- Biomedical Research (2016) Volume 27, Issue 3
Prevalence and distribution of high-risk human papillomavirus in amasya region, Turkey.
Rıdvan Güçkan1*, Çetin Kılınç1, Elif Gözdemir2, Atiye Aysemin Gürçağlar2, Öner Nergiz31Laboratory of Microbiology, Amasya Sabuncuoglu Serefeddin University, Training and Research Hospital, Amasya, Turkey
2Department of Obstetrics and Gynecology, Amasya Sabuncuoglu Serefeddin University, Training and Research Hospital, Amasya, Turkey
3Institute of Public Health, Amasya, Turkey
- *Corresponding Author:
- Ridvan Güçkan
Department of Microbiology
Amasya Sabuncuoglu Serefeddin University
Turkey
Accepted date: February 28, 2016
Abstract
Aim: In this study, the aim is to determine the HPV DNA prevalence and the genotype distribution of High Risk HPVs in women who came to Amasya Cancer Early Diagnosis, Screening and Education Center (KETEM) for screening.
Materials and methods: Totally 7992 women between the ages of 30-65 were included in the study between August, 2014 and August, 2015. HC II HPV DNA test (Digene Corporation, Gaithersburg, MD, USA) was used and HPV DNA presence and HR-HPV type detection studies were performed by using cervical swab samples.
Results: According to our results, 2.7% of the cases were HPV-DNA positive. HPV positivity was detected mostly in women who were between the ages of 30-39 years. In the genotype distribution of HPV positive women, most frequently observed type was HPV16 (23.6%) and then HPV51 was observed with 9% frequency. HR-HPV rates were detected as 77.8% in all HPV positive women.
Conclusion: HPV DNA positivity rate was low in our province. However, the high positivity of HR-HPV types detected in HPV positive women let us think that these women should be more careful in their future controls and routine screenings in terms of cervical cancer.
Keywords
Human papillomavirus, Genotype, HR-HPV.
Introduction
Human papillomaviruses (HPV) are members of papillomaviridae family, they have an icosahedral symmetry and they are DNA viruses without envelope and with 72 capsomers which are surrounding their genome [1,2]. It has been shown that HPV, which has more than 200 genotypes, primarily leads to cervical cancer, precursor lesions, and also other genital cancers (vulva, vagina, penis, anus), oropharyngeal cancers, genital warts, laryngeal papillomatosis and some skin cancers as a result of molecular diagnostic methods [3,4]. Cervical cancer is the second most frequent cancer among women throughout the world. Epidemiological and molecular studies have shown that cervical cancers and precursor intraepithelial lesions develop due to either one of the HPVs or subtype of HPVs [5,6]. HPV types are grouped according to their oncogenic risk potentials such as high risk types (HR-HPV), possible high risk types (PrHR-HPV) and low risk types (LR-HPV). High risk types of HPVs for the cervical cancers are HPV subtypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82 [7].
The national standards of cervical cancer screening are determined by Ministry of Health, Head of Cancer Department and the screenings have been applied in Cancer Early Diagnosis, Screening and Education Centers (KETEM). Recently, vaccines have been developed against high risk HPV types and they are also used in Turkey. This shows the importance of the regional HPV frequencies and HPV type distributions.
This study was performed in order to determine the HR-HPV type distributions which were detected in HPV infections. Furthermore, it was also aimed to contribute to the epidemiological data that can assist us to foresee the possible effects of HPV vaccines in Turkey.
Materials and Methods
This study was approved by Committee of Institute of Public Health, Amasya in the scientific meeting which was held on 17.08.2015.
Totally 7992 women between 30 and 65 years old and who applied to Cancer Early Diagnosis, Screening and Education Centers (KETEM) for screening between August, 2014 and August, 2015 were included in the study. This center is affiliated to Amasya Directorate of Public Health. Amasya is in the middle of the Blacksea region, in Turkey. Individuals, who are living in Amasya region, are not generally from different ethnic backgrounds, they are monogamous, they are engaged in agriculture and their socio-economic level is low.
