.R. China
3College of Biological and Chemical Engineering, Chongqing University of Education, Chongqing, P.R. China
- *Corresponding Authors:
- Guijie Li
Chongqing Collaborative Innovation Center for Functional Food
Chongqing University of Education, PR China
Xin Zhao
College of Biological and Chemical Engineering
Chongqing University of Education, PR China
Accepted date: September 25, 2017
Abstract
The colitis preventive effects of Lactobacillus plantarum YS4 (LP-YS4) were determined by in vitro animal experiment in this study. The BALB/c mice were induced colitis by oxazolone, after inducing colitis, the preventive activities of LP-YS4 were measured using the serum and colon tissue. LP-YS4 (1.83) could significantly reduce (P<0.05) DAI of colitis in mice (3.47) at 25th day, inhibited colitis caused colon shortening and increase ratio of colon weight/length. LP-YS4 also could significantly decrease (p<0.05) the MPO, NO, MDA levels and increase GSH level of colon tissue in mice. Meanwhile, LP-YS4 significantly increased (P<0.05) IL-2 cytokine level and decrease IL-10 level in serum of mice compare to those levels of mice in control group. By RT-PCR assay, LP-YS4 raised nNOS, eNOS, c-Kit, SCF mRNA expressions and reduced iNOS, IL-8, CXCR2 expressions in colon tissue of mice compare to those expressions of mice in control group. From these results, LP-YS4 showed a anti-colitis effect of experimental mice.
Keywords
Lactobacillus plantarum, Oxazolone, Colitis, Chemokine receptor, Expression
Introduction
Ulcerative colitis (UC) is a kind of inflammatory bowel disease with the potential risk of carcinogenesis. The onset age is mainly between 20 and 50 years old, which seriously threatens people’s life quality [1]. The pathogenesis and treatment of UC is the focus of current researches while the important principle of controlling and curing UC is the discovery and the maintenance of the disease [2]. As drugs used in clinical treatment of UC can cause side effects after long term use, the search for functional foods with non-side effects in UC treatment is also an important aspect of UC research [3]. Current studies have showed that the intestinal flora is closely connected with UC, which is involved in mucosal immune response. As bacteria is one of the important trigger factors of inflammatory bowel disease, the UC can be relieved by regulating intestinal flora to prevent dysbacteriosis and increase the quantity of probiotics [4,5].
Kurut is a kind of natural fermented food which is common in Qinghai-Tibet plateau areas and rich in nutrition. Study has shown that kurut has many physiological activities, including antioxidation, lowering cholesterol and improving immunity [6]. The flavor and quality of Kurut is quite different from the ordinary fermented milk because of special natural fermentation environment of Qinghai-Tibet plateau region, unique fermentation vessels, especially special fermentation microorganism [7]. LP-YS4 used in this study is a Lactobacillus plantarum separated, purified and identified from Kurut from Yushu Tibetan Autonomous Prefecture in Qinghai, which has good resistance to gastric acid and bile salt in vitro [8]. Preliminary study on the physiological activity of Lactobacillus in Kurut from Qinghai-Tibet plateau found that the separated Kurut Lactobacillus is anti-oxidative [9] and can prevent constipation [8]. In this study, LP-YS4 is taken as the research object to observe its prevention of oxazolone-induced colitis for the first time. The results will provide certain theoretical basis for the further development of LP-YS4, which is beneficial to the development and utilization of LP-YS4.
Materials and Methods
Microorganism strains
The isolation and identification of Lactobacillus plantarum was named Lactobacillus plantarum YS4 (LP-YS4), and this stain was preserved in China Center for Type Culture Collection (CCTCC NO: M2016749, Wuhan, China), and Lactobacillus bulgaricus (LB, CCTCC AB 200048) was also purchased from CCTCC.
