Research Article - Journal of Clinical Ophthalmology (2022) Volume 6, Issue 4
Prevalence of dry eye disease among Hail University staff and students.
Talal F Alharbi1, Khalid I Alrehili1, Moath Z Alaodah1, Mubashir Zafar2, Abrar Ali1, Nabeel Shalabi1*1Department of Ophthalmology, Hail University, Hail, Saudi Arabia
2Department of Community Medicine, Hail University, Hail, Saudi Arabia
- Corresponding Author:
- Dr. Nabeel Shalabi
Department of Ophthalmology
Hail University
Hail, Saudi Arabia
E-mail: n.shalabi@uoh.edu.sa
Received: 24-May-2022, Manuscript No. AACOVS-22-64766; Editor assigned: 27-May-2022, PreQC No. AACOVS-22-64766 (PQ); Reviewed: 10-Jun-2022, QC No. AACOVS-22-64766; Revised: 20-Jun-2022, Manuscript No. AACOVS-22-64766 (R); Published: 30-Jun-2022, DOI: 10.35841/aacovs.6.4.544-547.
Citation:Alharbi TF, Alrehili KI, Alaodah MZ, et al. Prevalence of dry eye disease among Hail University staff and students. J Clin Ophthalmol 2022;6(4):544-547.
Abstract
Purpose: This study aimed to estimate the prevalence of dry eye disease among Hail University staff and students. To investigate the Dry Eye Disease (DED) associated risk factors among Hail University staff students.
Patients and methods: A cross sectional study was conducted in Hail University during February 2022 using an electronic-based Ocular Surface Index (OSDI) questionnaire.
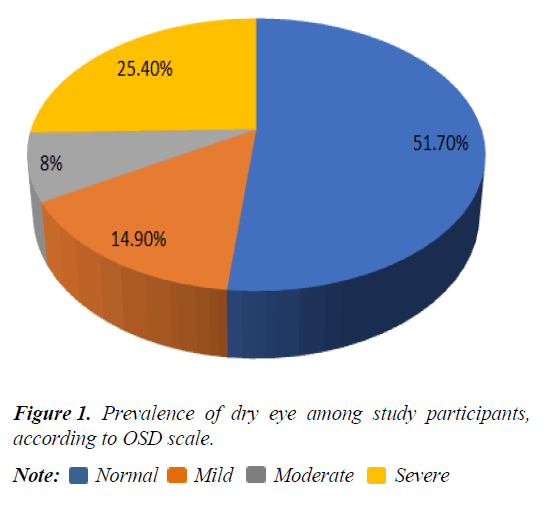
Results: A total 350 university students and staff completed the survey questionnaire. Participants were classified according to four groups, about half (48.3%) of participants were suffered from dry eyes, 14.9% had mild DES, 8% had moderate DES and 25.4% had severe DES according to OSDI score.
Conclusion: DED is common among university students and staff. These findings highlight the continued importance of research and therapeutic development for this common condition.
Keywords
Dry eye disease, Dry eyes, Ocular surface disorder.
Introduction
Dry Eye Disease (DED) is a common ocular surface disorder that considered a public health problem due to its impact on vision-related quality of life of the affected subjects [1-3]. According to the recent official report of the International Dry Eye Workshop (DEWS 2017), that based on summary of the findings of current research, DED was defined as “Dry eye is a multi-factorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles” [4]. Dry eye symptoms include eye dryness, foreign body sensation, and burning sensation, eye redness and discomfort. The condition is aggravated usually at hot, dry climate which is specifically relevant to Saudi Arabia [5-9]. In addition, early detection of dry eyes is important because it can indicate the presence of systemic diseases, such as systemic lupus erythematosus, rheumatoid arthritis, and Sjogren’s syndrome [10].
A review of the literature showed that the prevalence of DED in the Middle East has not been frequently studied. However, according to the few studies reported in the region; the prevalence was noticeably high. For example, in the Kingdom of Saudi Arabia (KSA), DED was reported at a prevalence of 93.2% in one city on the basis of presence of one or more DED symptoms occurring often or most of the time, along with presence of one or more of the dryness signs revealed by clinical tests [1]. Some studies have found an association between smoking, wearing contact lenses, the amount of daily screen time, and dry eyes [11,12]. Approximately 5%-50% of world’s population is affected by this condition [14]. Asian countries (e.g. Japan, Korea, Thailand, and China) have been found to have higher prevalence of DED compared to other countries in America and Europe [15-21]. There are few published articles related to the prevalence of dry eyes in Hail city, Saudi Arabia, and none were found in Hail university population. Therefore, this study is the first to estimate both the scope and the burden of the disease in Hail university population. It is vital to identify the prevalence and severity of dry eyes to suggest future public health measures that can raise awareness and explore ways to alleviate dry eyes. Our study aimed to explore the prevalence and potential risk factors of DED among students and staff at Hail University, Hail.