Cervical samples were obtained from women who were not in the menstruation period, who did not have vaginal treatment in the last three days, who did not receive vaginal acetic acid and iodine solution before the test, who did not have sexual activity in the last 24 hours. Swab samples were collected from endocervical place by using sterile swab rod (HC2 DNA collection bar). Samples were incubated and transported in a private medium (HC2 DNA Digene transport medium) to Turkey National Health Agency for the positivity and type determination. Laboratory findings of patients who had the HPV DNA screening and type identification were assessed retrospectively. HR-HPV type identification was done by using HC II HPV DNA test (Digene Corporation, Gaithersburg, MD, USA). The Hybrid Capture II (hcII) test is a nucleic acid hybridization assay where specimens containing the target DNA hybridize with a specific HPV RNA probe mixture including probes for 13 High-Risk HPV types. The resultant DNA: RNA hybrids are captured on a microplate coated with antibodies specific for DNA: RNA hybrids. After signal detection with antibodies conjugated with alkaline phosphatase and substrate, the emitted light is measured in a luminometer as relative light units (RLU). Samples are classified as positive for HR HPV if the relative light unit (RLU) reading is above 1.0, which (according to the manufacturer) is equivalent to 1 pg HPV DNA/mL.
Results
Out of 7992 women whose HPV screening was performed, 220 of them had HPV positivity (2.7%). According to the age range, the highest HPV positivity was in women between the ages of 30 to 39 years.
It was detected that HPV positivity was 2.3% in women between the ages of 40 to 49 and 2.1% between the ages of 50 to 59. Furthermore, there was a slight increment in the rates in case of women who were older than 60 years old (2.2%) (Table 1).
| Age | HPV negative | HPV positive | % of positivity |
|---|---|---|---|
| 30-39 | 1813 | 83 | 4.3% |
| 40-49 | 2600 | 63 | 2.3% |
| 50-59 | 2417 | 52 | 2.1% |
| >60 | 942 | 22 | 2.2% |
| Total | 7772 | 220 | 2.7% |
Table 1. HPV positivity rates according to age.
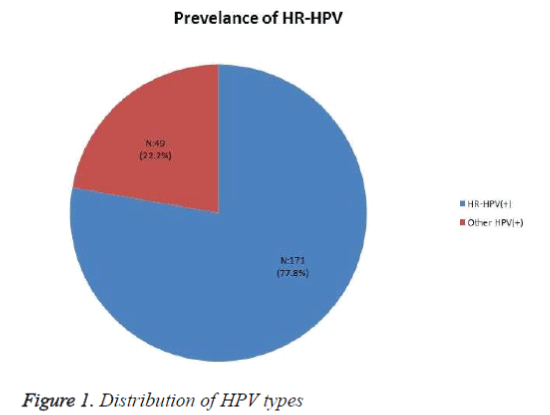
Out of 220 HPV positive patients, 171 of them (77.8%) had HR-HPV types, 49 of them (22.2%) had low and possible risk HPV types (Figure 1).
According to high risk HPV type distributions, 52 patients had HPV16 (23.6%), 20 patients had HPV51 (9%), 19 patients had HPV31 (8.6%), 14 patients had HPV 39 (6.3%), 11 patients had HPV52 (5%), 10 patients had HPV18-HPV56-HPV58 (4.5%), 7 patients had HPV35-HPV68 (3.1%), 5 patients had HPV45 (2.2%), and 3 patients had HPV33-HPV59 (1.3%) (Table 2). In all HPV positive women, the rate of HPV16 and HPV18, which play the maximum role in the etiology of cervical cancer, were detected as 28.1%.
| HR-HPV Types | N | % |
|---|---|---|
| HPV 16 | 52 | 23.6 |
| HPV18 | 10 | 4.5 |
| HPV 31 | 19 | 8.6 |
| HPV 33 | 3 | 1.3 |
| HPV 35 | 7 | 3.1 |
| HPV 39 | 14 | 6.3 |
| HPV 45 | 5 | 2.2 |
| HPV 51 | 20 | 9 |
| HPV 52 | 11 | 5 |
| HPV 56 | 10 | 4.5 |
| HPV 58 | 10 | 4.5 |
| HPV 59 | 3 | 1.3 |
| HPV 68 | 7 | 3.1 |
| Other HPV (+)* | 49 | 22.2 |
| Total | 220 | 100 |
Other HPV*:Low risk HPV and possible risk HPV
Table 2. HR-HPV prevalence between 7992 samples.
Discussion
Cervical cancer is an important health issue among women. Due to the presence of pre-invasive lesions and since it is easily accessible organ, cervical cancer is a convenient cancer for early diagnosis. The effectiveness of cervical cancer screening methods is improved and effective screening is thought to decrease the invasive cancer prevalence and mortality. Most frequently used screening tests are pap-smear and HPV-DNA detection tests [8,9]. Cytology screening is beneficial and it leads to significant decrease in the incidence and mortality rates of cervical cancer. However, it can be possible to overlook the diagnosis of the disease in women due to the low sensitivity of cytology screening [10,11]. It has been shown that HPV positivity rates were detected between 14.5% and 16.6% among women who have cervical cytology [12].
