- Biomedical Research (2013) Volume 24, Issue 3
Prevalence of Heamoglobin Variants, ABO and Rhesus Blood Groups in Northern Uttar Pradesh, India.
Pratima Verma, Shraddha Singh, Akhilesh Krishna, Wahid Ali*, Sunita TiwariDepartment of Physiology and P.G. Department of Pathology*, King George's Medical University, U.P., Lucknow, India
- Corresponding Author:
- Shraddha Singh
Department of Physiology
King George's Medical University
Lucknow 226003, India
E-mail: drshraddha.22@rediffmail.co, drshraddhasingh@yahoo.com
Accepted date: April 13 2013
Citation: Verma P, Singh S, Krishna A, Ali W, Tiwari S. Prevalence of Heamoglobin Variants, ABO and Rhesus Blood Groups in Northern Uttar Pradesh, India. Biomed Res- India 2013; 24 (3):377-384.
Abstract
Hemoglobin variants are mutant forms of hemoglobin in a population , caused by variations in genetics. It’s occurring when there are genetic changes in specific genes, or globins that cause changes or alterations in the amino acid. Hemoglobin variants, ABO and Rhesus blood groups are known to vary from one population to another. Thus, there is need to elucidate the frequency of these indices in Northern U.P., India. The result would serve as a platform for instituting genetic counseling services with a view to reduce haemoglobinopathies. Total 933 subjects aged 18 – 55 years were screened, 636 (68.17%) males and 297 (31.83%) females. Result of present study showed 12.01% prevalence of haemoglobinopathies. Out of total haemoglobinopathies screened subject, β-thalassemia in heterozygous state was found more frequent (5.04%) than β-thalassemia in homozygous state (0.43%). Other haemoglobinopathies followed by HbAE 3.32%, HbAS 0.86%, HbE-β 1.82% and HbS-β 0.54%. The frequencies with respect to ABO systems had been shown as O > B > A > AB. The distribution of Blood groups with 97.43% Rhesus positive (Rh+) out of which, O+(36.55%), B+ (35.78%), A+(18.97%), AB+ (6.11%) found respectively. In our study the Blood group O+ (36.55%), was most frequent but the higher prevalence haemoglobinopathies was found in Blood group A+ (33.93).
Keywords
ABO, blood groups, Haemoglobinopathy, Agrose gel electrophoresis
Abbreviations
Hb- Haemoglobin, α-Alfa, β- Beta, βT Minor - β thalassemia heterozygous, βT Major -β thalassemia homozygous, β TT - β thalassemia trait, HbAA - homozygous hemoglobin, HbAS - heterozygous hemoglobin with sickle cell disease gene, HbAE - heterozygous hemoglobin with E variant gene, HbE-β- β thalassemia trait with E variant gene, HbS-β- β thalassemia trait with sickle cell disease gene, %- Percent, μL- Micro liter, mL –Mili liter , V - Volts, mA -Mili Ampere, min- Minutes, g/dl- Gram per deciliter, CBC- Complete Blood Counts, EDTA - Ethylene diamine tetracetic acid.
Introduction
The inherited Hb disorders are the most common single gene defect in man. The prevalence of haemoglobinopathies is on the rise worldwide. The abnormalities can either be quantitative (the thalassemia syndromes) or qualitative (the haemoglobin variants) or a combination of both. Of these, the thalassemia syndromes particularly the beta thalassemias and some alpha thalassemias are the major cause of morbidity [1]. The World Health Organization (WHO) has suggested that about 5% of the world population is carrier for different inherited disorders of haemoglobin [2]. Approximately 80-90 million people with 60,000 new cases of β-thalassemia were estimated per year worldwide. The South-east Asia region (such as India, Thailand and Indonesia) is accounts for 50% (around 40 million people) of world carriers. Although in the developed world, Europe and the Americas jointly account for just 10% to 13% of the world’s carriers [3]. The prevalence of β-thalassemia trait is about 3.3% in India. According WHO report, about 370,000 severely affected homozygotes or compound heterozygotes of thalassemia are born every year. The UNICEF in 1996 estimated that there were 29.7 million carriers of beta thalassemia trait in India and about 10,000 infants with homozygous beta thalassemia born every year [4]. In various parts of India, the prevalence of β-thalassemia is different: 6.5% in Punjab, 8.4% in Tamilnadu, 4.3% in south India, and 3.5% in Bengal. β- Thalassemia has a high prevalence in some communities, such as Sindhi, Luvana, Tribes, and Rajputs. The incidence of β-thalassemia in Gujarat is 10% to 15% [5]. Generally incidence of thalassemia trait and sickle cell haemoglobinopathies in India varies between 3-17% and 1-44%, respectively [6-8]. In India, nearly 30 million people are carriers of beta thalassemia and 7000 babies with beta-thalassemia major are born every year [9-10,]. The carrier rate varies between 0 to 17% in different ethnic groups [11].