Methodology
Study setting, study participants and study design
Study was conducted in Public Sector University. This is the cross-sectional study.
Sampling technique and sample size
The participants selected through convenient sampling technique. Sample size calculated from world health organization sample size calculator for health studies software, 5% margin of error with 95% Confidence interval, 35% prevalence of dry eye from previous study, the required sample size is 350.
Data collection procedure and study instruments
This study was approved by ethics committee at University of Hail. The questionnaires distributed among study participants electronically. A validated, and structured questionnaire will be used, the internal validity and reliability of questionnaire has been found very high [8,11]. The reliability of the items in each domain and overall was assessed using Cronbach’s alpha coefficients at a 95% CI and value of the tool was 0.78 (95% CI: 0.76-0.81). The questionnaire had pretested, find out any inconsistency of responses and modification of questionnaire according to response from study participants, and build a final version of questionnaire.
The OSDI questionnaire on dry eye symptoms was used and translated into Arabic. There are two section of questionnaire, first is the Socio-demographic data and medical history of each participant.
Scoring
The grading used was on a scale from 0 to 4, where 0 denoted none; 1: Some; 2: Half; 3: Most; and 4: All of the time. The total score is commonly estimated on the basis of the following formula; OSDI=[sum of the scores for all questions answered × 100]/total number of questions answered] × 4 [16]. The contribution of contact lenses to the pathology, incidence and severity of the DES was studied to determine the frequency of these events. The total score was calculated on a scale of 0 to 100, with higher scores representing greater distress. Scores 0 to 12 representing normal, 13 to 22 representing mild dry eye disease, 23 to 32 representing moderate dry eye disease, and greater than 33 representing severe dry eye disease.
Statistical analysis
Data analysis was done in Statistical Package of Social Science Software program (SPSS) version 22.0 software (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp). Descriptive statistics in the form of mean, standard deviation, frequency, and percentage used for data summarization, OSD scores was converted into categories i.e. mild, moderate, severe Inferential statistical analysis used by logistic regression models to test association of risk factors of dry eye with the OSD score. P-value of <0.05 will be considered as statistical significance.
Results
Characteristics of study participants
Mean age of study participants was 23.58 ± 1.51 SD, most (83.1%) of them were students and 56.3% were male students. Few (2.9% and 4.3%) of participants were have diabetes and Thyroid dysfunction. Fifteen percent participants were used contact lenses (Table 1).
| Characteristics | Frequency (%) |
|---|---|
| Age (Years) (Mean ± SD) | 23.48 ± 1.51 |
| 18-20 | 165 (47.1) |
| 21-60 | 185 (52.9) |
| Gender | |
| Male | 197 (56.3) |
| Female | 153 (43.7) |
| Smoking | |
| Ever | 49 (14) |
| Never | 301 (86) |
| Occupation | |
| Students | 291 (83.1) |
| Employee | 59 (16.9) |
| Diabetes Mellitus(DM) | |
| Yes | 10 (2.9) |
| No | 340 (97.1) |
| =Thyroid Dysfunction(TD) | |
| Yes | 15 (4.3) |
| No | 335 (95.7) |
| Past Surgical History of Eye | |
| Yes | 17 (4.9) |
| No | 333 (95.1) |
| Contact Lens Use | |
| Yes | 54 (15.4) |
| No | 296 (94.6) |
Table 1. Clinical and demographic characteristics of study participants (n=350).
Prevalence of dry eye among study participants
Participants were classified according to four groups, about half (48.3%) of participants were suffered from dry eyes, 14.9% had mild DES, 8% had moderate DES and 25.4% had severe DES according to OSDI score (Figure 1).
