Research Article - Journal of Primary Care and General Practice (2020) Volume 3, Issue 3
Prevalence of Pressure Ulcer and Associated Factors Among Hospitalized Adult Patients in Public Hospitals Sidama Zone, South Nations, Nationalities, and Peoples Regional State, Ethiopia, 2017.
AAbiru Neme1*, Wadu Wolancho1, Gugsa Nemera1, Yosef Yohanes21Jimma University, Institute of Health, School of Nursing, Ethiopia
2Hawassa Health Sciences College, South Nations Nationalities, and Peoples’ Regional, Ethiopia
- *Corresponding Author:
- Abiru Neme
Negewo, Jimma University Institute of Health
School of Nursing, Ethiopia
Tel: 0965240864
E-mail: abiruneme@gmail.com
Accepted date: August 18, 2020
Citation: Neme A, Wolancho W, Nemera G, Yohanes Y. Prevalence of Pressure Ulcer and Associated Factors Among Hospitalized Adult Patients in Public Hospitals Sidama Zone, South Nations, Nationalities, and Peoples’ Regional State, Ethiopia, 2017. J Prim Care Gen Pract 2020:3(3):31-45.
Abstract
Background: On average, 60,000 people die each year worldwide due to pressure ulcer related causes. Even though, few studies reported the prevalence of pressure ulcer in some part of Ethiopia, there is paucity of information on the other side. Objectives: To Assess prevalence of Pressure Ulcer and Associated Factors Among Hospitalized Adult Patients in Public Hospitals in Sidama Zone; South Nations Nationalities, and Peoples? Regional State, Ethiopia, 2017. Methods: Institution based cross sectional study design was employed to assess pressure ulcer prevalence and associated factors in Sidama Zone from March13-April 12, 2017, On 356 subjects. Multistage sampling technique was employed to reach individual study subjects. Data was entered into EPI- data version 3.1 and was analyzed by using SPSS version 20 statistical software. Descriptive statistics, Bivariate and multivariate logistic regression were computed to assess statistical association using Odds Ratio. Significant of statistical association was assured or tested using 95% confidence interval and p value (<0.05). Results: A total of 56 Patients were Develop pressure ulcer from 356 admitted in Public Hospitals, with the prevalence rate of 15.7 %; from which 6 (1.7%), 34 (9.6%), and 16 (4.5%) were Medical Device Related Pressure Ulcers and Routine Pressure Ulcers .Patient who had No Position change by nurse were 4.53 times (95% CI: AOR, 4.346 (1.646 ? 11.473; P= 0.003) more likely to develop Pressure ulcer than Participants who had position change. Patients who had Body mass index Less than 18.5 kg/m2 were 6.9 times (95% CI: AOR, 6.91 (1.307,36.554) more likely to develop pressure ulcers than Patients who had BMI in between 25-29.99kg/m2. Conclusion and Recommendation: The Overall prevalence of pressure ulcer on this study is high. Position change, Activity, mobility, moisture, Antimicrobial, and ant diabetic were significantly associated with the development of pressure ulcer; Sidama Hospitals should Perform Risk and comprehensive assessment for all patients as soon as possible after admission, Provision of training for Nurses on Manual handling techniques when positioning and transferring patients, and if ,health condition patients permit nurses should reposition patient every two hours. Abstract
Keywords
Pressure ulcers, Risk factors, Prevalence, Sidama Zone
Introduction
A pressure ulcer is a localized injury to the skin and/or underlying tissue usually over a bony prominence, because of pressure, or pressure in combination with shear and/or friction [1-3]. Pressure ulcer also known as bed sore, pressure sore and decubitus ulcer [4].
Prolonged pressure impede capillary and venous return thus limit the delivery of oxygen and nutrients to tissue resulted with Metabolic wastes accumulation causes local vasodilatation [5,6], which contributes to edema compresses small vessels and ischemia prone patients at risk for pressure ulcer development [7,8].
Each year thousands of patients die of it and millions suffering from it in USA alone [9-13]. The number of patient suffering from PU is a few as 7.3% in hospitals in Europe and as high as 23% in North America [14-17], and 15.5% Malaysia [18-21].
Study reports in Africa revealed comparable magnitudes of pressure ulcer. In Nigeria it ranged from 3.22% to 18.6 % [4, 22]; whereas in Ethiopian hospitals it ranges from 13.4% to 16.8 % [23, 24].
A multicenter study in Brazil, prevalence of PU was 16.9%. Of which 16.3% patients had more than three PU [25]. Based on anatomical location; Sacral 82.5%, trochanter 37.5%, calcaneus 27.5%, Lumbar 6.3% and elbow 3.7% were the most affected. Whereas Patients presented with stage I 30.3 %, stage II 32.9 %, stage III 22.8 % and IV 13.9 % [26].
Pressure ulcer prevalence was 9% Study in the Republic of Ireland whereas 83% of the pressure ulcers were located on the sacrum. In terms of grade 33% were classified as grade II; but 24% were grade IV [20].
Cross-sectional study from different hospitals in Norway prevalence was 24 %. Stage I comprised most pressure ulcers, and the sacrum, ischial tuberosity, and heels, were the most common sites. Other ulcers were located on the feet, ears and back [25].
Cross-sectional survey in one university hospital and 11 general Hospital in China; prevalence was 1.58%, age of patients 40- 69 was almost half of study participant. Whereas 27.54% were aged over 70 years; the age of people with highest prevalence of pressure ulcer was more than 89 years. 52% of the pressure ulcers occurred in participants whose age between 70-89 years. Based on anatomical locations; Sacrum 60.22%, iliac crest 8.72%, heel 7.45%, trochanter 6.34%, ankle 4.91%, scapula 3.33%, ischial tuberosity 3.01%, Shoulder joint 0.79%, Elbow 0.79% and occiput 0.79% areas. Whereas stage I 28.68%, stage II 35.82%, stage III 12.68%, stage IV 12.99%, Unstageable 8.40%, and SDTI 1.43% [14].