Among the haemoglobin variants, haemoglobin E (β-26 glutamine→lysine) is the hallmark of South-East Asia. It is the commonest haemoglobin variant in India with prevalence of 7-50% in Northeastern region and 1-2% in West Bengal [12]. Because a majority of people with BTT are asymptomatic, they may not be aware of their carrier state. β-thalassemia trait is associated with mild or no anemia but with reduced mean corpuscular volume , mean corpuscular haemoglobin values and an elevated haemoglobin A2 level. The prevention of this homozygous condition can be achieved through the detection and education of heterozygous carriers. One way of achieving this goal is to screen the population at risk [13].
Sickle cell anemia and thalassemia major can cause lifethreatening situation and chronic ill health. They pose economical and psychological burden on the affected individual or family and the society as a whole. Hence, the population needs to be screened for haemoglobin disorders so that appropriate measures for treatment and prevention can be taken [14]. The membrane of the human red blood cell is complex and contains a variety of blood group antigens [15]. The ABO blood group system is the most clinically important blood group system because antibodies against A or B or both antigens of RBC’s are naturally present in the serum of persons whose red cells express blood group B, A, or O. In addition, human red blood cells that contain antigen D are known as Rhesus positive, while those without antigen D in their RBC’s are Rhesus negative. The ABO and Rh incompatible transfusions are potentially fatal to health [16,17].
The data regarding prevalence and distribution of the haemoglobin variants and blood groups aiding in prevention and management of various haemoglobinopathies plays a vital role in the hospital blood bank as well as in the formulation of transfusion policies [15].The frequencies of these inherited characters have been extensively reported in various populations and ethnic groups around the world [16-18]. In India, few published data have been encountered [19-21]. The data of the distribution pattern and frequency of haemoglobin variant, ABO and Rh blood group is still to explored in Northern region of Uttar Pradesh. Therefore, this study is aimed to provide useful information on the distribution pattern of haemoglobinopathies, ABO and Rh blood groups in Northern U.P. India.
Material and Methods
Subject Selection
The present study was carried out in the Department of Physiology and P.G. Department of Pathology in Kings Georg’s Medical University, U.P., Lucknow during the period of December 2009 to May 2012.Total 933 study participants were selected by random sampling with obtaining the consent. The age between 18 years to 55 years. These participants were pre-marital candidates, pregnant mother with known suspicious or unknown family history, clinically suspicious or haemoglobin fall patients referred by the physician and some self participants. But all participants were represented from northern region of Uttar Pradesh. The study was approved by Institutional ethics committee Kings Georg’s Medical University, U.P., Lucknow, India.
Sample collection and Preparation
6 ml venous blood was collected in EDTA vials and put few drops of fresh whole blood on slides for blood group investigation .The anticoagulated blood was used for performing CBC, reticulocyte count, haemoglobin electrophoresis. Haemolysate was prepared from whole blood by using saline and carbon tetra chloride with a concentration of 1.6 g/dl to 2.2 g/dl to the haemoglobin electrophoresis [22].