Animal experiment
The 50 BALB/c male mice were randomly divided into 5 groups: normal group, model group, LB (Bulgarian Lactobacillus) treatment group, LP-YS4 low-concentration treatment group and LP-YS4 high-concentration treatment group, with 10 in each group. Normal group and model group were normally fed without other treatment while LB treatment group, LP-YS4 low-concentration treatment group and LPYS4 high-concentration treatment group were givin 2 mL by gavage respectively with the concentration of 1.0 × 109, 1.0 × 108 and 1.0 × 109 CFU/mL for 26 days. After the 15th day, the abdomen of all mice was shaved 2 cm × 2 cm. Then the shaved part of mice in normal group was smeared with 0.2 ml ethanol (99%) while the other groups of mice were smeared with 0.2 ml oxazolone solution (3% mass ratio and 99% ethanol as solution). On the 19th day, after 24 h fasting, the mice were anesthetized with 0.1 ml/10 g chloral hydrate, and then were inserted 3.5 cm deep into intestinal from the anus with a blunt silicone tube. Mice in normal group were injected with 0.15 ml 50% ethanol solution while mice in other groups were injected into 0.15 ml 1% oxazolone solution (mass ratio and 50% ethanol as solution). The catheters were pulled out after 20 s, and the mice were inverted for 30 s at the same time [10]. On the 26th day, all the mice were neck-broken to collect the plasma. Then took their colon tissues and measured the weight and length of the colon tissues. In the meanwhile, Disease activity index (DAI) was determined through the formula: DAI=(score of weight loss+score of defecate character+score of hematochezia)/3 (Table 1).
| Weight decrease (%) | Stool character | Hematochezia | Score |
|---|---|---|---|
| No decrease | Normal | Occult blood (-) | 0 |
| 1-5 | Semi sparse stool | Occult blood (-) | 1 |
| 6-10 | Semi sparse stool | Occult blood (+) | 2 |
| 11-15 | Sparse stool | Occult blood (+) | 3 |
| >15 | Sparse stool | Visible blood | 4 |
Table 1. DAI scoring standard.
Determination of the activities of MPO, GSH, MDA, SOD and NO level in colon tissues of mice
Clean colon tissues of mice were mixed with saline which was nine times heavier than the colon. Colon tissues were homogenized by using ultrasonic grinding and then the content of MPO, NO, GSH, MDA and SOD (Nanjing Jiancheng Bioengineering Institute, Nanjing, Jiangsu, China) in colon tissues of mice were determined according to instructions in the kit [11].
Determination of the levels of IL-2 and IL-10 cytokines in serum of mice
Serum of the mice was taken and then the levels of IL-2 and IL-10 cytokines in the serum of the mice were determined by ELISA method according to instructions in the kit (Abcam, Cambridge, MA, USA) [11].
Expression determination by RT-PCR
The colon tissues of the mice were homogenized and the total RNA was extracted from the colon after adding RNAzol (Thermo Fisher Scientific, Inc., Waltham, MA, USA). Then the total RNA concentration was diluted to 1 μg/μL. 2 μL diluted total RNA extraction was added in turn with 1 μL oligodT18, RNase, dNTP, MLV enzyme and 10 μL 5X buffer (Thermo Fisher Scientific) under the condition of 37°C 120 min, 99°C 4 min, 4°C 3 min in order to synthesize cDNA. And by the method of reverse transcription-polymerase chain reaction (RTPCR) (94°C 5 min for one time, 94°C 30 sec, 58°C 30 sec, 72°C 30 sec all for 30 times, 72°C 5 min for one time), the mRNA expression of nNOS (forward: 5'-GAA TAC CAG CCT GAT CCA TGG AA-3'; reverse: 5'-TCC TCC AGG AGG GTG TCC ACC GCA TG-3'), eNOS (forward: 5'-GGA GAG GCT GCA TGA CAT TG-3'; reverse: 5'-GGT AGA GCC ATA GTG GAA TGA C-3'), iNOS (forward: 5'-AGA GAG ATC GGG TTC ACA-3'; reverse: 5'-CAC AGA ACT GAG GGT ACA-3'), c-Kit (forward: 5'-AGA CCG AAC GCA ACT-3'; reverse: 5'-GGT GCC ATC CAC TTC A-3'), SCF (forward: 5'- AAA CTG GTG GCG AAT-3'; reverse: 5'-CAC GGG TAG CAA GAA-3'), IL-8 (forward: 5'-AGA AGC ATG GCC CAG AAA TCA-3'; reverse: 5'-GGC CTT GTA GAC ACC TTG GT-3') and CXCR2 (forward: 5'-GAA CAA AGG CAA GGC TAA-3'; reverse: 5'-AAC ATA ACA ACA TCT GGG CA-3') (Thermo Fisher Scientific) were amplified, with housekeeping gene GAPDH (forward: 5'-CGG AGT CAA CGG ATT TGG TC-3'; reverse: 5'-AGC CTT CTC CAT GGT CGT GA-3') as internal parameters. In the end, the PCR amplification products were examined with 1% ethidium bromide agar electrophoresis and was performed the semi-quantitative analysis using Image1.44 software (National Institutes of Health, Bethesda, MD, USA) [11].