The most important risk factor in the cervical cancer development is HPV presence and it is possible to detect the presence of HPV by DNA analysis in the cervical samples of patients. According to studies, HPV-DNA positivity rates vary in different countries and even in different regions of Turkey. According to a meta-analysis study in which HPV-DNA prevalence of women with normal cervical cytology was examined, HPV-DNA prevalence was found as 10.4%. It was comparatively higher in Africa, Middle America and Mexico (almost 20-30%) and comparatively lower in North America, Europe, and Asia (almost 11%) [13]. In Turkey, Altun et al. [14] have stated that the HPV positivity rate is 5.2% in Adana, Yıldırım et al. [15] have shown that it is 6.4% in Sivas and Akçalı et al. [16] have reported that it is 8.5% in Manisa (2013). In our study, HPV positivity was 2.7%. HPV DNA positivity rates detected in our province was lower in comparison with HPV positivity rates in Turkey. Wide ranges of HPV prevalence rates that are shown in national and international studies can be due to the social differences and cultural diversity in geographical regions. However, different methods and differences in the molecular sensitivities can also lead to these different findings. Also HPV vaccination has not yet been included in the vaccination calendar in Turkey. Vaccination is optional and has also a certain fee. Thus, there is no data with respect to the number of patients who had received the HPV vaccine.
It has been shown in some studies that age has an important effect on HPV prevalence. Epidemiological studies have indicated that HPV infection prevalence among 18-25 years old young women is higher compared to the prevalence among women who are 30 years old or older. Thus, it has been stated that as the age increases, HPV prevalence decreases [17]. De Sanjose et al. [13] performed a study (2007) in which they examined the 346,000 women from 70 countries, they detected a difference in age dependent HPV prevalence according to region and population. In most of the regions, HPV frequency increased in women who were around 25 years old. In a study which was performed in the USA in order to assess HPV prevalence according to age, it was detected that HPV prevalence was highest in women who were between the ages of 20 and 24 years [18]. In Turkey, Yıldırım et al. [15] and Akçalı et al. [16] reported that there was no significant relationship between age and HPV prevalence. In our study, HPV prevalence (4.3%) was shown mostly in women who were between 30 and 39 years old as it was shown in study performed in Altun et al. [14].
HR-HPV types were detected in 89% of the cervical cancers in the world [19]. Out of HR-HPV genotypes, HPV-16 and HPV18 have higher risks for pre-cancer compared to other types [20]. HPV16 leads to 50% and 60% of the cervical cancers and HPV18 leads to 10%-12% of the cervical cancers [5]. HPV16 and HPV18 have higher risks for pre-cancerous lesions and cervical cancer and this can provide an important opportunity to clinicians when they decide which genotypes should be considered as risky and which treatments are effective in order not to have cervical cancer due to the HRHPV infection.
Even though the frequency of HPV types change, HPV16 and HPV18 types are the most common ones [7]. Bruni et al. [21] performed a study in 2010 in which they conducted metaanalysis in 1 million women who had normal cytology. They reported that the most commonly observed types were HPV-16, 18, 52, 31, 58, 39, 51, and 56; respectively. In Turkey, Fındık et al. [22] and Altun et al. [14] indicated that the most common type was HPV16 (18.7%), Akçalı et al. [16] stated that the most common ones were HPV-16, 45 and 53; respectively. Unlike various national studies, Yıldırım et al. [15] detected the most frequently observed type was HPV6 (25%) and Eroğlu et al. [23] showed it was HPV18. In our study, similar to various national and international studies, HPV16 was determined as the most commonly observed HPV type among HPV positive women (23.6%). HPV51 (9%) and HPV31 (8.6%) were the other most commonly observed HPV types. HPV18, which is the second most frequent reason for cervical cancer, was detected as 4.5% whereas its prevalence was lower compared to other HR-HPV types. In our region, HR-HPV rates were 77.8% in all HPV positive women.
In the world and also in Turkey, there are 2 HPV vaccines (dual and quadrivalent vaccines). Dual vaccine provides protection against HPV16 and HPV18 which are the most common reason for cervical cancer and quadrivalent vaccine provides protection against HPV16 and HPV18 as well as HPV6 and HPV11 which cause genital warts [24]. The efficacy of these vaccines in the population is directly related to truly identified type distributions at the population level. However, it can be concluded according to national studies that HPV type 18 is not regarded as the first type in vaccinations. Therefore, there should be further studies in order to find the standard method for the determination of HPV type prevalence and HPV types that should be used in vaccines. These studies should be more comprehensive and similar patient and control groups should be included in these studies.