Prospective observational study at the University of Malaya, Malaysia; prevalence of PU was 15.5%, of which 64.2% had a single pressure ulcer and 35.8% had pressure ulcers at more than one site. Stages Were, 64.2% stage II, 13.1% stage III, and 22.6% stage IV. Anatomical location: 72.3% were at the sacrum, 13.9% were at the trochanter and 13.9% were situated at the heel [21].
Survey in Nigeria in among 129 bed-ridden patients’ prevalence of Pressure ulcer was 18.6%; majority of patients with PU were male 91.7% and 8.3% female. Majority of patients who had pressure ulcer were the elderly patients above 65years 37.5% and those in the age range of 51-57 years 25%. Stages of Pressure were noted to be highest for Stages III 37.5%, and Stage IV 33.3%, and then low in Stage II 20.8% and Stage I 8.3%; location of pressure ulcers buttocks and sacrum 50% and 33.3% respectively [4]. Another study in the six university hospitals Nigeria, prevalence of PU was 3.22%, prevalence in the university hospitals ranged from 0% to 6.9%. The patients with a pressure ulcer were aged 16 to 86 years with a mean of 47.04±21.23 years. Prevalence rate based on gender; male and female patients were 3.59% and 2.83% respectively, whereas based on anatomical distribution 69.3% of the ulcers: ischium/ buttocks 43.6%; sacrum/coccyx 18.0%; and heel 7.7% [22].
Cross-sectional study in Ethiopia, Prevalence of pressure ulcer was 16.8%; higher in male respondents 42% than in female 29%. Based on Stages PU, stage I 62%, stage II 26.8% and stage IV 2.8%. From that developed pressure ulcer, most of the participants 70.4% developed sacral area and 10% patients at both sacral and shoulder area [23]. Another study in Wolaita Sodo Hospital Prevalence of pressure ulcer was 13.4%, higher among male Participant than female.
A cross-sectional survey study from 1100 patients, in the Republic of Ireland, 77% of the study participants was low risk of pressure ulcer development. However, individual scale of the Braden identified 53.5% were either completely immobile or had very limited mobility. Also, 51% was chair-fast and 7% bed-fast. 49% was incontinent of urine and feces, 78% having an adequate or an excellent nutritional status, of those with pressure ulcers [20].
A cross-sectional study in Norway different hospitals and community care sites, 32% were at risk for PU, There was a statistically significant association between having a pressure ulcer and being at risk using Braden (cut-off 18) (p < 0.001) [25].
Cross-sectional study in six long-stay institutions for the elderly in São Paulo, the Braden scale scores ranged from 7 to 19. According to the Braden scale, 67.5% of the patients were at high risk of pressure ulcer development [27].
Cross sectional point prevalence study in USA pressure ulcers was 5·4%. Of which 1·4% patients had at least one MDR pressure ulcer. The proportion of patients with hospital-acquired ulcers related to medical devices was 34·5%. Whereas Most MDR HAPUs were stage I 35%, stage II 32% however; it is important to note that 24% were unstageable and 3% were stage III, a full thickness ulcer. The most common locations of MDR HAPU were the ears 35%, lower leg 11% and heels 8% [19].
Study of two major metropolitan hospitals in Saudi Arabia in 84 patients, 33 patients was identified giving a HAPU incidence of 39.3%. A total of 41 HAPUs were recorded in 33 patients. The overall incidence of MDRPU was 8.3%. From the 41 HAPUs, 20% were related to medical devices, and the most common site was the ear 37.5% [28,29]. As to my knowledge Prevalence of medical device related pressure ulcer study was not done in the study area.
A cross-sectional study in South-Eastern Norway, There was no gender difference between patients with and without PUs (X2 = 0.862, p = 0.353); however, age 70 or above (X2 = 70.347, p < 0.001) differed significantly [7].
A cross-sectional study in Republic of Ireland, from completely immobile or had very limited mobility and chair-fast or bedfast. Both factors to be statistically significantly associated with pressure ulcer development (χ2 = 31.298, p < 0.0001; χ2 = 40.467, p < 0.0001, respectively). The association between pressure ulcers and nutritional status was noted to be statistically significant (χ2 = 9.409, p = 0.024). This association counters intuitive as it suggests that as nutritional status increases, so too does the number of pressure ulcers. Mobility and moisture are the highest predictors of pressure ulcer development and was statistically significant (β = -0.202, 95% CI = -0.100 to -0.023; p = 0.002; β = -0.121, 95% CI = -0.015 to -0.099; p = 0.008), respectively [20].
A cross-sectional study in Norway, there was a statistically significant association between having a pressure ulcer and being at risk using Braden (cut-off 18) (p< 0.001) [25].
Study in Kuala Lumpur Malaysia, from October 2012 to May 2013, Braden score ≤12 were 1.9 times (95% CI: 1.14, 3.19) more likely to develop pressure ulcer than those Braden score > 12 [21].
A community based cross-sectional study, Ethiopia, patient slightly limited in sensory perception, were 3.3 times (95% CI: 1.39, 7.75) at higher risk to develop pressure ulcer than those who had no impairment in sensory perception. And problem in friction and shearing forces were 4.5 times (95% CI: 1.56, 12.93) more likely to develop pressure ulcer than those who had no apparent problem [23].
Cross sectional study in Wolaita Sodo teaching hospital; patients with very limited sensory perception, friction and shearing and bedbound in activity were (AOR: 2.773; 95% CI: 1.244-4.64; P<0.05), (AOR: 2.28; 95% CI: 1.85-15.79; P<0.05), and (AOR: 2.34; 95% CI: 3.24- 4.13; P<0.05) respectively significant predictors of Pus [24].
Study among 84 Participants adult intensive care unit Saudi Arabian, the result illustrated infrequent repositioning were (AOR: 250.04; 95% CI: 5.230-11 954.16; P = 0.005) significant predictors of all stages of Pus [29].