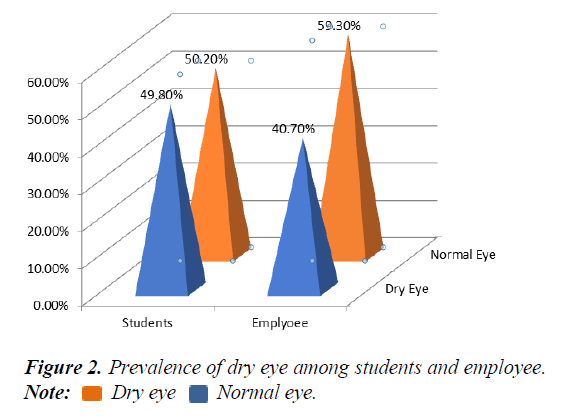
Prevalence of dry eye among students and university employee
Nearly half (49.8%) of students were had DES and 40.7% of employee were had DES according to OSDI score (Figure 2).
Risk factors affecting the prevalence of DES
Logistic regression test used to study the association between risk factors and eye dryness, there was no statically significant association between those risk factors variables and dry eyes (Table 2).
| Characteristics | Dry eyes un-adjusted Odd Ratio OR (95%Confidence Interval CI) (p-value) | Dry eyes adjusted odd Ratio OR (95% Confidence Interval CI) |
|---|---|---|
| Age category (years) | ||
| 18-20 | 1 | 1 |
| 21-60 | 1.22 (0.80-1.85) (0.354) | 1.14 (0.72-1.82) (0.561) |
| Gender | ||
| Female | 1 | 1 |
| Male | 1.15 (0.75-1.76) (0.501) | 0.98 (0.60-1.60) (0.949) |
| Smoking | ||
| Ever | 1 | 1 |
| Never | 1.06 (0.58-1.95) (0.839) | 0.93 (0.48-1.78) (0.833) |
| Occupation | ||
| Student | 1 | 1 |
| Employee | 4.54 (2.81-7.98) (0.030) | 1.35 (0.72-2.54) (0.341) |
| Contact lens use | ||
| No | 1 | 1 |
| Yes | 1.54 (0.85-2.72) (0.147) | 0.62 (0.32-1.18) (0.151) |
| LASIK operation | ||
| No | 1 | 1 |
| Yes | 1.75 (0.63-4.86) (0.277) | 1.51 (0.52-4.34) (0.442) |
| Diabetes | ||
| No | 1 | 1 |
| Yes | 1.41 (0.39-5.10) (0.596) | 1.17 (0.31-4.45) (0.813) |
| Thyroid dysfunction | ||
| No | 1 | |
| Yes | 1.64 (0.57-4.71) 0.358 | 1.96 (0.66-5.83) (0.222) |
Table 2. Association of dry eyes with risk factors among study participants (n=350).
Discussion
Few studies have investigated the prevalence of DED in Hail city. This is the first population-based study regarding prevalence of DED in Hail University population. In the study, the OSDI questionnaire was used to assess the presence of symptomatic DED.
The current study participants were classified according to four groups, about half (48.3%) of participants were suffered from dry eyes, 14.9% had mild DES, 8% had moderate DES and 25.4% had severe DES according to OSDI score. In comparison with other dry eye disease epidemiological surveys that also adopted the same DED diagnostic criteria based on OSDI questionnaires, a study focusing on the prevalence of DED among Mexican high school students revealed that 65.3% of the students suffered from symptomatic DED [23]. The prevalence reported in our study was higher than that in the above-mentioned study.
Considering the high prevalence of DED among Hail university population in the current study, we speculated that it may attribute to long online courses and heavy stress. The high prevalence might be attributed to several factors mainly related to the arid climate with temperature ranging from 30 to 40°C during summer seasons. Selection bias is a limitation of the study as it was limited to Hail university population who could access the internet, which limits the generalizability of our results. This study aimed to explore the prevalence of dry eye disease among Hail University staff and students, and to investigate the Dry Eye Disease (DED) associated risk factors among Hail university staff students.
Further research is recommended to better understand other potential risk factors associated Dry Eye Disease (DED), and answering other potential among society. Finally, this is the first study of the prevalence of DED in a previously unstudied population in Hail university population. It was found that the prevalence of DED is relatively high in this study. An attempt should be performed to increase the awareness of the society with DED, so modifiable risk factors can be reduced. However, further research is required to better understand other potential risk factors associated with DED including; impact of arid environment, drug use, systemic diseases and anxiety.
Conclusion
In conclusion, this is the first study of the prevalence of DED in a previously unstudied population in Hail university population. It was found that the prevalence of DED is relatively high in this study. An attempt should be performed to increase the awareness of the society with DED, so modifiable risk factors can be reduced. However, further research is required to better understand other potential risk factors associated with DED.
