Research Article - Journal of Clinical Ophthalmology (2021) Advancements in Treatment of Ocular Diseases
Prevention of relapse of surgically treated aqueous misdirection by combining primary posterior capsulectomy with irido-zonulo-hyaloido-vitrectomy.
Vanita Pathak-Ray1*, Gurcharan Singh2, Isha Gulati2
1Centre for Sight, Banjara Hills, Hyderabad, Telangana, India
2LV Prasad Eye Institute, Hyderabad, Telangana, India
- *Corresponding Author:
- Dr. V Pathak-Ray FRCS (Ed) FRCOphth (Lon)
Orcid ID no: 0000-0002-7830-283X Centre for Sight Road No 2 Banjara Hills Hyderabad, India 500034
Email: vpathakray@gmail.com
Accepted on 26 July, 2021
Citation: Pathak-Ray V, Singh G, Gulati I. Prevention of relapse of surgically treated aqueous misdirection by combining primary posterior capsulectomy with irido-zonulo-hyaloido-vitrectomy. J Clin Ophthalmol. 2021;5(S4):440-444.
Abstract
Purpose: To report the outcomes of Primary Posterior Capsulectomy (PPC) when combined with Irido-Zonulo-Hyaloido-Vitrectomy (IZHV) in the surgical management of Aqueous Misdirection (AM) to prevent relapse.
Methods: Retrospective, non-comparative and interventional case series reporting the outcomes of reformed and sustained deep anterior chamber, intraocular pressure (IOP), Anti-Glaucoma Medications (AGM), complications and Best Corrected Visual Acuity (BCVA) of AM management subsequent upon intervention. A fellowship trained glaucoma specialist managed all cases with IZHV and PPC with an anterior vitrector via various incisional approaches.
Results: Ten eyes of 9 patients with AM were treated with PPC during IZHV. AM occurred in 3 eyes intra-operatively in combined phaco-filtration surgery in Primary Angle Closure Glaucoma (PACG); rest occurred in the post-operative period. Mean age of patients was 56.4 ± 17 years and were followed up for a mean of 31.3 ± 17.9 months (median 32 months, range 12-66 months). All cases achieved reversal of AM; none developed relapse. Each had deepening of Anterior Chamber (AC), control of intraocular pressure (IOP in mmHg) (pre 38.8 mmHg ± 14.6 mmHg, 95%CI [28.3,49.2] vs. post 14.6 mmHg ± 2.5 mmHg, 95%CI [12.8,16.4]; p<0.001) and requirement for anti-glaucoma medication (mean number pre 3.1 ± 0.8, 95% CI [2.5,3.8] vs. post 0.4 ± 0.8, 95%CI [-0.2,1.0]; p<0.001) at last follow-up. No serious long-term complication occurred.
Conclusion: Primary posterior capsulectomy, when combined with IZHV, is an efficient means of ensuring complete hyaloidectomy, essential for preventing recurrence of AM. It can be successfully utilised by the anterior segment surgeon through multiple incisions with an anterior vitrector, thereby reducing burden on the resources and skills required in a vitreo-retinal procedure
Keywords
Aqueous misdirection, Malignant glaucoma, Irido-Zonulo-Hyaloido-Vitrectomy (IZHV), Primary Posterior Capsulectomy (PPC).
Introduction
Aqueous Misdirection (AM) or malignant glaucoma has been described after a myriad of procedures [1]. If surgical management is indicated, then in recent times, Irido-Zonulo- Hyaloido-Vitrectomy (IZHV) via the anterior route [2,3] has been favoured over Pars-plana Posterior Vitrectomy (PPV). This is especially so in pseudophakic eyes as the aim of surgical management to create a direct and unhindered communication between the aqueous and vitreous cavity, rendering the eye unicameral, can also be achieved via the anterior route. However, both these approaches are fraught with recurrence [4,5]. A simple technique of combining central primary posterior capsulectomy (PPC) with IZHV in AM management has aided in prevention of relapse in our series of ten eyes of nine patients.
Methods
This is a retrospective, non-comparative and interventional case series reporting the outcomes of reformed and sustained deep Anterior Chamber (AC), intraocular pressure (IOP), Anti- Glaucoma Medications (AGM), complications and Best Corrected Visual Acuity (BCVA) of the surgical management (IZHV with PPC) of aqueous misdirection.