Cross-sectional study among 422 hospitalized patients in Felegehiwot referral hospital, Ethiopia; position change was not significantly associated with PU in multivariate logistic regressions [23].
Multicenter, cross-sectional, study in hospitals in different geographic regions of Brazil, the result depicted that a length of stay in hospital stay between 8 days to 15days significant association with PU (OR 3.85; 95% CI: 1.53-9.73; P< 0.05) [26].
prospective observational study in Kuala Lumpur, the result Shows that Individuals with hospital acquired pressure ulcers had significantly longer duration of hospitalization (median [IQR] = 22 [12.75–34.50] vs. 15 [10.25–23] days; P = 0.032) [21].
Study done in two major metropolitan tertiary care hospitals Saudi Arabia; Length of stay in the ICU significant association with PU (OR: 1.23; 95% CI: 1.087–1.392; P = 0.001) [29].
Cross-sectional study in Felegehiwot referral hospital Ethiopia, length of stay in hospital greater than or equal to 21days was strongly associated with pressure ulcer development, 95% CI, AOR, 5.97(1.98,18.00) [23].
a population-based study from 15 general and tertiary care hospitals, in USA the result depicted that, Patients with BMI (in kg/m2) <19 reported a higher risk of PU (OR=3.07; 95% CI: 2.41, 3.91), but a lower risk in the BMI 25–30 (OR= 0.65; 95% CI: 0.53, 0.80) and ≥30 (OR= 0.52; 95% CI: 0.42, 0.64) [30].
study at a large private general hospital located in São Paulo, the results from the statistical analysis BMI and the development of PU were not statistically significant (p>0.05) [31].
Study in University Hospital João Pessoa, Brazil; PU statistically not associated with presence of Edema (p > 0.005) [2].
The sectional, quantitative study in University Hospital João Pessoa, Brazil; PU was statistically associated with the level of consciousness (p = 0.004) [2].
Cross sectional study in Wolaita Sodo Hospital south Ethiopia; PU significantly associated with Diabetes (AOR=4.116;95% (CI=2.135,6.884) [24].
Method and Materials
Study Setting
The study was conducted in public hospitals sidama Zone, from March13-April 12, 2017
Sidama zone is bordered in the south with Oromia region and Gedeo, in the West Bilate River which separate from North omo, and in the north and East by Oromia region. The administrative center for Sidama Zone is Hawassa; another town Includes Yirgalem, Wendo Genet, and Chuko. Hawassa is Located at the eastern shore of Lake Hawassa 276 KM south of Addis Abeba. Sidama zone has a population of 3,232,306 people in 23 districts with three city administrations. There were eleven hospitals found in sidama zone around 994 health care professionals [32].
Hawassa University comprehensive specialized Hospital (HUCSH), has 400 beds average of 65,000 peoples seen per year. This teaching hospital has 341 health care workers. In terms of Human power senior Physicians, General practitioners, Pharmacist, Laboratory Technicians, Nurses & Radiographers of 36, 30, 25, 32, 209 & 9, respectively.
Adare General Hospital is found center of the city under Hawassa city administration which is up graded from health center in 2004 EC and it has limited health professionals and hospital setting. has 131 beds, total of 365 Human power which includes 34 Nurses BSc, Nurses Diploma 83, Health Officer 6, General practitioners 22, Senior Physicians 4, Pharmacist 8, Pharmacy Technician 9, Lab technician 12, Lab technologist 12, Radiologist 1, and X-Ray technician 6.
Yirgalem General Hospital is found in sidama zone Dalle District, was built 1958 E.c by Norwegian king IV the total bed of the hospital 171, with total of 287 Human power, 60 Nurses, health officer 5, General practitioners16, Senior Physicians 8, Clinical Pharmacist 2, Pharmacist 8, Pharmacy technician 19, and X-Ray Technician 6.
Leku Hospital it is primary hospital, found in sidama zone Shebedino District, with the total of 66 bed, 149 Human power which includes 52 Nurses, Midwifes 11, Health Officer 5, GP 8, Lab Technologist and Lab technicians 12, Pharmacist 3, pharmacy technician 4, and x-ray technician 2.
Study design
Institution based cross sectional quantitative study design was employed to determined prevalence of pressure ulcer and to identify factors with Pressure ulcers in Public Hospital in Sidama Zone
Population
Source Population
All hospitalized patients in public hospitals, Sidama Zone.
Study Population
Sampled adult patients who were admitted in Medical, Surgical, Obs/Gyn, & ICU Wards in selected public hospitals in sidama Zone
Study Unit
Individual patients who were admitted on beds medical, surgical, Oby/Gyn & ICU wards
Inclusion and exclusion criteria
Inclusion Criteria
Adult Patients who were admitted in Medical, surgical, Oby/ Gyn, and ICU Greater than or Equal to 24 Hours
Exclusion criteria
Patients who developed pressure ulcer before admission.
Sample size and Sampling technique
Sample size
Sample size was determined by using single population proportion formula; the prevalence of pressure ulcers 16.8%. which was taken from Haileyesus Gedamu et al. done at Felegehiwot Referral Hospital, Bahir Dar, Ethiopia [23].
(n) Sample size at a Z-value of 1.96 with 95% CI and d of 5%:
n= (z α/2) 2 ρ(1-p)/d2
Where,
Z= 1.96, the confidence limits of the survey result (value of Z at α/2 or critical value for normal distribution at 95% confidence interval).
