Research Article - Current Pediatric Research (2021) Volume 25, Issue 12
Prevalence of symptomatic hypocalcaemia in neonates in neonatal intensive care unit in al-Diwaniyah city
Qahtan Khayoon Hammod Alyasiri*
Department of Pediatric, College of Medicine, University of Al-Qadisiyah, Al Diwaniyah, Iraq
- Corresponding Author:
- Qahtan Khayoon Hammod Alyasiri
Department of Pediatric, College of Medicine, University of Al-Qadisiyah, Al Diwaniyah, Iraq
E-mail: abujamaljameel@gmail.com
Accepted date:24th December, 2021
Abstract
Objectives: To assess the prevalence of symptomatic hypocalcaemia in neonates in neonatal intensive care unit in al-Diwaniyah city. Patients and Methods: This cross-sectional analytical study was conducted at the neonatal intensive care unit of the maternity and children teaching hospital in Al Diwaniyah from January to May 2021. The total number of twenty-nine neonates with hypocalcaemia were included in this study from 709 neonates, admitted to the neonatal intensive care unit at the hospital. The parameters of newborns(age, gender, weight, the age of the newborn at the time of occurrence of hypocalcaemia, signs, and symptoms at diagnosis of hypocalcaemia, in addition to investigations of serum calcium in the blood). Results: Out of a total of 709 newborns treated at neonatal intensive care unit, hypocalcaemia was found in 29 subjects (4.01%), 72.4% of them were males and 27.6% were females, 58.6 of them was term and 41.4% was preterm, Age group at the firsts day of constituted 17.8% while the age group of 1-7 day constituted 17.2% and the age group more than 7 day was 13.8 %. Patients with serum calcium levels between 5-7 mg constituted 34.5% and between 7-8.1 mg/dl were 65.5%. Conclusion: The prevalence of symptomatic hypocalcaemia in neonates examined was 4.01%. Recommendation: more attention should be devoted to identifying risk factors, prevention, early identification, and metabolic support for sick newborns.
Keywords
Symptomatic hypocalcaemia, Neonatal intensive care unit, Al-Diwaniyah city.
Introduction
Hypocalcaemia is a frequently observed clinical and laboratory abnormality in neonates [1]. The etiology of hypocalcaemia varies with the time of onset and the associated illnesses of the child [2]. Neonatal hypocalcaemia is classified according to its onset to early-onset which manifests within the first 72 hours of birth and delayed onset after 3 days of birth [3]. Causes include prematurity maternal diabetes birth asphyxia fetal growth restriction and hyperparathyroidism [4-12]. Late hypocalcaemia usually occurs at the end of the first week of life but may occur earlier after the second or third day after birth [13]. The mechanisms for late neonatal hypocalcaemia are unclear but may represent a delayed response to the rise of PTH following hypocalcaemia [2,14]
Late hypocalcaemia is usually caused by high phosphate intake [15]. It is unclear whether vitamin D insufficiency (possibly caused by maternal vitamin D deficiency) has a causative role in late neonatal hypocalcaemia [13]. Most infants with hypocalcaemia are asymptomatic. If symptomatic, neuromuscular irritability is the most common sign with jitteriness, clonus, or seizures rarely, laryngospasm, wheezing or vomiting [16-18]. Infants may also be lethargic, eat poorly, vomit, and have abdominal distention [19]. For screening Calcium (Ca) levels are measured for at risk neonates including Very Low Birth Weight (VLBW) infants (BW<1500 g), those with congenital heart disease, and patients with symptoms consistent with hypocalcaemia [16]. The diagnosis is made by an abnormally low serum Ca value, which is defined by BW, if available, ionized Ca is the optimal test because this measurement most accurately assesses the risk of symptoms in all neonatal patient groups [16]. In term infants or preterm infants with BW>1500 g, hypocalcaemia is confirmed when the total serum Ca is less than 8 mg/dL (2 mmol/L) or an ionized fraction of less than 4.4 mg/dL (1.1 mmol/L) [20]. In VLBW preterm infants (BW<1500 g), hypocalcaemia is diagnosed when the total serum Ca is less than 7 mg/dL (1.75 mmol/L) or an ionized fraction of less than 4 mg/dL (1 mmol/L) [16]. Electrocardiography can show a prolonged QT interval [17]. In symptomatic patients, suggest providing initial parenteral Ca therapy as a 10% Ca gluconate solution at a dose of 100 mg/kg or 1 mL/kg (Grade 2C).