Blood Group identification
ABO and Rhesus blood grouping were carried out using the tile method. Few drops of whole blood of each subject was mixed with respective antisera, anti A, anti B, anti D reagents (Tulip Diagnostics (P) Ltd., Goa, India) in separate places on a clean slide and blood groups were determined on the basis of agglutination.
CBC- Hematological indices were measured using Sysmex MX– 4 fully automated blood cell counter, which was calibrated with commercially available controls. The sickling test was performed using freshly prepared sodium metabisulphite solution as a reducing agent [23].
Electrophoresis
Agarose gel electrophoresis was performed using Tris- EDTA –borate buffer at alkaline pH (8.8). The electrophoresis pattern is visualized by staining the film with a ponceau stain. This pattern was then quantified using a densitometer (Beckman Coulter) at 600 nm wavelength [22,24].
Results/Observations
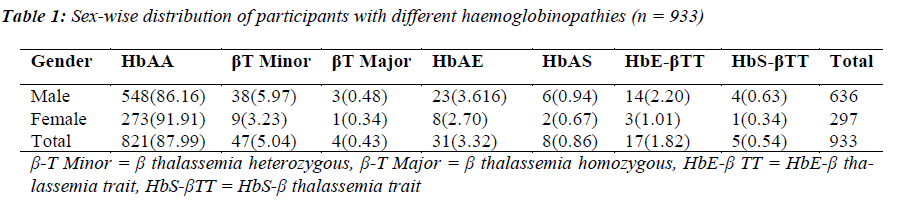
A total 933 participants were screened for abnormal hemoglobin variants, ABO, and Rhesus blood groups. Out of total 933 subjects, male were 636 (68.17%) and female 297 (31.83%). Table1 showed different patterns of haemoglobin variants according to Gender. Out of 933 subjects, we found 821 subjects (87.99%) were normal (HbAA) and 112 subjects (12.01%) with abnormal hemoglobin variants or haemoglobinopaties. In present study, total observed haemoglobinopathy 112 (12.01%), in which the most frequent haemoglobinopathy was β- thalassemia minor (βT-minor) 47 (5.04%) while less frequent β-thalassemia major (βT-major) 4 (0.43%). However, frequency of other hemoglobin variants such as HbAE 31(3.32%), HbE-βTT 17(1.82%), HbAS 8 (0.86%), HbS-βTT 5(0.54%) respectively.
In male the frequency of βT Minor was high 38 (5.97%) followed by HbAE 23 (3.62%), HbE-βTT 14(2.20%), HbAS 6(0.94%), HbS-βTT 4(0.63%), βT Major 3 (0.48%). In female the frequency of haemoglobinopathies βT Minor (β-thalassemia heterozygous) was 9 (3.23%), followed HbAE 8 (2.70%), HbE-βTT 3(1.01%), HbAS 2(0.67%), HbS-βTT and βT Major 1 (0.34%) .
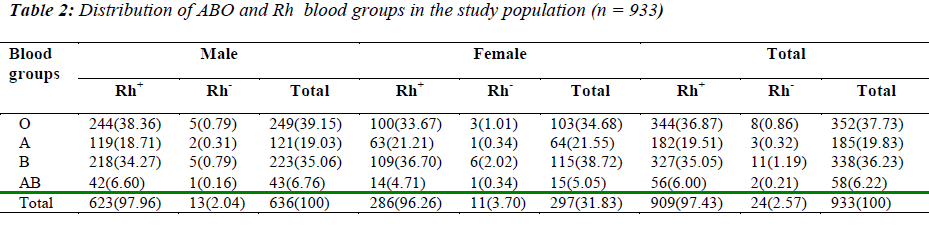
Table 2 revealed the distribution of the ABO and Rhesus (D) blood groups among study subjects. Blood group O was found to be the most frequent 352 (37.73%) while blood group AB was least frequent 58 (6.22%). In Rh blood typing, 97.43% was Rh positive and 2.57% was Rh negative. Amongst Rh positive male blood group ‘O’ was found to be most prevalent group 38.36% followed by group ‘B’ (34.27%), ‘A’ (18.71%) and ‘AB’ (6.6%). Among Rh positive female, blood group ‘B’ was most common (36.7%) followed by group ‘O’ (33.67%), ‘A’ (21.21%) and ‘AB’ (4.71%). On further analysis female showed a relatively higher incidence of Rh negativity (3.7%) as compared to male (2.04%). The frequencies pattern with respect to ABO can be shown as O > B > A > AB.