P= 0.168, the proportion pressure ulcer
d= 0.05, the desired precision of the estimate
n= the total sample size.
n= (1.96)2 0.168(1-0.168)/ (0.05)2
n=214.8
n=215
Considering a 10% nonresponse rate, the total sample size
215×10/100 = 21.5,215+21.5=237
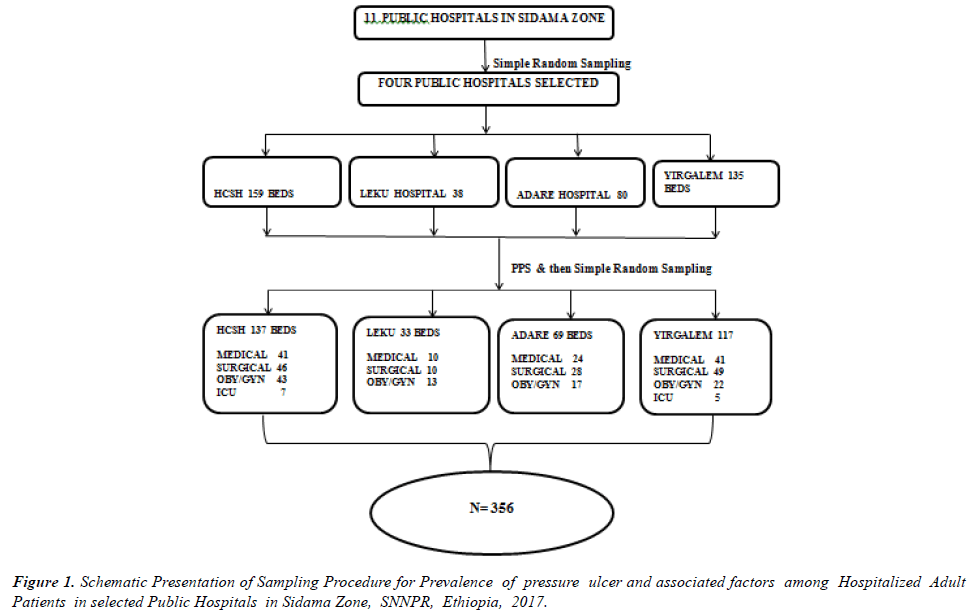
And calculating design effect (1.5) the final sample size was 356; Therefore, 356 patients was included in this study from selected public hospitals in sidama Zone Finally, the number of patients participating in each hospital was determined using the population proportionate sampling (PPS).
n= (nf × N)/ (N total)
Where, n = Proportion of patient participate in the study in each public hospital, nf = Final sample size (356), N=is the number of patient beds in medical, surgical, Oby/Gyn and ICU of each public hospital; N total = Total number of patient beds in all selected public hospitals (412) i.e.
1. Hawassa comprehensive Specialized Hospital=159, = 356 x 159 ̸ 412 = 137
2. Adare General Hospital=80, =356 x 80 ̸ 412 = 69
3. Yirgalem General Hospital= 135, =356 x 135 ̸ 412 = 117
4. Leku Hospital=38, =356 x 38 ̸ 3412 = 33
Sampling technique
Multistage sampling technique was employed Simple Random sampling (Lottery method) technique was employed to select four hospitals from eleven hospitals in sidama Zone; therefore Leku, Adare, Yirgalem and Hawassa comprehensive specialized hospital was selected [33,34].
Population Proportionate Sampling (PPS) was applied to get the total number of study participants from each hospital (Hawassa comprehensive Specialized Hospital 41, 46, 43,& 7 medical, surgical, Oby/Gyn & ICU wards respectively); Adare General Hospital 24, 28, & 17; medical, surgical & Oby/Gyn wards respectively; Yirgalem General Hospital 41, 49, 22 & 5; medical, surgical, Oby/Gyn & ICU wards respectively) and Leku Hospital 10, 10, and 13; medical, surgical and Oby/Gyn wards respectively.
Simple Random sampling (Lottery method) was employed again to obtain the individual participants from each ward by using Registration book as sampling frame obtained from case team leader as illustrated in (Figure 1).
Study Variables
Dependent Variable
• Pressure Ulcer
Independent Variables
• Socio demographic factors
▪ Age
▪ Gender
• Braden Risk Factors
▪ Sensory perception
▪ Moisture
▪ Activity
▪ Friction /Shear
▪ Mobility
▪ Nutrition
• Service-Related Factor
▪ Position change
▪ Length of stay in hospital
▪ Drug Profile
▪ Medical device related Factor
• Patient Related Factors
▪ BMI
▪ Edema
▪ Level of Consciousness
▪ Patient diagnosis
Data collection procedures
Participant information (such as age, Place of residence, Marital status, Educational status, Religion, Length of Hospital stay, and Evidence of prescribed turning position schedules, Edema, BMI, Presence of pressure ulcers) collected through interview, document review and physical examination techniques from head to toes. The tool is developed after reviewing different Literature [2,7,14,19,21,23,24] and the Braden Pressure Ulcer Risk Assessment Scale Adopted from Barbara J. Braden (33). The Structured Questionnaire contain three section part I, socio-demographic Question which contain 6 question, Part II , Patient and Service Related,17 question and Part III Braden risk assessment tool which has 6 item (sensory perception, skin moisture, activity, mobility, nutrition, and friction/shear[33]. summated rating scale made up of five subscales scored from 1-4 and six subscale 1-3, for total scores that range from 6-23. With cutoff <17 risk for PU and no risk of pressure ulcer at Braden score ≥17[14]. A lower Braden Scale Score indicates a lower level of functioning and, therefore, a higher level of risk for pressure ulcer development [34].
The data was collected by 6 trained Degree nurses and were supervised by 2 MSc nurses having previous experience in data collection. Continuous follow-up and supervision were performed by principal investigator throughout the data collection period.
Validity and Reliability
The Braden Scale has demonstrated a high degree of inter-rater reliability between 0.99 and 0.83. In terms of predictive validity, the Braden Scale has demonstrated sensitivities that range from 70% to 100% and specificities ranging from 64% to 90%. The tool has been shown to be equally reliable with Black and White patients [14,33,34].