References
- Bukhari A, Ajlan R, Alsaggaf H. Prevalence of dry eye in the normal population in Jeddah, Saudi Arabia. Orbit. 2009; 28:392-7.
[CrossRef] [Google Scholar] [PubMed]
- Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276-83.
[CrossRef] [Google Scholar] [PubMed]
- Grubbs JR, Tolleson-Rinehart S, Huynh K, et al. A review of quality of life measures in dry eye questionnaires. Cornea. 2014;33:215-8.
[CrossRef] [Google Scholar] [PubMed]
- Lemp CM. Report of the national eye institute/industry workshop on clinical trials in dry eyes. Eye Contact Lens. 1995; 21:221.
[Google Scholar] [PubMed]
- Lemp MA, And GN, Foulks FACS. The definition & classification of dry eye disease guidelines from the 2007 International Dry Eye Workshop. 2008.
- Ohashi Y, Ishida R, Kojima T, et al. Abnormal protein profiles in tears with dry eye syndrome. Am J Ophthalmol. 2003;136:291-9.
[CrossRef] [Google Scholar] [PubMed]
- Kaercher T, Bron AJ. Classification and diagnosis of dry eye. Dev Ophthalmol. 2008; 41:36-53.
[CrossRef] [Google Scholar] [PubMed]
- Schaumberg DA, Sullivan DA, Dana MR. Epidemiology of dry eye syndrome. Adv Exp Med Biol. 2002;506:989-98.
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Smith JA. The epidemiology of dry eye disease. Acta Ophthalmol Scand. 2007.
[CrossRef]
- Findlay Q, Reid K. Dry eye disease: when to treat and when to refer. Aust Prescr. 2018;41:160-3.
[CrossRef] [Google Scholar] [PubMed]
- Titiyal J, Falera R, Kaur M, et al. Management of late-onset flocculent after-cataract with capsular bag lavage and posterior continuous curvilinear capsulorhexis. Indian J Ophthalmol. 2018;66:984.
[CrossRef] [Google Scholar] [PubMed]
- Markoulli M, Kolanu S. Contact lens wear and dry eyes: challenges and solutions. Clin Optom (Auckl). 2017;9:41-8.
[CrossRef] [Google Scholar] [PubMed]
- Bhavsar AS, Bhavsar SG, Jain SM. A review on recent advances in dry eye: Pathogenesis and management. Oman J Ophthalmol. 2011;4:50-6.
[CrossRef] [Google Scholar] [PubMed]
- Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334-65.
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Uchino M, Nishiwaki Y, Michikawa T, et al. Prevalence and risk factors of dry eye disease in Japan: Koumi study. Ophthalmology. 2011;118:2361-7.
[CrossRef] [Google Scholar] [PubMed]
- Ahn JM, Lee SH, Rim THT, et al. Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010-2011. Am J Ophthalmol. 2014;158:1205-14.
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Lekhanont K, Rojanaporn D, Chuck RS, et al. Prevalence of dry eye in Bangkok, Thailand. Cornea. 2006;25:1162-7.
[CrossRef] [Google Scholar] [PubMed]
- Jie Y, Xu L, Wu YY, et al. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. EYE. 2009;23:688-93.
[CrossRef] [Google Scholar] [PubMed]
- Schaumberg DA, Sullivan DA, Buring JE, et al. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318-26.
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Schaumberg DA, Dana R, Buring JE, et al. Prevalence of dry eye disease among US men: estimates from the Physicians’ Health Studies: Estimates from the physicians’ health studies. Arch Ophthalmol. 2009;127:763-8.
[CrossRef] [Google Scholar] [PubMed]
- Viso E, Rodriguez-Ares MT, Gude F. Prevalence of and associated factors for dry eye in a Spanish adult population (the Salnes Eye Study). Ophthalmic Epidemiol. 2009;16:15-21.
[CrossRef] [Google Scholar] [PubMed]
- Asiedu K, Kyei S, Mensah SN, et al. Ocular Surface Disease Index (OSDI) versus the Standard Patient Evaluation of Eye Dryness (SPEED): A study of a nonclinical sample. Cornea. 2016;35(2):175-180.
[CrossRef] [Google Scholar] [PubMed]
- Garza-León M, López-Chavez E, De La Parra-Colín P. Prevalence of Ocular Surface Disease Symptoms in High School Students in Monterrey, Mexico. J Pediatr Ophthalmol Strabismus. 2021;58:287-91
[CrossRef] [Google Scholar] [PubMed]