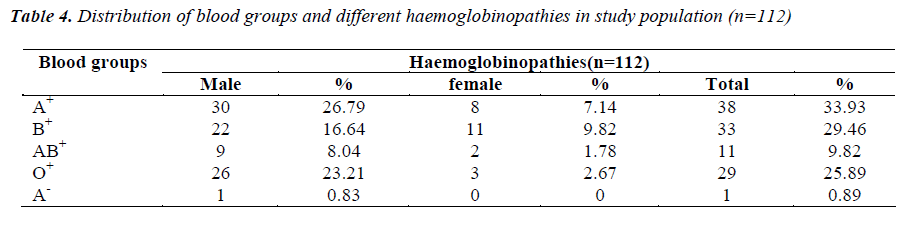
Table 3 shows the prevalence of blood group with haemoglobinopathies. The present study shown that haemoglobinopathy was most frequent in Rh positive ‘A’ 38(33.93%) followed by Rh positive ‘B’ 33(29.46%) , Rh positive ‘O’ 29 (25.89%) , Rh positive ‘AB’ 11(9.82) and Rh negative ‘A’1(0.89%).
Discussion
The thalassaemias and related haemoglobinopathies are responsible for the largest number of genetic disorders and hence are of great public health importance in India. It indicates that haemoglobinopathies and their related clinical complications are not uncommon at birth. The inherited disorders of haemoglobin synthesis are one of the important public health problems in the region. The present scenario of haemoglobinopathies reflects the genetic heterogeneity of the population of the region. Historical accounts reveal that several ethnic elements with varied genetic heritages have been absorbed into the mainstream, resulting in population diversity with the passage of time [25,26] The findings of prevalence of different haemoglobinopathies in the region are in agreement with the population admixture in Northern Uttar Pradesh, India.
The present study revealed that large numbers of people were encountered with haemoglobinopathies (12.01%) in northern region of Uttar Pradesh. In our study, β- thalassemia heterozygous individuals (5.04%) was the most frequently encountered quantitative haemoglobinopathies, followed by HbAE (3.32%), β-thalassemia homozygous state (0.43%), HbE β-thalassemia trait (1.82%), HbAS (0.86%) and HbS β-thalassemia trait (0.54%). This compares with previous studies from Kolkata (26%) and Gujarat (16.35%) where β-thalassemia heterozygous was the commonest disorder [11,25]. In a study by Balgir, sickle cell trait was reported common disorders from Orissa where sickle cell trait and β- thalassemia trait were the most frequently encountered haemoglobinopathies. Different variants of haemoglobinopathy manifest variable clinical and hematological profile in India [8]. The highest frequency of β-thalassemia trait is reported in Gujarat (10-15%), followed by Sindh (10%), Punjab (6.5%), Tamil Nadu (8.4%), and Maharashtra [6,8,21]. This study is similar to a Italian study in regards of percentage (1.81 % of total population), but the percent wise distribution of types of haemoglobinopathies is inconsistent with our study. [28,29,30].