Data analysis
The data was entered into EPI- data version 3.1, and then the data was edited, cleaned, and coded and analyzed by using Statistical Package for Social Science (SPSS) version 20 statistical software. Descriptive statistics: frequencies and percentages were done and presented in table, figure, and graph. Binary logistic regression was used to identify the statistical association between pressure ulcer and independent variables using, OR 95% CI and p-value of less than 0.25. Multiple logistic regression models were fitted to control the possible effect of confounders and finally the variables which had independent association with pressure ulcer was identified based on AOR, with 95%CI and p-value less than 0.05. The variables were entered to the multivariate model using the Backward LR regression.
Data quality control
Data quality was ensured during collection, coding, entry, and analysis. Training was given to the data collectors and supervisors to prevent any confusion and have a common understanding about the study. Pretest was conducted 10% of study participants at Dilla University Teaching Hospital; based on the pretest, questions were revised, edited, and those found to be unclear was removed by investigator. Supervision of data collectors and observation of how the data collectors were collected data was done by supervisors. The data collectors were instructed to write Medical record number on the Questionnaires during the data collection so that any identified errors were traced back using the Medical record number. The filled Questionnaires were checked for completeness by data collectors, supervisors, and Principal investigator daily. Consequently, any problem encountered was discussed among the team and solve immediately.
Ethical consideration
Ethical clearance and approval for the study was obtained from institutional review board (IRB) of Jimma University, institute of health. An official letter of cooperation was given to Hawassa Comprehensive specialized hospital, Adare General Hospital, Yirgalem General Hospital, Leku primary Hospital, Dilla University Teaching Hospital (neighboring to study zone) and an official letter of permission was provided to the head of Medical, surgical and Oby/Gyn wards for the utilization of patient cards and to conduct physical examination. The purpose and importance of the study was explained to each study participants and written or oral consent was obtained from patients and/or relatives. To ensure confidentiality of participant’s information, anonymous typing was applied whereby the name of the participant and any identified of participants were not be written on the questionnaire. Participant was interview and Examine alone to keep the privacy. Respondents who are not wasting to be involved in the study and those who want to stop interview at any time could do so. The instruments were translated from English into Amharic language, reviewed by a group of researchers for meaning, clarity and cultural appropriateness, and back translated into English for verification.
Dissemination Plan
The findings will be present to Jimma University, Institute of health, and Faculty of health science, School of Nursing, and midwifery. The copy of the result will be submitted to four public hospitals; also, I will try to disseminate through presentation on conferences and publication on scientific journals on local or international journals
Results
Socio-Demographic Data
A total of 356 admitted patients in Four Public Hospital were Participated in the study. Above half of study Participants 212(59.6%) were age between18-39 on the contrary 30(8.4%) were age between70-89.
Majority Participants, 267(75.0%), 230(64.6%), 218(61.2%) and 200(56.2%) were married, rural residents, females in Gender and Protestant in religion, respectively. In addition, 112 (31.5%) of the respondents were not educated (see table 1).
| Variables | Frequency (n) | Percent (%) |
|---|---|---|
| Numbers of Participants | ||
| Hawassa Comprehensive Specialized Hospital | 137 | 38.5 |
| Adare General Hospital | 69 | 19.4 |
| Yirgalem General Hospital | 117 | 32.9 |
| Leku Primary Hospital | 33 | 9.3 |
| Participants Age | ||
| 18-39 Age | 212 | 59.6 |
| 40-69 Age | 114 | 32.0 |
| 70-89 Age | 30 | 8.4 |
| Place of Residence | ||
| Urban | 126 | 35.4 |
| Rural | 230 | 64.6 |
| Sex of Patients | ||
| Male | 138 | 38.8 |
| Female | 218 | 61.2 |
| Religion of patients | ||
| Protestant | 200 | 56.2 |
| Orthodox | 92 | 25.8 |
| Muslim | 57 | 16.0 |
| Catholic | 7 | 2.0 |
| Marital Status | ||
| Single | 82 | 23.0 |
| Married | 267 | 75.0 |
| Divorced | 5 | 1.4 |
| Widowed | 2 | 0.6 |
| Educational Status | ||
| No education | 112 | 31.5 |
| Only read and write | 52 | 14.6 |
| 1-8 Grade | 106 | 29.8 |
| 9-12 Grade | 54 | 15.2 |
| 12+ Grade | 32 | 9.0 |
Table 1: Socio demographic Data of the Participants of Public Hospitals in Sidama Zone, SNNPR, Ethiopia, 2017 (N=356).
Patients and services related information
Majority patients 309 (86.8%) who admitted in four Public Hospitals in sidama Zone were stayed more than or equal to 6 days; meanwhile 47(13.2%) had stayed in Hospital less than 6 days.
Majority of study Participants 135(37.9%) were admitted in Surgical ward, 113 (31.7%) in medical ward and 12(3.4%) in ICU.
Majority of the patients 290(81.5%), 225(63.2%), and 160(44.9%) were conscious, had no turning position Schedule, and BMI between 18.5-24.99kg/m2, respectively.
Majority of Patients 310 (87.1%), 347(97.5%), and 131(36.8) were Used Medical device, patient with medication and Patient diagnosis with Sepsis, Respectively (table 2).
| Variables | Frequency (n) | Percent (%) |
|---|---|---|
| Length of Hospital Stay | ||
| <6 Days | 47 | 13.2 |
| >=6 Days | 309 | 86.8 |
| Patients Ward | ||
| Medical | 113 | 31.7 |
| Surgical | 135 | 37.9 |
| Gynecology | 96 | 27 |
| ICU | 12 | 3.4 |
| Level of consciousness | ||
| Unconscious | 66 | 18.5 |
| Conscious | 290 | 81.5 |
| Evidence of turning Position | ||
| No | 225 | 63.2 |
| Yes | 131 | 36.8 |
| Patient Body mass index | ||
| <18.5kg/m2 | 134 | 37.6 |
| 18.5-24.99kg/m2 | 160 | 44.9 |
| 25-29.99kg/m2 | 62 | 17.4 |
| Patient with Medical device | ||
| No | 46 | 12.9 |
| Yes | 310 | 87.1 |
| Patient with Medication | ||
| No | 9 | 2.5 |
| Yes | 347 | 97.5 |
| Patient Diagnosis | ||
| Diabetes Mellitus | 20 | 5.6 |
| Sepsis | 131 | 36.8 |
| Respiratory Disease | 22 | 6.2 |
| Anemia | 19 | 5.3 |
| Hypertension | 22 | 6.2 |
| Heart Disease | 8 | 2.2 |
| Stroke | 5 | 1.4 |
| Fracture | 15 | 4.2 |
Table 2: Patients and Services Related Information of the Participants in Public Hospitals in Sidama Zone, SNNPR, Ethiopia, 2017 (N=356).