Informed consent for surgery was obtained from all the eligible participants; the study adhered to the principles as laid down by the Declaration of Helsinki. Data was collected across 2 sites- Institutional Review Board (at LVPEI)/and an Independent Ethics Committee (S2J) approval was obtained for collection of data for complications of glaucoma surgery and its management.
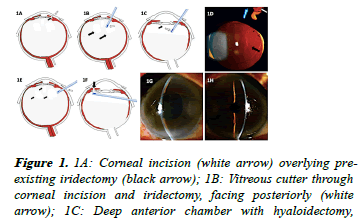
Routine IZHV was performed via any one of three incisional approaches–corneal if a pre-existing iridectomy was available (Figure 1A); a 23-gauge anterior vitrector was inserted through the patent iridectomy (Figure 1B) to perform a zonulectomy. The vitreous cutter initially faced the surgeon posteriorly (Figure 1B), and after zonulectomy, it was rotated anteriorly, until it was visible in the anterior vitreous. It is at this juncture that the Anterior Chamber (AC) started to deepen, marking the point of reversal of AM (Figure 1C). Anterior hyaloid face was then debulked and was deemed adequate when a central PPC was performed (Figures 1C-1D).
Figure 1. 1A: Corneal incision (white arrow) overlying preexisting iridectomy (black arrow); 1B: Vitreous cutter through corneal incision and iridectomy, facing posteriorly (white arrow); 1C: Deep anterior chamber with hyaloidectomy, vitreous cutter now facing anteriorly (white arrow); primary posterior capsulectomy (black arrow) also completed; 1D: Primary Posterior Capsulectomy performed intra-operatively and seen post-operatively on the slit lamp (black arrow) via retro-illumination technique; zonulectomy also visible (white arrow) through iridectomy; 1E: Pars plana stab incision (white arrow) and anterior vitrectomy when no antecedent iridectomy is available; 1F: Zonulectomy along with iridectomy (black arrow) is done at the opposite limbus via a posterior to anterior approach; 1G: Pre-operative flat anterior chamber in case 9 (Table 1) where pars plana anterior vitrectomy was done as no previous iridectomy was available; 1H: Postoperative deep anterior chamber in case 9 (Table 1).
If antecedent iridectomy was not available (Case 3 and 10, Table 1), then pars-plana anterior vitrectomy was done (Figure 1E) and zonulectomy along with iridectomy was via a posterior to anterior approach (Figure 1F), with deep AC postoperatively (Figure 1H) compared to pre-op (Figure 1G).
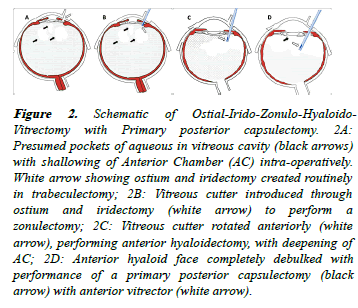
Figure 2. Schematic of Ostial-Irido-Zonulo-Hyaloido- Vitrectomy with Primary posterior capsulectomy. 2A: Presumed pockets of aqueous in vitreous cavity (black arrows) with shallowing of Anterior Chamber (AC) intra-operatively. White arrow showing ostium and iridectomy created routinely in trabeculectomy; 2B: Vitreous cutter introduced through ostium and iridectomy (white arrow) to perform a zonulectomy; 2C: Vitreous cutter rotated anteriorly (white arrow), performing anterior hyaloidectomy, with deepening of AC; 2D: Anterior hyaloid face completely debulked with performance of a primary posterior capsulectomy (black arrow) with anterior vitrector (white arrow).
If IZHV was performed intra-operatively in filtration surgery in a pseudophake or in combined phaco-filter, or soon thereafter, then the ostium and iridectomy created as part of trabeculectomy was taken advantage of (Figure 2) [6,7].
Results
We performed central PPC with IZHV in ten eyes of 9 patients. Seven patients were males and the ratio of right to left eye was 1:1. The mean age of patients was 56.4 ± 17 years and were followed up for a mean of 31.3 ± 17.9 months (median 32 months, range 12-66 months). AM occurred in 3 eyes intraoperatively in combined phaco-filtration surgery in Primary Angle Closure Glaucoma (PACG) or Plateau Iris Syndrome (PIS); all the rest occurred in the post-operative period. All the eyes that developed AM post-operatively (n=7), except one, were pseudophakic with intraocular lens (IOL) in the bag; the only phakic eye had lens extraction along with IZHV and PPC.