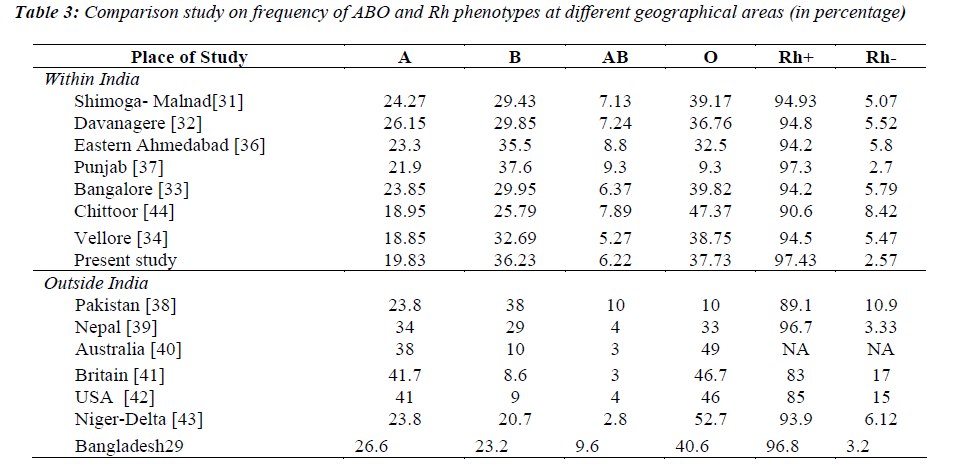
The frequency of ABO Blood Groups is an important tool to determine the direction of recruitment of voluntary donors as required for each zone across the country. In our study the ABO blood groups and Rh positivity in male and female showed that the blood group O positive was most prevalent in male followed by group B, A and AB. blood group B positive female followed by group O,A and AB. The distribution of ABO blood group varies regionally, ethically and from one population to another. The comparison of frequency and distribution of ABO and Rh group in Northern Uttar Pradesh, India (present study) with the similar studies carried out within and outside India is described in table-3.
While looking at ABO grouping, it can be read from table- 3 that the distribution of ABO and Rh grouping was comparable to the studies done at Shimoga- Malnad, Davanagere, Bangalore, Vellore, Britain [31-35]. All these studies have described ‘O’ as the most frequent and ‘AB’ as the least common blood group. The second most common blood group was observed as “B” in present study which is found to be consistent with the studies reported earlier at Eastern Ahmedabad , Punjab and Pakistan [36-38]. Studies at Southern India have described similar findings with ‘O’ being the most common blood group followed by ‘B’, ‘A’ and ‘AB’ [31-35]. In Nepal , which is connected to western India, as well as Australia, Britain and USA, ‘O’ and ‘A’ are the common blood groups that are followed by B and ‘AB’[40-42]. In Nigeria ‘O’ is the predominantly encountered blood group accounting for more than 50 % of donors and AB has least common occurrence [43]. In Rhesus System, our study shows prevalence of Rh positive was 97.43%, while only was 2.57% was Rh negative table-2.These are similar to other studies carried out in Punjab, India [18]. While looking at Rh grouping, 89-95 % donors all over the world are detected as Rh positive except at Britain and U.S.A. where the frequency of Rh positivity is 83%, 85 % respectively and Rh negativity 17 %,15% respectively . Almost similar incidences of Rh negative donors from other countries are as follows e.g. Nepal (3.3%) and Bangladesh (3.2%) which are neighboring country of the India.Knowledge of the prevalence and distribution of haemoglobinopathies, ABO and Rh blood groups among any population is useful in health care planning and appropriate allocation of resources [11,15]. haemoglobinopathy screening and identification can become the cornerstone to reduce this burden especially in developing countries. Adequate measures and screening procedures should be performed concurrently. In short, generation of a simple database of blood groups, not only provides data about the availability of human blood in case of regional calamities, but also serves to enables insight into possibilities of future burden of diseases.
Acknowledgements
The authors would like to thank the participants for participating in this study; the participating physicians and residents of the Department of Medicine and Physiology, King George's Medical University Uttar Pradesh Lucknow, India for their generous support. This study was supported by the Council of science and technology Lucknow Uttar Pradesh (Grant No. CST/D 3322).
References
- Sachdev R, Dam AR, Tyagi G. Detection of Hb variants and haemoglobinopathies in Indian population using HPLC: report of 2600 cases
- Angastinosis M, Modell B. Global epidemiology of haemoglobin disorders. Proc Natl Acad Sci USA 1998; 850: 251-269.
- Angastinotis M. Epidemiology. In: Galanello R, Eleftheriou A, Traeger-Synodinos J, et al, eds. Prevention of Thalassemias and Other Haemoglobin Disorders. Vol I. Nicosia, Cyprus: Thalassemia International Federation Publication; 2005: 10-13.