Braden risk assessment scale Information
Out of the total Participants 118 (33.1%) had slightly limited in sensory perception, and 69 (19.4%) of participants had Occasionally Moist. From the total participants 52 (14.6 %) were completely immobile. 229 (64.3%) participants were probably inadequate in nutrition, and 168 (47.2%) of the patients had problem in Friction & Shear (table 3).
| Variable | Frequency | Percentage | |
|---|---|---|---|
| Sensory perception | Completely limited | 40 | 11.2% |
| Very limited | 38 | 10.7% | |
| Slightly limited | 118 | 33.1% | |
| No impairment | 160 | 44.9% | |
| Moisture | Constantly moist | 2 | 0.6% |
| Very moist | 5 | 1.4% | |
| Occasionally moist | 69 | 19.4% | |
| Rarely moist | 280 | 78.7% | |
| Activity | Bedfast | 119 | 33.4% |
| chair fast | 67 | 18.8% | |
| walks occasionally | 96 | 27% | |
| walks frequently | 74 | 20.8% | |
| Mobility | completely immobile | 52 | 14.6% |
| very limited | 90 | 25.3% | |
| slightly limited | 167 | 46.9% | |
| no limitation | 47 | 13.2% | |
| Nutrition | very poor | 76 | 21.3% |
| probably inadequate | 229 | 64.3% | |
| Adequate | 40 | 11.2% | |
| Excellent | 11 | 3.1% | |
| Friction and shear | Problem | 168 | 47.2% |
| potential problem | 125 | 35.1% | |
| no apparent problem | 63 | 17.7% | |
Table 3: Braden Scale Pressure Ulcer Risk Assessment of the Participants in Public Hospitals in Sidama Zone, SNNPR, Ethiopia, 2017 (N=356).
Prevalence of Pressure Ulcers
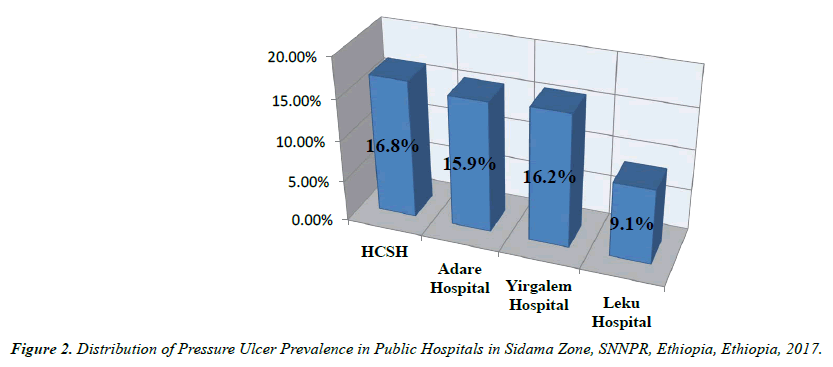
A total of 56 (15.7%) patients were developed pressure ulcer from 356 who were admitted in four public Hospitals in Sidama Zone; Out of the overall prevalence Hawassa comprehensive Specialized Hospital, Yirgalem Hospital, Adare Hospital, and Leku Hospital were accounts 16.8% (23), 16.2% (19), 15.9%(11), and 9.1% (3) respectively (see figure 2).
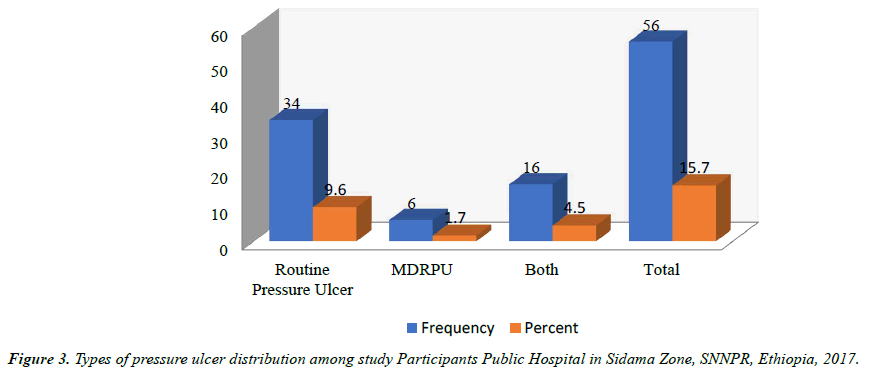
Out of those who developed PU 34(9.6%), 16(4.5%), and 6 (1.7%), and were due to Routine, Both Types, and MDRPU respectively (see figure 3).
Prevalence Medical device related pressure ulcers
The Overall Prevalence Pressure ulcers was 56 (15.7%) from which MDRPU which account 6 (1.7%). From this; Hand and Lips 3 (50%), leg 2(33.3%), and Nose, Ear and Neck 1(16.7%). Based on EPUAP stage 3(50%) were stage I and 3(50%) stage II.