Further Ca supplementation is provided either parenterally or orally, if enteral feeds are tolerated. Infusion of Ca gluconate is associated with risks that must be weighed against the benefits of treatment [21]. Risks include bradyarrhythmias that can result from rapid elevations in serum Ca concentration, further evaluation is warranted if infants have persistent early hypocalcaemia that does not respond to dietary treatment, develop late hypocalcaemia, or have associated seizures [21].
Methods and Patients
This is a cross-sectional analytical study conducted at the neonatal care unit of the maternity and children teaching hospital in Al-Diwaniyah city. It was carried out over 3 months, from January to May 2021. The total number of twenty-nine newborns with symptomatic hypocalcemia was included in this study of 709 neonates in this period.
Inclusion criteria: Neonates under 28 days of life seek neonatology patient clinic medical care
The exclusion criteria: were infants with missing or incomplete data and infants older than 28 day
Data collection: Data were collected by interviewing mothers using a pre-prepared and pretested structured Arabic questionnaire include the age of newborns, sex, weight, maturity, early hypocalcemia (during the first three days of life), and late hypocalcemia (after 72 hours) were obtained. And symptoms of hypocalcemia which include (lethargy, poor feeding, and history of fit). Hypocalcemia is defined as a calcium level less than 8.0 mg/dl also patients were divided according to the severity of hypocalcemia, to those who had serum calcium levels less than 7 mg/dl and those who had serum calcium levels between 7-8.2 mg/dl. Informed consent was obtained from each participant. Patients' data were kept confidential. Ethics approval for the study was obtained from the pediatrics department of Al-Qadisiyah University of medical faculty.
Statistical analysis
The data obtained were analyzed using SPSS software version 19.0 for Windows (SPSS), chi-square, and Fisher's test were used where applicable. P values of less than 0.05 were considered statistically significant.
Results
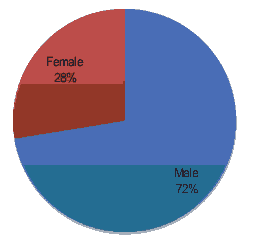
In our study, the total patients seen during 3 months period taken from 26.1.2021 to 08.5.2021 were 709 neonates the prevalence of symptomatic neonatal hypocalcemia among was 4.1% (twenty-nine cases). Twenty-one (72.4%) were male and eight of them female (27.5%) as shown in Figure 1.
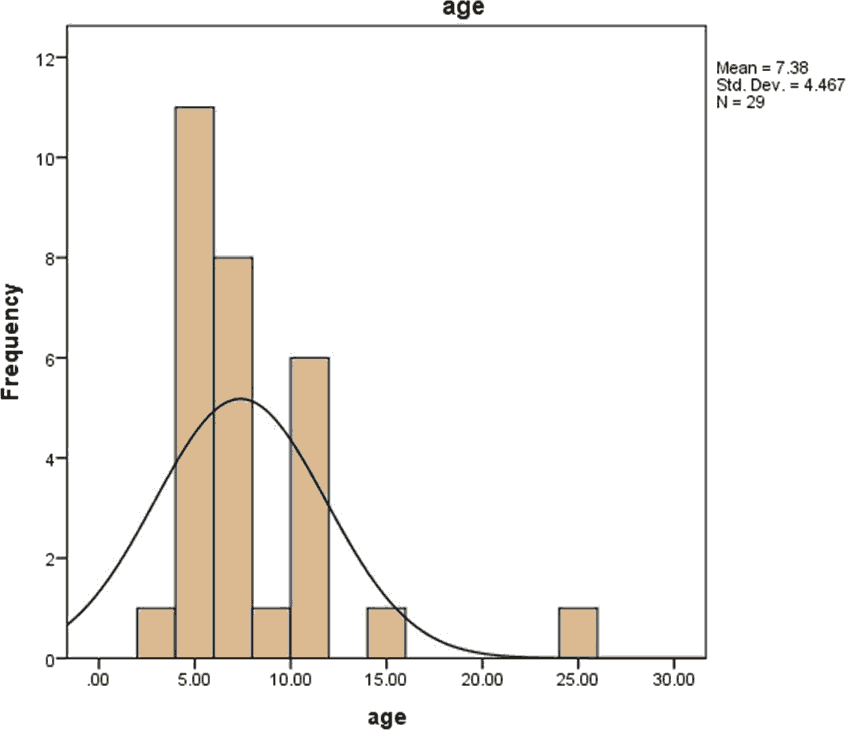
As for the gestational age of the seventeen (58.6%) were term and twelve (41.4%) were preterm. Patient’s age was ranged from 1-28 days and their mean age them was (7.3793 days) as shown in the nomogram in Figure 2.