Statistical analysis
All the experiments were repeated three times to get the average as the final results. The collected data were compared with data at P<0.05 level to see whether they have significant differences using SAS9.1 statistical software and the one-way ANOVA method to analyze.
Results
DAI score, colon length and weight of mice
According to Table 2, after the mice were given oxazolone by lavage, the DAI value of the mice in model group has gradually increased, and was significantly higher than that of the other 4 groups (P<0.05). At the same time, the experimental results showed that the colonic length and the ratio between colon length and weight of the mice in the LPYS4 high-concentration treatment group were significantly higher than that of the model group but slightly lower than that of the normal group (Table 3).
| Group | 20th day | 22th day | 25th day |
|---|---|---|---|
| Normal | 0.00 ± 0.00e | 0.00 ± 0.00e | 0.00 ± 0.00e |
| Model | 2.35 ± 0.25a | 3.02 ± 0.21a | 3.47 ± 0.26a |
| LB | 1.77 ± 0.22b | 2.02 ± 0.25b | 2.21 ± 0.22b |
| LP-YS4-L | 1.65 ± 0.22c | 1.82 ± 0.21c | 1.95 ± 0.27c |
| LP-YS4-H | 1.42 ± 0.23d | 1.61 ± 0.19d | 1.83 ± 0.23d |
Table 2. DAI score of different group mice.
| Group | Colon length (cm) | Colon weight/colon length (mg/cm) |
|---|---|---|
| Normal | 9.1 ± 0.4a | 41.1 ± 2.8a |
| Model | 3.0 ± 0.5e | 10.8 ± 1.0e |
| LB | 5.1 ± 0.6d | 24.3 ± 1.9d |
| LP-YS4-L | 6.3 ± 0.5c | 27.6 ± 2.1c |
| LP-YS4-H | 8.0 ± 0.6b | 36.6 ± 2.2b |
Table 3. The colon length and ratio of colon weight/colon length of different group mice.
Colon tissue levels of mice
As can be seen from Table 4, MPO, MDA activities and NO level in the colon tissues of the model group were the highest, while GSH activity the lowest. Compared with the model group, LB and LP-YS4 lavage can reduce MPO, MDA activities and NO level in colon tissues of colitis mice and improve the level of GSH activity. Besides, high-concentration LP-YS4 (LP-YS4-H) had the strongest effect, making the MPO, MDA activities and NO level just higher than that of the normal group and GSH activity just second to the normal group.
| Group | MPO (mU/mg) | NO (μmol/gprot) | GSH (µmol/mg) | MDA (nmol/mg) |
|---|---|---|---|---|
| Normal | 6.49 ± 0.28e | 0.29 ± 0.05e | 8.52 ± 0.47a | 0.36 ± 0.07e |
| Model | 34.17 ± 2.08a | 3.17 ± 0.44a | 2.15 ± 0.35e | 1.52 ± 0.28a |
| LB | 21.01 ± 2.28b | 2.67 ± 0.40b | 4.32 ± 0.42d | 1.07 ± 0.22b |
| LP-YS4-L | 15.41 ± 1.17c | 1.82 ± 0.25c | 5.51 ± 0.28c | 0.82 ± 0.18c |
| LP-YS4-H | 9.92 ± 0.55d | 1.11 ± 0.18d | 6.71 ± 0.26b | 0.66 ± 0.16d |
Table 4. The MPO, NO, GSH and MDA levels in colon tissue of different group mice.
Cytokine levels in serum of mice
According to Table 5, the IL-2 level in serum of the model group was the lowest while IL-10 the highest. After the mice were given Lactobacillus by lavage, the IL-2 level in serum of both LB and LP-YS4 groups were significantly increased, while the IL-10 levels were significantly reduced, and highconcentration LP-YS4 (LP-YS4-H) was better.
| Group | IL-2 (pg/ml) | IL-10 (pg/ml) |
|---|---|---|
| Normal | 219.67 ± 32.31a | 116.41 ± 12.36e |
| Model | 70.36 ± 12.20e | 977.21 ± 25.47a |
| LB | 105.35 ± 17.48d | 714.25 ± 21.39b |
| LP-YS4-L | 135.20 ± 18.71c | 536.47 ± 24.48c |
| LP-YS4-H | 180.35 ± 20.84b | 278.26 ± 23.74d |
Table 5. The cytokine IL-2 and IL-10 levels in serum of different group mice.