Pressure Ulcer and Socio-Demographic Data
Patients age between 40-69 and 70-89 pressure ulcer were more prevalent 27(23.7%) and 5(16.7%) respectively. Majority of Patients who developed Pressure ulcers were not educated and between grades 1-8. The prevalence of pressure ulcer was higher in male respondents 27(19.6) than in female respondents 29(13.3%). The reason might be male were low fat composition than female (table 4).
| Variables | Patients develop pressure Ulcer | ||||
|---|---|---|---|---|---|
| NO | Yes | ||||
| N° | Percent (%) | N° | Percent (%) | ||
| Patient Age | 18-39 40-69 70-89 |
188 | 88.7% | 24 | 11.3% |
| 87 | 76.3% | 27 | 23.7% | ||
| 25 | 83.3% | 5 | 16.7% | ||
| Sex | Male Female |
111 | 80.4% | 27 | 19.6% |
| 189 | 86.7% | 29 | 13.3% | ||
| Residence | Urban Rural |
105 | 83.3% | 21 | 16.7% |
| 195 | 84.8% | 35 | 15.2% | ||
| Education | No Education Only Read &write 1-8 grade 9-12 grade 12+ |
92 | 82.1% | 20 | 17.9% |
| 49 | 94.2% | 3 | 5.8% | ||
| 86 | 81.1% | 20 | 18.9% | ||
| 43 | 79.6% | 11 | 20.4% | ||
| 30 | 93.8% | 2 | 6.2% | ||
Table 4: Prevalence of Pressure Ulcer and Socio-Demographic Data of the Participants in Public Hospitals in Sidama Zone, SNNPR, Ethiopia, 2017 (N=356).
Pressure Ulcer with Patients and services related Variables
Majority of admitted patient in Public Hospital 160(44.9%) of them were BMI in between 18.5-24.99 kg/m2 and pressure ulcer more prevalent 33(24.6%) of BMI <18.5kg/m2. 309(86.8%) admitted patients were greater than or equal to six-day length of Hospital stay; from which 55(17.8%) of the Participant develop pressure ulcers. 276 (77.5%) of patient have no edema; 21(26.2%) Patient develop pressure ulcer with Edema.
Majority of the patient admitted in Public hospitals 250 (86.2%) were conscious; the prevalence of pressure ulcer 16(24.2%) increased in unconscious patients. Majority of hospitalized patients 225(63.2%) had no evidenced position change schedule; and from those no position changes 44(19.6%) of them develop pressure ulcers.
Majority of patients 135(37.9%) were admitted in surgical ward; the least were 12(3.4%) in ICU and which was the most prevalent Unit in the Wards (table 5).
| Variables | Patients develop pressure Ulcer | ||||
|---|---|---|---|---|---|
| NO | Yes | ||||
| N° | Percent (%) | N° | Percent (%) | ||
| BMI | <18.5 kg/m2 |
101 | 75.4% | 33 | 24.6% |
| 18.5-24.99 kg/m2 |
140 | 87.5% | 20 | 12.5% | |
| 25-29.99 Kg/m2 | 59 | 95.2% | 3 | 4.8% | |
| Edema | No |
241 | 87.3% | 35 | 12.7% |
| Yes | 59 | 73.8% | 21 | 26.2% | |
| Patient levels of consciousness | Unconscious |
50 | 75.8% | 16 | 24.2% |
| Conscious | 250 | 86.2% | 40 | 13.8% | |
| Patient diagnosis | Diabetes Mellitus | 287 | 85.4% | 49 | 14.6% |
| 13 | 65% | 7 | 35% | ||
| Sepsis | 186 | 82.7% | 39 | 17.3% | |
| 114 | 87% | 17 | 13% | ||
| Respiratory Disease | 282 | 84.4% | 52 | 15.6% | |
| 18 | 81.8 | 4 | 18.2 | ||
| Anemia | 283 | 84% | 54 | 16% | |
| 17 | 89.5% | 2 | 10.5% | ||
| Hypertension | 285 | 85.3% | 49 | 14.7% | |
| 15 | 68.2% | 7 | 31.8% | ||
| Heart Disease | 293 | 84.2% | 55 | 15.8% | |
| 7 | 87.5% | 1 | 12.5% | ||
| Stroke | 297 | 84.6% | 54 | 15.4% | |
| 3 | 60% | 2 | 40% | ||
| Fracture | 290 | 85% | 51 | 15% | |
| 10 | 66.7% | 5 | 33.3 | ||
| Turning position | No |
181 | 80.4% | 44 | 19.6% |
| Yes | 119 | 90.8% | 12 | 9.2% | |
| Length of Hospital stay | <6 days | 46 | 97.9% | 1 | 2.1% |
| >= 6 days | 254 | 82.2% | 55 | 17.8% | |
| Wards | Medical |
87 | 77% | 26 | 23% |
| Surgical |
118 | 87.4% | 17 | 12.6% | |
| Gyn |
91 | 94.8% | 5 | 5.2% | |
| ICU | 4 | 33.3% | 8 | 66.7% | |
| Medical device | No |
43 | 93.5% | 3 | 6.5% |
| Yes | 257 | 82.9% | 53 | 17.1% | |
| Drug Profile | Antimicrobial |
||||
| No |
106 | 77.9% | 30 | 22.1% | |
| Yes | 185 | 87.7% | 26 | 12.3 | |
| Antihypertensive | |||||
| No |
274 | 85.1% | 48 | 14.9% | |
| Yes | 17 | 68% | 8 | 32% | |
| Analgesics | |||||
| No |
244 | 82.7% | 51 | 17.3% | |
| Yes | 47 | 90.4% | 5 | 9.6% | |
| Antidepressant | |||||
| No |
290 | 84.3% | 54 | 15.7% | |
| Yes | 1 | 33.3% | 2 | 66.7% | |
| Ant diabetics | |||||
| No |
287 | 85.7% | 48 | 14.3% | |
| Yes | 4 | 33.3 | 8 | 66.7% | |
Table 5: Distribution Pressure Ulcer with Patients and services related Variables in Public Hospitals in Sidama Zone, SNNPR, Ethiopia, 2017 (N=356).