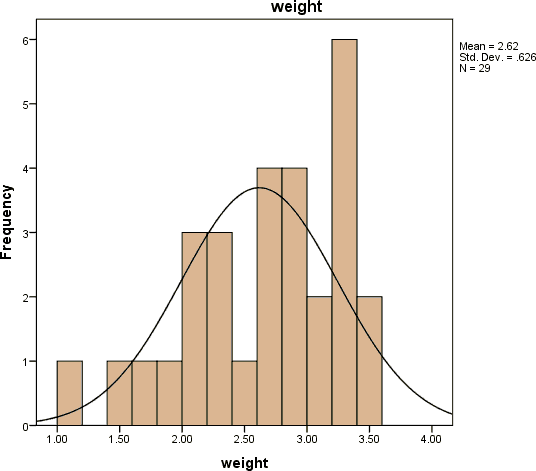
Their weight range from 1.10 kg to 3.50 kg and their mean age was 2.6172 kg as shown in Figure 3.
According to time of onset of symptomatic hypocalcemia, 14 cases (48.3%)had early hypocalcemia, while 15 (51.7%) had late hypocalcemia, We recorded twenty-three cases (79.3%) of them as lethargic, eighteen (62.1%) of them were poor feeding and three cases (10.1%) presented with convulsion as shown in Table 1.
| Variables | Hypocalcemia | P-value | ||
|---|---|---|---|---|
| Early (n=14) | Late (n=14) | |||
| Gender | Male | 12 (85.7%) | 9 (60%) | 0.122 |
| Female | 2 (14.3%) | 6 (40%) | ||
| Maturity | Term | 6 (42.9%) | 12(80%) | 0.94 |
| Preterm | 8 (57.1%) | 3 (20%) | ||
| Poor feeding | Yes | 7 (50%) | 11 (73.3%) | 0.36 |
| No | 7 (50%) | 4 (26.7%) | ||
| Lethargy | Yes | 10 (71.4%) | 13 (86.7%) | 0.31 |
| No | 4 (28.6%) | 2 (13.3%) | ||
| Convulsion | Yes | 2 (14.3%) | 1 (6.7%) | 0.5 |
| No | 12 (85.7%) | 14 (93.3%) | ||
Table 1. Frequency early and late hypocalcemia.
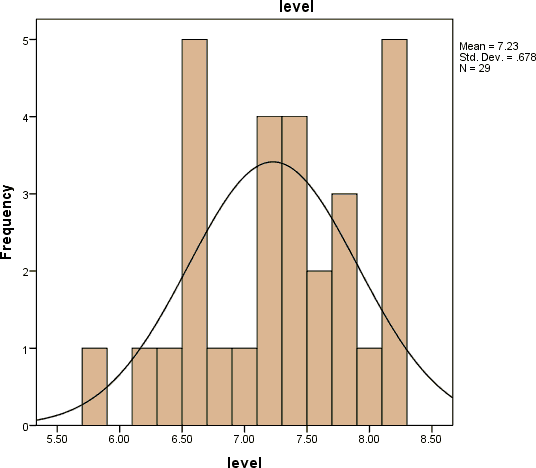
The neonatal serum calcium level distribution was between 5.8 to 8 mg/dl and the mean level of serum calcium was 7.2276 mg/dl as shown in Figure 4.
There was no statistically significant association/ statistical association between the date of onset of hypocalcemia and sex, gestational age, lethargic neonates, or poor feeding and Convulsion, Similarly, there was also no statistically significant positive correlation between serum calcium level and birth weight.
Discussion
Our objective in this study was to determine the prevalence of symptomatic neonatal hypocalcemia and the frequency of early and late neonatal hypocalcemia. The current study revealed that the prevalence of neonatal hypocalcemia was 4.01%, compared to other studies in Jordan was 2.7% [22]. but these result was much lower if compared to other studies conducted in Yemen (18%) Kenya (21.5%) while 33.5% in Iran and we think because we took only symptomatic hypocalcemia in our study while in those studies they conducted symptomatic and asymptotic neonatal hypocalcemia in our study we recorded Late hypocalcemia was more frequent (51.7%) than early hypocalcemia (48.3%)in the current study [3,23,24].