Conclusively, even though HPV positivity in our region has been found lower in other national and international regions, women who are under the risk of cervical cancer should be closely followed and certain precautions should be taken in women who have high positivity of oncogenic HPV types.
PS: Data obtained from Amasya Institute of Public Health were used in our study.
References
- Munoz N, Castellsague X, de Gonzalez AB, Gissmann L. Chapter 1: HPV in the etiology of human cancer. Vaccine 2006; 24: 1-10.
- Trottier H, Burchell AN. Epidemiology of mucosal human papillomavirus infection and associated diseases. Public Health Genomics 2009; 12: 291-307.
- American Cancer Society: Detailed guide: Cervical cancer, Am Cancer Soc 2005.
- Burd HM. Human papilloma virus and cervical cancer, ClinMicrobiol Rev 2003; 16: 1-17.
- Bosch FX, Sanjose S. Human papillomavirus and cervical cancer-burden and assessment of causality, J Natl Cancer Ins Monogr 2003; 31: 3-13
- Schlecht NF, Kulaga S, Robitaille J, et al.Persistant human papillomavirus infection as a predictor of cervical intraepithelial neoplasia, JAMA 2001; 286: 3106-3114.
- Psyrri A, DiMaio D. Human papillomavirus in cervical and head-and-neck cancer. Nat ClinPractOncol 2008; 5: 24-31.
- Arvas M, Gezer A. HPV DNA Tests. In: Arvas M, Gezer A (eds). Genital HPV. Istanbul Medical Publishing2007; 93-106.
- Wu S, Meng L, Wang S, Ma D. A comparison of four screening methods for cervical neoplasia. Int J GynaecolObstet 2005; 91: 189-193.
- Saslow D, Solomon D. Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. Am J ClinPathol2012; 137:516-542.
- Castle PE, Stoler MH, Wright TC Jr, Sharma A, Wright TL, Behrens CM. Performance of carcinogenic human papillomavirus (HPV) testing and HPV16 or HPV18 genotyping for cervical cancer screening of women aged 25 years and older: a subanalysis of the ATHENA study.
- Perez G, Lazcano-ponce E, Hernandez-Avila M, et al. Safety immunogenicity and efficacy of quadrivalent human papilo-mavirus (type 6, 11, 16, 18) L1 virus-like particle vaccine in Latin American women. Int J Cancer 2008; 122: 1311-1318.
- de Sanjosé S, Diaz M, Castellsagué X, Clifford G, Bruni L, Muñoz N, Bosch FX: Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis 2007; 7:453-459.
- Altun Z, Yarkın F, Vardar MA, Uğuz AH. The prevalence of human papilloma virus infection among women who admitted to çukurova university faculty of medicine hospital. J Med Sci 2011; 31: 307-314.
- Yıldırım D, Yıldırım ME, Bakıcı MZ . Human Papillomavirus Positivity and Frequency of Genotypes in Servical Samples of Women Living in Sivas Region, , Firat Med J 2013; 18: 94-97
- Akcali S, Goker A, Ecemis T, Kandiloglu AR, Sanlidag T. Asian Pac J Cancer Prev2013; 14:503-506.
- Yarkın F. Virology and epidemiology ofhumanpapillomavirus infections. Actual Medicine Clinic 2007; 12:1-6.
- Dunne EF, Unger ER, Stenberg M, et al. Prevalence of HPV infection among females in the United States. JAMA 2007; 297: 813-819.
- Clifford G, Franceschi S, Diaz M, Munoz N, Villa LL. HPV type distribution in women with and without cervical neoplastic diseases. Vaccine 2006; 24: 26-34.
- Khan MJ, Castle PE, Lorincz AT, et al. The elevated 10-year risk of cervical precancer and cancer in women with human papillomavirus (HPV) type 16 or 18 and the possible utility of type-specific HPV testing in clinical practice. J Natl Cancer Inst 2005; 97:1072-1079.
- Bruni L, Diaz M, Castellsagué X, Ferrer E, Bosh FX, de Sanjosé S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with nomal cytological findings.J Infect Dis 2010; 202:1789-1799
- Fındık D, TürkDağı H, Arslan U, Fındık Y. Frequency and genotype distribution of human papillomavirus in cervical specimens. General Medical Journal 2012; 22:116-20.
- Eroğlu C, Keşli R, Eryılmaz MA. Ünlü Y, Gönenç O, Çelik Ç.Hpv Types and The Relation of HPV Prevalence to Risk Factors and Cervical Smear in Women at Risk for Cervical Cancer Nobel Med 2011; 7: 72-77
- CDC. Human papillomavirus vaccination. Recommendations of the Advisory Committee on Immunization Practices (ACIP). 63:1-30.