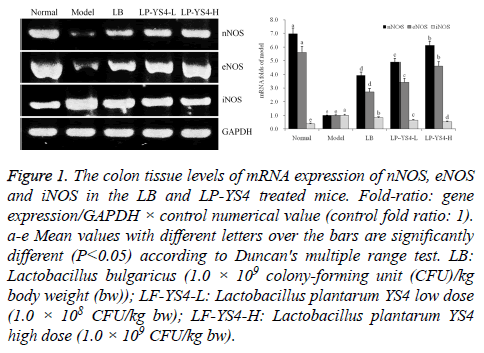
Colon tissue expression of nNOS, eNOS and iNOS in mice
According to Figure 1, compared to the model group, the expression of nNOS and eNOS in the colon of LP-YS4 and LB treatment group were higher (P<0.05), while the expression of iNOS was lower, and high-concentration LP-YS4 (LP-YS4-H) had better effect.
Figure 1: The colon tissue levels of mRNA expression of nNOS, eNOS and iNOS in the LB and LP-YS4 treated mice. Fold-ratio: gene expression/GAPDH × control numerical value (control fold ratio: 1). a-e Mean values with different letters over the bars are significantly different (P<0.05) according to Duncan's multiple range test. LB: Lactobacillus bulgaricus (1.0 × 109 colony-forming unit (CFU)/kg body weight (bw)); LF-YS4-L: Lactobacillus plantarum YS4 low dose (1.0 × 108 CFU/kg bw); LF-YS4-H: Lactobacillus plantarum YS4 high dose (1.0 × 109 CFU/kg bw).
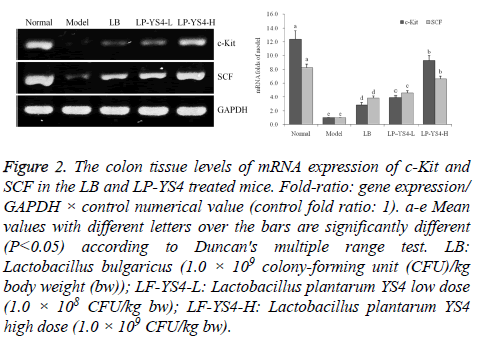
Colon tissue expression of c-Kit and SCF in mice
According to Figure 2, compared to the model group, LB and LP-YS4 can significantly up-regulate the expression of c-Kit and SCF mRNA (P<0.05), and the expression of c-Kit and SCF in LP-YS4 high-concentration (LP-YS4-H) group were significantly higher than the other groups except the normal group (p<0.05).
Figure 2: The colon tissue levels of mRNA expression of c-Kit and SCF in the LB and LP-YS4 treated mice. Fold-ratio: gene expression/ GAPDH × control numerical value (control fold ratio: 1). a-e Mean values with different letters over the bars are significantly different (P<0.05) according to Duncan's multiple range test. LB: Lactobacillus bulgaricus (1.0 × 109 colony-forming unit (CFU)/kg body weight (bw)); LF-YS4-L: Lactobacillus plantarum YS4 low dose (1.0 × 108 CFU/kg bw); LF-YS4-H: Lactobacillus plantarum YS4 high dose (1.0 × 109 CFU/kg bw).
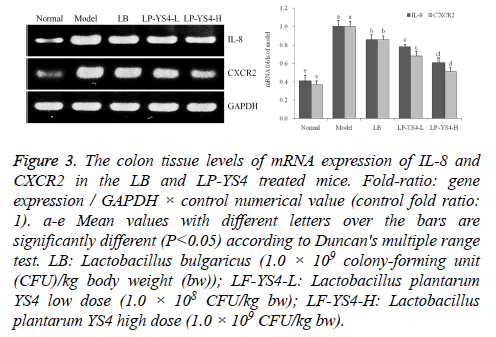
Colon tissue expression of IL-8 and CXCR2 in mice
According to Figure 3, the expression of IL-8 and CXCR2 mRNA of LP-YS4 high-concentration (LP-YS4-H) group were significantly higher than the other groups except the normal group (P<0.05), and the expression of LP-YS4 lowconcentration (LP-YS4-L) treatment group was similar to that of LB group, which was lower than the model group.