- UNICEF. The state of the world’s children. Oxford : Oxford university Press, 1996; 250.
- Ambek SS, Phadke MA, Mokashi GD, et al. Pattern of haemoglobinopathies in western Maharastra. Indian Pediatr. 2001; 38: 530-535.
- Balgir RS. The burden of haemoglobinopathies in India and the challenges ahead. Curr Sci 2000; 79:1536- 1547.
- Balgir RS. The genetic burden of haemoglobinopathies with special reference to community health in India and the challenges ahead. Indian J Hematol Blood Transfus 2002; 20: 2-7.
- Balgir RS. Spectrum of haemoglobinopathies in the state of Orissa, India: A ten years cohort study. J Assoc Physicians India 2005; 53: 1021-1026.
- Choudhury V, Kotwal J, Saxena R. Thalassemia screening and control programme. Pediatrics Today 1998 ; 1: 283-289.
- Verma IC, Saxena R, Thomas E, Jain PK. Regional distribution of beta-thalassemia mutations in India. Hum Genet 1997; 100(1): 109-113.
- B, Chakraborti S, Sengupta B. Prenatal Diagnosis of Thalassaemias. Int J Hum Genet 2002; 2(3): 173-178.
- Piplani S. Haemoglobin E disorders in the north east India. J Assoc Physicians India 2000; 48(11): 1082- 1084.
- Shalev O, Yehezkel E, Rachmilewitz EA. Inadequate utilization of routine electronic RBC counts to identify beta thalassemia carriers. Am J Public Health. 1993; 78:1476-1477.
- B. Sudhakar,R. M Shah, Y. C. Yada. HAEMOGLOBINOPATHIES IN VADODARA: A HOSPITALBASED STUDY. Int J Drug Discovery and Medical Research Accepted 25 May 2012
- Erhabor O, Adias TC, Jeremiah ZA, Hart ML. Abnormal haemoglobin variants, ABO, and Rhesus blood group distribution among students in the Niger Delta of Nigeria. Pathol Lab Med Int 2010; 2: 41-46.
- Jeremiah ZA. Abnormal haemoglobin variants, ABO and Rh blood groups among student of African descent in Port Harcourt, Nigeria. Afr Health Sci 2006; 6:177- 81.
- Akhigbe RE, Ige SF, Afolabi AO, Azeez OM, Adegunlola GJ, Bamidele JO. Prevalence of haemoglobin variants, ABO and rhesus blood groups in ladoke akintola University of Technology, Ogbomoso, Nigeria. Trends Med Res 2009; 4: 24-49.
- Egesie UG, Egesie OJ, Usar I, Johnbull TO. Distribution of ABO, Rhesus blood groups and haemoglobin electrophoresis among the undergraduate students of Niger Delta University Nigeria. Niger J Physiol Sci 2008; 23: 5-8.
- Patel J, Patel A, Patel J, Kaur A, Patel V. Prevalence Of Haemoglobinopathies in Gujarat, India: A Cross- Sectional Study. Int J Hematol 2009; 5(1).
- Shivashankara AR, Jailkhani R, Kini A. Haemoglobinopathies in Dharwad, North Karnataka: A hospitalbased study. J Clin Diagnostic Res 2008; 593-599.
- Balgir RS. Genetic epidemiology of the three predominant abnormal haemoglobins in India. J Assoc Physicians India 1996; 44: 25-28.
- Dacie JV, Lewis SM. Practical Hematology. 10th Ed. Edinburgh:Churchill Livingstone 2006.
- Daland GA, Castle WB. Simple and rapid method for demonstrating sickling of red blood cells use of reducing agents. J Lab Clin Med 1948; 53: 1082.
- Weatherall DJ. The Thalassemias. In: Methods in Hematology. Vol 8. New York:Churchill Livingstone 2001.
- Russel RV, Lal H. Tribes and Castes of the Central Provinces of India. Four volumes, Macmillan Company, London, 1916: 215-218.