All the cases, summarised in Table 1, achieved reversal of AM with no relapse and long-lasting deepening of AC. There was significant reduction in mean intraocular pressure (IOP) (pre 38.8 ± 14.6 mmHg, 95%CI [28.3,49.2] vs. post 14.6 mmHg ± 2.5 mmHg, 95%CI [12.8,16.4]; p<0.001) and requirement for anti-glaucoma medication (mean number pre 3.1 ± 0.8, 95%CI [2.5,3.8] vs. post 0.4 ± 0.8, 95%CI [-0.2,1.0]; p<0.001) at last follow-up. All eyes were able to maintain pre-IZHV BCVA or showed improvement; two eyes with poor vision also maintained their vision (Table 1).
There were no intra-operative complications; one patient had choroidal exudation post-operatively. None developed a break or retinal detachment, which has been reported following a PPV [8]. Corneal decompensation, subluxation and/or dislocation of intraocular lens (IOL) also did not occur. Most notably, none of the eyes developed recurrence in the followup period.
Three representative cases highlighting the three incisional approaches are described here.
Case 1
An 84-year-old pseudophake, with very advanced and uncontrolled IOP, underwent a routine trabeculectomy with MMC. Post-operatively on day 1 his AC was very shallow, with an IOP of 19 mmHg; bleb was formed, with patent surgical PI. Atropine eye drops were commenced along with topical steroids and antibiotics. On day 5 post-operatively his AC was flat with an IOP of 31 mmHg; there was no choroidal detachment. Misdirection process was suspected, laser posterior capsulotomy and hyaloidotomy was not possible as he was unable to co-operate at the slit lamp for any length of time. The IOP did not respond to medical treatment, so he underwent ZHV and PPC (as described) under peribulbar block and sterile conditions 48 hours later, via the pre-existing ostium and patent iridectomy (Figure 2).
Post-operatively his AC remained deep and well-formed till last follow-up, almost a year after the procedure. His bleb was diffuse and well-formed with an IOP of 10 mmHg without AGM.
Case 2
A 48-year-old one-eyed pseudophakic man presented with flat AC on fifth post-operative day following routine Ahmed Glaucoma Valve (AGV, model FP7) surgery of the left eye. His past ocular history was significant for very advanced Juvenile Open Angle Glaucoma with failure of two filtration procedures. Prior to AGV surgery, VA was Light Perception (LP) with inaccurate projection and an IOP of 22 mmHg on 3 AGM and history of recent rapid deterioration in vision.
Day 5 post-operatively VA was LP+ and IOP was 47 mmHg; the AC was flat, and the tube was barely visible in the AC, having been engulfed by the iris. A large surgical PI was patent. Although he was atropinised immediately along with commencement of topical steroids, antibiotics and AGM, there was poor response to medical management. In view of his oneeyed status, IZHV with PPC was done within 2 days, through a corneal incision overlying the surgical iridectomy.
Post-IZHV and PPC on day 1, AC was deep with controlled IOP (14 mmHg) and good visibility of tube in the AC and remained so till last follow-up, He was referred to our Low Vision and Rehabilitation Services.
Case 3
A 71-year-old man presented with severe pain, redness and decreased vision in the right eye along with vomiting and headache of one-day duration. He had undergone AGV surgery 5 days ago for uncontrolled IOP in advanced Primary Angle Closure Glaucoma in a pseudophakic eye where cataract was extracted via Small Incision Cataract surgery several years ago.
BCVA in the right eye was count fingers, AC was uniformly flat, cornea was edematous with mid-dilated non-reactive pupil. The IOL was centrally placed and IOP was 60 mmHg. Although the view was hazy, indirect ophthalmoscopy failed to reveal any choroidal elevation. In view of pseudophakic status and uniformly flat AC, as opposed to iris bombe appearance of pupillary block (peripherally flat and relatively formed central AC) and absence of choroidal elevation, a diagnosis of aqueous misdirection was the most probable one, even in the absence of a patent peripheral iridotomy.
Medical management was initiated; laser iridotomy was considered but had to be abandoned for fear of endothelial decompensation as the iris was appositional with edematous cornea.
Following maximum medical therapy, both topical and systemic, IOP improved (18 mmHg after 5 days); however, AC continued to be uniformly flat as before and he was still very symptomatic. Hence, he underwent hyaloido-vitrectomy via a pars plana stab incision (Figure 1E) with PPC with an anterior vitrector; irido-zonulectomy was performed via a posterior to anterior approach (Figure 1F) as described above.