Figure 3: The colon tissue levels of mRNA expression of IL-8 and CXCR2 in the LB and LP-YS4 treated mice. Fold-ratio: gene expression / GAPDH × control numerical value (control fold ratio: 1). a-e Mean values with different letters over the bars are significantly different (P<0.05) according to Duncan's multiple range test. LB: Lactobacillus bulgaricus (1.0 × 109 colony-forming unit (CFU)/kg body weight (bw)); LF-YS4-L: Lactobacillus plantarum YS4 low dose (1.0 × 108 CFU/kg bw); LF-YS4-H: Lactobacillus plantarum YS4 high dose (1.0 × 109 CFU/kg bw).
Discussion
Colitis can result in weight loss, diarrhea and bleeding. As DAI is scored by weight, fecal traits and hematochezia, it can be used to measure the degree of colitis [12]. The DAI index shows that LP-YS4 can relieve the symptoms of oxazoloneinduced colitis and the effect becomes more obvious as the concentration increases. Colon length and the ratio between colon weight and length are also standards to measure degree of colitis. Compared with normal mice colon, colon length of mice with colitis is shorter and the ratio between colon weight and length is much lower [13].
The increased activity of MPO (myeloperoxidase) in colon shows that the aggregation of neutrophils in inflammatory tissues decreased [14]. During the process of colon inflammation, iNOS can form NO which wil aggravate the lesion of the colonic tissues. As the content of NO increases, the activity of MPO also increases, making the inflammation worse [3]. Colitis can also produce a large number of ROS (reactive oxygen species) and RNS (reactive nitrogen species), which can trigger oxidative stress toxicity, which can cause inflammation of the colon tissues [15]. After the inflammation reaction, the generation of lots of ROS will destroy the balance between oxidants and antioxidants in body and reduce the content of GSH in colon tissues. Besides, large number of lipid peroxidations can increase the production of its end product MDA [16].
Oxazolone-induced colitis is a kind of inflammation mediated by Th2 cells. The mechanism of the inflammation is that the imbalance of Th1/Th2 immune network leads to colitis. Cytokine IL-2 and IL-10 are produced respectively by Th1 and Th2 cells, which are directly related to colitis. Excessive low level of IL-2 and high level of IL-10 show the deepening of colitis [17].
NOS are divided into neural NOS (nNOS), endothelial NOS (eNOS) and inducible NOS (iNOS). Studies have confirmed that NO produced by eNOS is the key to controlling the damage of colon tissues, because excessive NO produced by iNOS has fastened the colon inflammation damage, and the down-regulation of nNOS also makes the expression of iNOS stronger and releases a large number of NO [18].
Ulcerative colitis shows not only the symptoms of diarrhea and hematochezia, but also colon motor disorder. Studies have shown that ICC (Interstitial cells of Cajal) is connected with colon motor, thus directly involved in the process of colitis [19]. In inflammatory bowel diseases, SCF has direct effect to maintain the number and function of ICC, because it is the natural ligand of c-Kit. If SCF/Kit signals are damaged, the proliferation and differentiation of ICC will decrease, thus aggravating colitis [20].
IL-8 has inflammatory activity and chemotaxis. CXCR is the receptor of IL-8. IL-8 and CXCR2 are connected with the incidence of colon cancer, and studies have also confirmed that the expression of IL-8 and CXCR2 will become higher in colon cancers [21]. And this study also got similar results, the colitis mice showed the stronger IL-8 and CXCR2 expressions than normal mice, and LP-YS4 could reduce these expressions in colitis mice.
Conclusion
According to research on the inhibition of LP-YS4 on oxazolone-induced colitis in mice, the experimental results showed that LP-YS4 could significantly (P<0.05) reduce DAI of colitis mice, inhibit the shortening of colon length caused by colitis and increase the ratio between colon weight and length. LP-YS4 could significantly (P<0.05 reduce the content of MPO, NO, MDA and the level of IL-10 in colon tissues of colitis mice and increase the content of GSH and the level of IL-2 in serum. The detection of mRNA level in the colon tissues also revealed that LP-YS1 could up-regulate the mRNA expression of nNOS, eNOS, c-Kit, SCF and down-regulate the expression of iNOS, IL-8 and CXCR2. As a result, LP-YS4 can effectively prevent oxazolone-induced colitis, which has the potential of probiotics development.
Acknowledgment
The present research was supported by Chongqing Research Program of Basic Research and Frontier Technology (cstc2016jcyjA0820) and Open fund of Beijing Advanced Innovation Center for Food Nutrition and Human Health, (20161001), China
References
- Shivakumar BM, Chakrabarty S, Rotti H, Seenappa V, Rao L, Geetha V, Tantry BV, Kini H, Dharamsi R, Pai CG, Satyamoorthy K. Comparative analysis of copy number variations in ulcerative colitis associated and sporadic colorectal neoplasia. BMC Cancer 2016; 16: 271.