This result is in agreement with a study conducted in Egypt with 63.8% late hypocalcemia but this result was not consistent with other studies conducted in Tehran, Iran, the frequency of hypocalcemia in infants was 63% for early hypocalcemia and 37% for late hypocalcemia also In another study in 2018 in Amritsar, India, it was reported that 55% had early hypocalcemia and 45% had late hypocalcemia [25-27].
Our research showed that incidence rates were higher in the newborn with gestational age >37 weeks was 58.6% this result is in agreement with a study conducted in Algeria [28]. But another study in Iran shows a high percentage of hypocalcemia was detected in premature infants from 28 to 32 gestational weeks [29]. Regarding the risk factors of newborns involved in the study, our research has shown that a greater number of newborns had a male gender which is in agreement with the findings of other studies in Jordan and Egypt [1,5]. and birth weight between 1100 g and 3500 g comparable with another study conducted in Bosnia and Herzegovina was birth weight between 2500 g and 3500 g According to this same study, the most common age of the newborn at the time of occurrence of hypocalcemia was within the first 24 hrs of life, while our research showed that hypocalcemia is most common in the eighth day of life, and in another study conduct in South Korea showed that the most common age in the third day of life [30,31].
Our research has shown that a greater number of newborns had lethargic about 79.3%, poor feeding was 62,1% and convulsion only three cases which is not in agreement with other studies conducted in Jordan and Iran that noted Seizures were the most common symptom in neonatal hypocalcemia [32,33].
Conclusion
•The prevalence of neonatal hypocalcemia in the study population was 29 (4.01%).
•Hypocalcemia was more in males in comparison with females, also was more in neonate followed by gestational age more than 37 weeks.
•It was observed that more newborns were diagnosed with late-onset hypocalcemia compared to early-onset hypocalcemia. The most common age of hypocalcemia was the eighth day of life.
Recommendations
The recommended the implementation of preventative strategies as an effective public health measure for maternal and neonatal health care programs through:
•Calcium supplementation should be offered during pregnancy and Lactation.
•Routine investigations of serum calcium as a part of maternal and child health care program for early detection and management of neonatal hypocalcemia to supplement those with deficiency.
•Neonatal calcium levels should also be monitored to intervene in cases of neonatal hypocalcemia.
•Health education program to raise awareness about healthy and dietary lifestyles.
References
- Jain A, Agarwal R, Sankar MJ, et al. Hypocalcemia in the newborn. Indian J Pediatr 2010; 77(10): 1123-8.
- Marcdante KJ, Kliegman RM. Nelson essentials of pediatrics. (7th edn) Elsevier 2015.
- http://erepository.uonbi.ac.ke/handle/11295/15748.
- Tsang RC, Light IJ, Sutherland JM, et al. Possible pathogenetic factors in neonatal hypocalcemia of prematurity. The role of gestation, hyperphosphatemia, hypomagnesemia, urinary calcium loss, and parathormone responsiveness. J Pediatr 1973; 82(3): 423-9.
- Venkataraman PS, Tsang RC, Steichen JJ, et al. Early neonatal hypocalcemia in extremely preterm infants. High incidence, early onset, and refractoriness to supraphysiologic doses of calcitriol. Am J Dis Child 1986; 140(10); 1004-8.
- Rosenn B, Miodovnik M, Tsang R. Common clinical manifestations of maternal diabetes in newborn infants: implications for the practicing pediatrician. Pediatr Ann 1996; 25(4): 215-22.
- Schwartz R, Teramo KA. Effects of diabetic pregnancy on the fetus and newborn. Semin Perinatol 2000; 24(2): 120-35.
- Tsang RC, Chen I, Hayes W, et al. Neonatal hypocalcemia in infants with birth asphyxia. J Pediatr 1974; 84(3): 428-33.
- Venkataraman PS, Tsang RC, Chen IW, et al. Pathogenesis of early neonatal hypocalcemia: Studies of serum calcitonin, gastrin, and plasma glucagon. J Pediatr 1987; 110(4): 599-603.
- Spinillo A, Capuzzo E, Egbe TO, et al. Pregnancies complicated by idiopathic intrauterine growth retardation. Severity of growth failure, neonatal morbidity and two-year infant neurodevelopmental outcome. J Reprod Med 1995; 40(3): 209-15.