Post-operatively day one, he was comfortable and remarked on the disappearance of pain overnight. AC was deep, IOP controlled without AGM and visual recovery to pre-AM level (20/80) was achieved within a few weeks and was sustained over the follow-up period.
Discussion
Pars plana posterior vitrectomy and IZHV are effective means of reversing AM but both PPV [5,9] and IZHV [4] can be replete with recurrences. Madgula, et al. [4] experienced recurrence in 40% cases in their series of ten eyes that underwent IZHV, majority of which presented in the first 12 months, two eyes within the first week. Most of these recurrences appear to be due to blockage by vitreous, perhaps a reflection of incomplete hyaloidectomy. Zarnowski, et al. [10] have described peripheral capsulectomy with a vitreous cutter after initially creating a ‘tunnel’ with a knife through the iris and zonules. Our technique of central PPC with anterior vitrector affords greater control as it is performed under direct vision. Although, Zarnowski and colleagues did not encounter recurrence in their series of ten eyes, their follow-up is much shorter (one year).
We hypothesize that hyaloidectomy is incomplete unless one is able to perform a central PPC, and hence one of the key elements in the ill-understood mechanism of AM is insufficiently negotiated. As such, there is persistent risk of relapse in the post-operative period. We believe that this step is the reason why we did not encounter any recurrences in our series. Furthermore, no further recurrence occurred in case 5 (Table 1), who had presented with a relapse after PPV, described in details elsewhere [9].
| Gender | Age | Eye | Aetiology of glaucoma | Phakic status | Procedure inciting AMd | Timing of AM | Pre-procedure VA | Pre-procedure IOP mmHg | Follow-up in months | Re-lapse of AM | Last VA | Last IOP mm Hg | Last AGM |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 84 | OD | Pseudo-phakic | pseudo-phakia | Trab | Post-operative Day 5 | HM | 31 | 12 | Nil | HM | 10 | 0 |
| M | 48 | OS | JOAGa | pseudo-phakia | AGV (previous Trab X 2) | Post-operative Day 5 | LPf | 47 | 12 | Nil | LP | 14 | 0 |
| M | 71 | OD | PACGb | pseudo-phakia | AGV | Post-operative Day 5 | CFg | 60 | 38 | Nil | 20/80 | 12 | 0 |
| M | 29 | OD | PISc | phakic | Bleb repair | Post-operative week 3 | CF | 30 | 66 | Nil | 20/20 | 13 | 2 |
| F | 56 | OS | PACG | pseudo-phakia | AGV+PPVe (previous Phaco-trab) | Post-operative week 6 (relapse post PPV) | CF | 15 | 36 | Nil | 20/30 | 13 | 0 |
| M | 58 | OS | PACG | phakic | Phaco-Trab | Intra-operative | 20/40 | 56 | 21 | Nil | 20/40 | 16 | 2 |
| M | 58 | OD | PACG | phakic | Phaco-Trab | Intra-operative | 20/40 | 24 | 15 | Nil | 20/30 | 18 | 0 |
| M | 27 | OS | PIS | phakic | Phaco-Trab | Intra-operative | 20/125 | 38 | 54 | Nil | 20/63 | 16 | 0 |
| M | 70 | OD | Nil | Pseudo-phakia | Yag laser posterior capsulotomy | Post-laser Day 2 | CF | 68 | 24 | Nil | 20/50 | 15 | 0 |
| F | 63 | OS | PACb | Pseudo-phakia | Phaco | Post-operative Day 7 | 20/50 | 41 | 28 | Nil | 20/20 | 14 | 0 |
*JOAGa: Juvenile Open Angle Glaucoma; LPf: Light perception; PACGb: Primary Angle Closure/Glaucoma; CFg: Count fingers; PISc: Plateau Iris Syndrome; AMd: Aqueous Misdirection; PPVe: Pars Plana Posterior Vitrectomy
Table 1. Summary all cases undergoing Primary Posterior Capsulectomy (PPC) with Irido-Zonulo-Hyaloido-Vitrectomy (IZHV).
In summary, for prompt reversal of AM and for prevention of relapse, a complete anterior debulking of hyaloid and disruption of the hyaloid face is necessary, as ensured by a central PPC, along with IZHV. This is easily adaptable through various approaches by an anterior segment surgeon, without additional instrumentation and cost, thereby reducing burden on the resources and skills required in a vitreo-retinal procedure its and potential complications.
Conclusion
In conclusion, performance of primary posterior capsulectomy represents completeness of anterior hyaloidectomy in IZHV, a pre-requisite to prevent relapse in surgically treated Aqueous Misdirection.