- Sun FM. The pathogenesis of ulcerative colitis and therapeutic update. Guide China Med 2012; 10: 445-447.
- Sun YB, Liu KR, Chen GZ. Research progress of traditional Chinese medicine in treatment of ulcerative colitis. J Liaoning Univ Tradit Chinese Med 2015; 17: 222-224.
- Cui HL, Chen CL, Sun Y, Liu YH, Wang YD, Zhang YD, Yang YJ, Pan LJ. Changing of the flora and humoral immunofunction in patients with inflammatory bowel diseases. Chinese J Microecol 2003; 15: 151-155.
- Sun Y, Ding YQ. Changes of intestinal flora and pathology in ulcerative colitis. Mod Digest Inter 2009; 14: 26-28.
- Wu CS, Shu C, Li J, Qian Y, Suo HY. The research progress and prospect of Yak yogurt lactic acid bacteria. Food Ind 2012; 2012: 135-139.
- Wu CS, Li J, Qian Y, Suo HY. Research progress of Yak milk and fermented Yak milk and their nutritional value. J Dairy Sci Technol 2012; 35: 43-46.
- Qian Y, Suo H, Du M, Zhao X, Li J, Li GJ, Song JL, Liu Z. Preventive effect of Lactobacillus fermentum Lee on activated carbon-induced constipation in mice. Exp Ther Med 2015; 9: 272-278.
- Zhou XF, Yi RK, Zhao X. Skin anti-aging effect of mice of Lactobacillus fermentum Zhao. J Chongqing Univ Edu 2016; 29: 160-167.
- Wang X, Fan F, Cao Q. Modified Pulsatilla decoction attenuates oxazolone-induced colitis in mice through suppression of inflammation and epithelial barrier disruption. Mol Med Rep 2016; 14: 1173-1179.
- Feng X, Zhao X. Study on preventive effects of different vessels fermented Shuidouchi on CCl4 induced hepatic damage. Sci Technol Food Ind 2016; 37: 338-342.
- Wang Y, Liu L, Guo Y, Mao T, Shi R, Li J. Effects of indigo naturalis on colonic mucosal injuries and inflammation in rats with dextran sodium sulphate-induced ulcerative colitis. Exp Ther Med 2017; 14: 1327-1336.
- Strober W, Fuss IJ, Blumberg RS. The immunology of mucosal models of inflammation. Annu Rev Immunol 2002; 20: 495-549.
- Mustafa A, El-Medany A, Hagar HH, El-Medany G. Ginkgo biloba attenuates mucosal damage in a rat model of ulcerative colitis. Pharmacol Res 2006; 53: 324-330.
- Osman N, Adawi D, Ahrné S, Jeppsson B, Molin G. Probiotics and blueberry attenuate the severity of dextran sulfate sodium (DSS)-induced colitis. Dig Dis Sci 2008; 53: 2464-2473.
- Fiocchi C. Inflammatory bowel disease: new insights into mechanisms of inflammation and increasingly customized approaches to diagnosis and therapy. Curr Opin Gastroenterol 2004; 20: 309-310.
- Cheng Z1, Peng HL1, Zhang R2, Fu XM3, Zhang GS4. Bone marrow-derived innate macrophages attenuate oxazolone-induced colitis. Cell Immunol 2017; 311: 46-53.
- Vannucchi MG, Corsani L, Bani D, Faussone-Pellegrini MS. Myenteric neurons and interstitial cells of Cajal of mouse colon express several nitric oxide synthase isoforms. Neurosci Lett 2002; 326: 191-195.
- Li H, Lu ZH, Chen L, Lin L. Expression of interstitial cells of Cajal and stem cell factors in mice colon with ulcerative colitis. Acta Univ Med Nanjing (Nat Sci) 2009; 29: 648-651.
- Galli SJ, Tsai M, Wershil BK. The c-kit receptor, stem cell factor, and mast cells. What each is teaching us about the others. Am J Pathol 1993; 142: 965-974.
- Zhu F, Wang XB, Liu S, Wu T, Xia B. Expressions and significance of CXC chemokine receptor type 2 and interleukin-8 in patients with inflammatory. Chinese J Gastroenterol 2016; 21: 331-335.