Anatomical Location and Stages of Pressure Ulcer
Based on EPUAP grading scale; 21(5.9%), 26 (7.3%), 4 (1.1%), and 5(1.4%) patients developed stage I, stage II, stage III, and stage (stage IV) pressure ulcer, respectively. In terms of anatomical location 20(5.6%), 16(4.5%) were developed pressure ulcer on Sacral area and Shoulder, respectively. 7(2.0%), 4(1.1%), were at Hand& lips and heel area, respectively (table 6).
| Variable | Frequency | Percentage | |
|---|---|---|---|
| Stages of Pressure Ulcer | Stage I | 21 | 5.9% |
| Stage II | 26 | 7.3% | |
| Stage III | 4 | 1.1% | |
| Stage IV | 5 | 1.4% | |
| Anatomical Location Pressure Ulcer | Sacral | 20 | 5.6% |
| Shoulder | 16 | 4.5% | |
| Hand & Lips | 7 | 2% | |
| Greater trochanter, Heel, Leg, Nose, ear, Neck, Elbow, Other area (Occipital) | 13 | 3.6% | |
Table 6: Frequency and percentage of Anatomical Location and stage of Pressure Ulcer in Public Hospitals in Sidama Zone, SNNPR, Ethiopia, 2017 (N=356).
Factors Associated with Pressure Ulcer
Independent variables analyzed in logistic regression with Outcome variable of pressure ulcer to identify their association. Those variables which were significant at ≤ 0.25 entered multiple logistic regressions. A multiple logistic regression identified that Position change; BMI, Activity, mobility, moisture, Antimicrobial, and ant diabetic were significantly associated with the development of pressure ulcer.
Study Participants who had No Position change schedule were 4.34 times (95% CI: AOR, 4.346 (1.646 – 11.473; P= 0.003) more likely to develop Pressure ulcer than Participants who had position change. Those participants who had Body mass index of Less than 18kg/m2 were 6.9 times (95% CI: AOR, 6.912(1.307,36.554) more likely to develop pressure Ulcers than Patients who had BMI in between 25-29.99kg/m2.
Participants who had occasionally Moist were 4.7 times (95% CI: AOR, 4.734(1.999, 11.234) more risk to develop Pressure ulcer than those rarely Moist skin. Patients who were bed fast in activity 13.4 times (95% CI: AOR, 13.365(1.622, 110.138) more risk to develop Pressure Ulcer than those who walks frequently.
Those participants who had very limited in Mobility were 10.7 times (95% CI: AOR, 10.661 (1.256, 90.494) more likely risk to develop pressure Ulcer than Participant who had no limitation in mobility. Patients who had Problem for friction and shear were 5 times (95% CI: AOR, 5.002(1.024, 24.445) more likely to develop pressure ulcer than Patient who had no apparent problem (table 7).
| Variables | Pressure develop Ulcer | Crude OR(95% CI) | P-Value | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Patients age | 18-39 Age | 188 | 24 | 1 | |
| 40-69 Age | 87 | 27 | 2.431(1.327,4.455)* | 0.004 | |
| 70-89 age | 25 | 5 | 1.567(0.548,4.477) | 0.402 | |
| Patient Gender | Male | 111 | 27 | 1.585(0.893,2.815)* | 0.116 |
| Female | 189 | 29 | 1 | ||
| Educational Status | no education | 92 | 20 | 3.261 (0.720,14.773)* | 0.125 |
| only read and write | 49 | 3 | 0.918 (0.145, 5.817) | 0.928 | |
| 1-8 grade | 86 | 20 | 3.488 (0.769, 15.819)* | 0.105 | |
| 9-12 grade | 43 | 11 | 3.837 (0.793, 18.576)* | 0.095 | |
| 12+ grade | 30 | 2 | 1 | ||
| Patient Level of consciousness | Unconscious | 50 | 16 | 2.000(1.039,3.848)* | 0.038 |
| Conscious | 250 | 40 | 1 | ||
| Length of Hospital stay | <6 days | 46 | 1 | 1 | - |
| >=6 days | 254 | 55 | 9.961(1.345,73.783)* | 0.024 | |
| Position Change | No | 181 | 44 | 2.411 (1.223,4.753)* | 0.011 |
| Yes | 119 | 12 | 1 | ||
| Patient Body mass index | <18.5kg/m2 | 101 | 33 | 6.426(1.888,21.869)* | 0.003 |
| 18.5-24.99kg/m2 | 140 | 20 | 2.810(0.804,9.816)* | 0.106 | |
| 25-29.99kg/m2 | 59 | 3 | 1 | ||
| diabetes mellitus | No | 287 | 49 | 1 | |
| Yes | 13 | 7 | 3.154(1.199,8.299)* | 0.020 | |
| Sepsis | No | 186 | 39 | 1 | |
| Yes | 114 | 17 | 0.711(0.384,1.316) | 0.278 | |
| Disease of Respiratory | No | 282 | 52 | 1 | |
| Yes | 18 | 4 | 1.205(0.392,3.705) | 0.745 | |
| Anemia | No | 283 | 54 | 1 | - |
| Yes | 17 | 2 | 0.617(0.138,2.746) | 0.526 | |
| Hypertension | No | 285 | 49 | 1 | - |
| Yes | 15 | 7 | 2.714 (1.053,6.997)* | 0.039 | |
| Stroke | No | 297 | 54 | 1 | - |
| Yes | 3 | 2 | 3.667(0..599,22.462)* | 0.160 | |
| Fracture | No | 290 | 51 | 1 | - |
| Yes | 10 | 5 | 2.843(0.933,8.662)* | 0.066 | |
| Antimicrobial | No | 106 | 30 | 2.014(1.131,3.586)* | 0.017 |
| Yes | 185 | 26 | 1 | ||
| Antihypertensive | No | 274 | 48 | 1 | |
| Yes | 17 | 8 | 2.686(1.098,6.571)* | 0.030 | |
| Analgesics | No | 244 | 51 | 1 | |
| Yes | |||||