Acknowledgments
Figures 1A-1C reproduced from Indian J Ophthalmol 2019;67:1204-6, ‘Management of recurrent aqueous misdirection by anterior segment surgeon after failed pars plana posterior vitrectomy.’ Authors Pathak Ray V and Malhotra V. Copyright 4865110014077 (9th July, 2020), with permission from Wolters Kluwer/MedKnow publications.
Figure 1D reproduced from Current Eye Research 2019 Oct; 44(10):1087-1090 ‘Intra-Operative Ostial Irido-Zonulo- Hyaloido-Vitrectomy with Primary Posterior Capsulectomy for Prevention of Post-Operative Aqueous Misdirection in Combined Phaco-Trabeculectomy in Primary Angle Closure Glaucoma.’ Authors Pathak Ray V, Gulati I, Choudhari N. Copyright 4854280982971 (22nd June, 2020) with permission from Taylor&Francis And J Cataract Refract Surg. 2019 Dec; 45(12):1826-1829. ‘Bilateral aqueous misdirection syndrome after routine cataract surgery in angle closure.’ Authors Pathak Ray V, Bansal A K, and Malhotra V. Copyright 4854280982971 (22nd June, 2020) with permission from Elsevier.
Figures 2A-2C reproduced from Current Eye Research 2019 Oct;44(10):1087-1090 ‘Intra-Operative Ostial Irido-Zonulo- Hyaloido-Vitrectomy with Primary Posterior Capsulectomy for Prevention of Post-Operative Aqueous Misdirection in Combined Phaco-Trabeculectomy in Primary Angle Closure Glaucoma.’ Authors Pathak Ray V, Gulati I, Choudhari N. Copyright: 4854310284966 (22nd June 2020) with permission from Taylor&Francis
Figure 2D is reproduced from J Cataract Refract Surg. 2019 Dec;45(12):1826-1829. ‘Bilateral aqueous misdirection syndrome after routine cataract surgery in angle closure.’ Authors Pathak Ray V, Bansal A K, and Malhotra V. Copyright 4854280982971 (22nd June, 2020) with permission from Elsevier.
Conflict of Interest
There are no conflicts of interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Shahid H, Salmon JF. Malignant glaucoma: A review of the modern literature. J Ophthalmol. 2012;2012:852659.
- Lois N, Wong D, Groenewald C. New surgical approach in the management of pseudophakic malignant glaucoma. Ophthalmology. 2001;108:780-3.
- Bitrian E, Caprioli J. Pars plana anterior vitrectomy, hyaloido-zonulectomy, and iridectomy for aqueous humor misdirection. Am J Ophthalmol. 2010;150:82-7 e1.
- Madgula IM, Anand N. Long-term follow-up of zonulo-hyaloido-vitrectomy for pseudophakic malignant glaucoma. Indian J Ophthalmol. 2014;62:1115-20.
- Debrouwere V, Stalmans P, Van Calster J, et al. Outcomes of different management options for malignant glaucoma: A retrospective study. Graefes Arch Clin Exp Ophthalmol. 2012;250:131-41.
- Tsai YY, Tseng SH. Combined trabeculectomy and vitrectomy for pseudophakic malignant glaucoma and extensive peripheral anterior synechia-induced secondary glaucoma. J Cataract Refract Surg. 2004;30:715-7.
- Pathak Ray V, Gulati, I, Choudhari, N. Intra-Operative Ostial Irido-Zonulo-HyaloidoVitrectomy with Primary Posterior Capsulectomy for Prevention of Post-Operative Aqueous Misdirection in Combined Phaco-Trabeculectomy in Primary Angle Closure Glaucoma. Curr Eye Res. 2019;44:1087-90.
- Al Bin Ali GY, Al-Mahmood AM, Khandekar R, et al. Outcomes of Pars Plana Vitrectomy in the Management of Refractory Aqueous Misdirection Syndrome. Retina. 2017;37:1916-22.
- Pathak Ray V, Malhotra V. Management of recurrent aqueous misdirection by anterior segment surgeon after failed pars plana posterior vitrectomy. Indian J Ophthalmol. 2019;67:1204-6.
- Zarnowski T, Wilkos-Kuc A, Tulidowicz-Bielak M, et al. Efficacy and safety of a new surgical method to treat malignant glaucoma in pseudophakia. Eye (Lond). 2014;28:761-4.