- Balgir RS, Dash BP, Murmu B. Blood groups, haemoglobinopathy and G-6-PD deficiency investigations among fifteen major scheduled tribes of Orissa, India. Anthropologist, 2004; 6: 69-74.
- Swarup-Mitra S. Medical Genetics in India. In: Verma IC, editor. Vol. 2. Pondicherry: Auroma Enterprises; 1978; 199-213.
- Lisot CL, Silla LM. Screening for hemoglobinopathies in blood donors from Caxias do Sul,Rio Grande do Sul, Brazil: 1595-601.
- Angastiniotis, M. and Modell, B. Global epidemiology of hemoglobin disorders. Ann. N.Y. Acad Sci 1998; 850: 251-269.
- Mukherjee MB, Lu CY, Ducrocq R Gangakhedkar RR, Colah R, Kadam MD,et al. Effect of alpha thalassaemia on sickle cell anaemia linked to the Arab-India haplotype in India. Am JHematol 1997; 55(2): 104-109.
- Girish C J, Chandrashekhar T N, Ramesh Babu K, Kantikar SM. ABO and Rhesus blood group distribution among Malnad region blood Donors Research and Reviews in Biomedicine and Biotechnology [RRBB]. 2011; 2 (3): 25-30.
- Mallikarjuna S. Prevalence of ABO and Rhesus blood group among blood donors. Indian Journal of Public Health, Research and Development. 2011.
- Periyavan A, Sangeetha S K, Marimuthu P, Manjunath B K,Seema. Distribution of ABO and Rhesus-D groups in and around Bangalore. Asian J Transfus Sci. 2010; 4 (1): 41.
- Das P K, Nair S C, Harris V K, Rose D, Mammen J J, Bose Y N, Sudarsanam A. Distribution of ABO and Rh-D blood groups among blood donors in a tertiary care centre in South India. Trop Doct. 2001; 31 (1): 47- 48.
- Frances TF: Blood groups (ABO groups). In: Common Laboratory and Diagnostic Tests. Philadelphia: Lippincott. 2002, 3rd Edition: 19-95.
- Wadhwa MK, Patel SM, Kothari DC, Pandey M, Patel DD. Distribution of ABO and Rhesus-D groups in Gujarat, India: a hospital based study. Indan J Ped Oncol. 1998; 19 (4): 137-141.
- Sidhu S. Distribution of the ABO Blood Groups and Rh (D) Factor Among the Scheduled Caste Population of Punjab. Anthropologist. 2003; 5: 203-204.
- Hammed A, Hussain W, Ahmed J, Rabbi F, Qureshi J A.Prevalence of Phenotypes and Genes of ABO and Rhesus (Rh) Blood Groups in Faisalabad, Pakistan. Pak J Biol Sci. 2002; 5: 722-724.
- Pramanik T, Pramanik S. Distribution of ABO and Rh blood groups in Nepalese medical students: a report. East Mediterr Health J 2000; 6 (1): 156-158.
- Australian Red Cross society. All about blood. URL: www.donateblood.com.au/all-aboutblood/blood-types.
- Frances TF: Blood groups (ABO groups). In: Common Laboratory and Diagnostic Tests. Philadelphia: Lippincott, 2002; 3rd Edition: 19-25.
- Mollison PL, Engelfriet CP, Conteras M. The Rh blood Group system. In Blood Transfusion in Clinical Medicine, 9th Edition. Oxford: Black well Scientific Publication. 1993; 2008-2009.
- Enosolease ME, Bazuaye GN. Distribution of ABO and Rh- D blood groups in the Benin area of Niger-Delta: Implication for regional blood transfusion. Asian J Transf Sci 2008; 2 (1): 3-5.
- Reddy KSN, Sudha G. Rh (D) blood groups among the desuri Reddis of Chittoor District, Andhra Pradesh. Anthropologist. 2009; 11 (3): 237-238.
- Talukder SI, Das RK Distribution of ABO and Rh Blood Groups among Blood Donors of Dinajpur District of Bangladesh. Dinajpur Med Col J 2010; 3: 55- 58.