- Kramer MS, Olivier M, McLean FH, et al. Impact of intrauterine growth retardation and body proportionality on fetal and neonatal outcome. Pediatrics 1990; 86(5): 707-13.
- Tsang RC, Chen I, Friedman MA, et al. Parathyroid function in infants of diabetic mothers. J Pediatr 1975; 86(3): 399-404.
- Thomas TC, Smith JM, White PC, et al. Transient neonatal hypocalcemia: presentation and outcomes. Pediatrics 2012; 129(6): e1461-7.
- Allgrove J. The parathyroid and disorders of calcium metabolism. Clin Pediatr Endocrinol 2005; 254-79
- Venkataraman PS, Tsang RC, Greer FR, et al. Late infantile tetany and secondary hyperparathyroidism in infants fed humanized cow milk formula. Longitudinal follow-up. Am J Dis Child 1985; 139(7): 664-8.
- Abram S. Neonatal hypocalcemia. Wellesley 2021.
- Green JM, Enlow E. Clinical manifestations of diseases in the newborn period (hypocalcemia). Nelson textbook of pediatrics. (21st edn) Elsevier 2019; 910-3.
- Rubin LP. Disorders of calcium and phosporus metabolism. Avery's diseases of the newborn. (7th edn) WB Saunders 1998; 1189.
- Abrams SA, Tiosano D. Disorders of calcium, phosphorus, and magnesium metabolism in the neonate. Fanaroff and martin's neonatal-perinatal medicine (10th edn) Elsevier 2015.
- Kovacs CS, Lanske B, Hunzelman JL, et al. Parathyroid hormone-related peptide (PTHrP) regulates fetal-placental calcium transport through a receptor distinct from the PTH/PTHrP receptor. Proc Natl Acad Sci USA 1996; 93(26): 15233-8.
- Mimouni F, Tsang RC. Neonatal hypocalcemia: To treat or not to treat? (A review). J Am Coll Nutr 1994; 13(5): 408-15.
- Ayash FF, Alyassen AA, Khaled NEB, et al. The frequency of early and late neonatal hypocalcemia: Prince Zaid Bin Al-Hussein military hospital experience. J R Med Serv 2020; 27(1):25-36.
- BinMohanna M, Raja’a YA, Saif GA. Prevalence of hypocalcaemia in children examined for serum calcium in Sana'a, Yemen. Saudi Med J 2005; 26(3): 457-9.
- Behjati SH, Anjarani S, Rastegar H. The study of prevalence of neonatal hypocalcaemia. Iran J Pediatr 2003; 13(2): 141-6.
- Elsary A, Elgameel A, Mohammed WS, et al. Neonatal hypocalcemia and its relation to vitamin D and calcium supplementation. Saudi Med J 2018; 39(3): 247-53.
- Khalesi N, Namiranian P, Samavati S, et al. The frequency of early and late hypocalcemia among hospitalized newborns in an Iranian hospital. Shiraz E-Medical J 2015; 16(6): 16-18.
- Aggarwal K, Sandhu S, Narang GKG. Prevalence of neonatal hypocalcemia and its relation to supplementation. Int J Curr Res Biol Med 2018; 3(10): 43-47
- Benali A, Demmouche A. Calcium deficiency among pregnant women and their newborns in Sidi Bel Abbes region, Algeria. J Nutr Food Sci 2014; 4(6).
- Jain A, Agarwal R, Sankar MJ, et al. Hypocalcemia in the newborn. Indian J Pediatr 2010; 77: 1123-28.
- Raguz MJ, Bosnjak I. Frequency of neonatal hypocalcaemia and its correlation with risk factors. Clinics Mother Child Health. 2017; 14(4).
- Cho WI, Yu HW, Chung HR, et al. Clinical and laboratory characteristics of neonatal hypocalcaemia. Ann Pediatr Endocrinol Metab 2015; 20(2): 86-91.
- Tahmasebi S, Qasim MT, Krivenkova MV, et al. The effects of oxygen–ozone therapy on regulatory T‐cell responses in multiple sclerosis patients. Cell Biol Int 2021; 45(7): 1498-1509.
- Shabgah AG, Qasim MT, Mostafavi SM, et al. CXC chemokine ligand 16: A Swiss army knife chemokine in cancer. Expert Rev Mol Med 2021; 23: e4.