Case Report - Ophthalmology Case Reports (2023) Volume 7, Issue 5
Preseptal cellulitis and lid abscess secondary to necrotizing fasciitis of scalp: Case report.
Sherein M. Hagras*, Yossef G. ElHerz, Mona A. Nasief, Amna A. AlrashidiDepartment of Ophthalmology, Farwanyia Hospital, Farwanyia, Kuwait
- *Corresponding Author:
- Sherein M. Hagras
Department of Ophthalmology
Farwanyia Hospital, Farwanyia, Kuwait
E-mail: sherienhagras@gmail.com
Received: 08-Aug-2023, Manuscript No. OER-23-113516; Editor assigned: 10-Aug-2023, Pre QC No. OER-23-113516 (PQ); Reviewed: 24-Aug-2023, QC No. OER-23- 113516; Revised: 26-Sep-2023, Manuscript No. OER-23-113516 (R); Published: 03-Oct-2023, DOI: 10.35841/oer-7.5.171
Citation: Hagras SM, ElHerz YG, Nasief MA, et al. Preseptal cellulitis and lid abscess secondary to necrotizing fasciitis of scalp: Case report. Ophthalmol Case Rep. 2023;7(4):171.
Abstract
Necrotizing fasciitis is a rapidly progressing soft tissue infection with extensive necrosis of subcutaneous fat and fascia while sparing the skin and the underlying muscle. It is usually caused by toxin producing virulent bacteria. Though it can occur in previously healthy patients, the disease is usually seen in immune-compromised patients. Rarely involves the head and neck structures. We present a case of with necrotizing fasciitis of the scalp extending to upper eyelid with abscess formation secondary to Streptococcus agalactiae infection in uncontrolled diabetic patient. Early recognition and prompt surgical debridement were critical in the favorable outcome of the case.
Keywords
Necrotizing fasciitis, Preseptal Cellulitis, Lid Abscess.
Introduction
Necrotizing Fasciitis (NF) is an uncommon, rapidly progressive soft tissue infection characterized by cutaneous gangrene, suppurative fasciitis, and vascular thrombosis. NF occurs most frequently in the limbs or abdominal wall. The disease usually occurs in immune compromise conditions as diabetes, alcoholism, malignancy, corticosteroid use, and chronic systemic disease. Nevertheless, about half of the reported cases were diagnosed in otherwise healthy individuals [1]. Periorbital location is significantly less common, owing to the rich blood supply to the head and neck. The condition typically follows blunt or penetrating trauma. However- in the head and neck region- it can be caused by dental or pharyngeal infections [2]. Eyelid involvement in NF is rare, with only few cases reported over the past years, carrying an associated mortality from 10 to 18% [3,4]. We report a case of preseptal cellulitis with upper lid abscess secondary to necrotizing fasciitis in the scalp.
Case report
A 42year-old Pakistani male patient was brought by the ambulance to the Emergency Department (ED) of Farwanyiah hospital with marked swollen forehead, pus pointing all over the skin and drippling from the right side of the scalp with marked swelling in both upper eyelids. The patient was found unconscious in his home. The condition started 10 to 15 days ago with painless lesion in the scalp, without any predisposing factors. He had no significant past medical history.
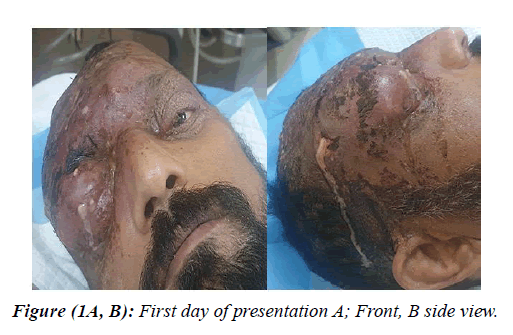
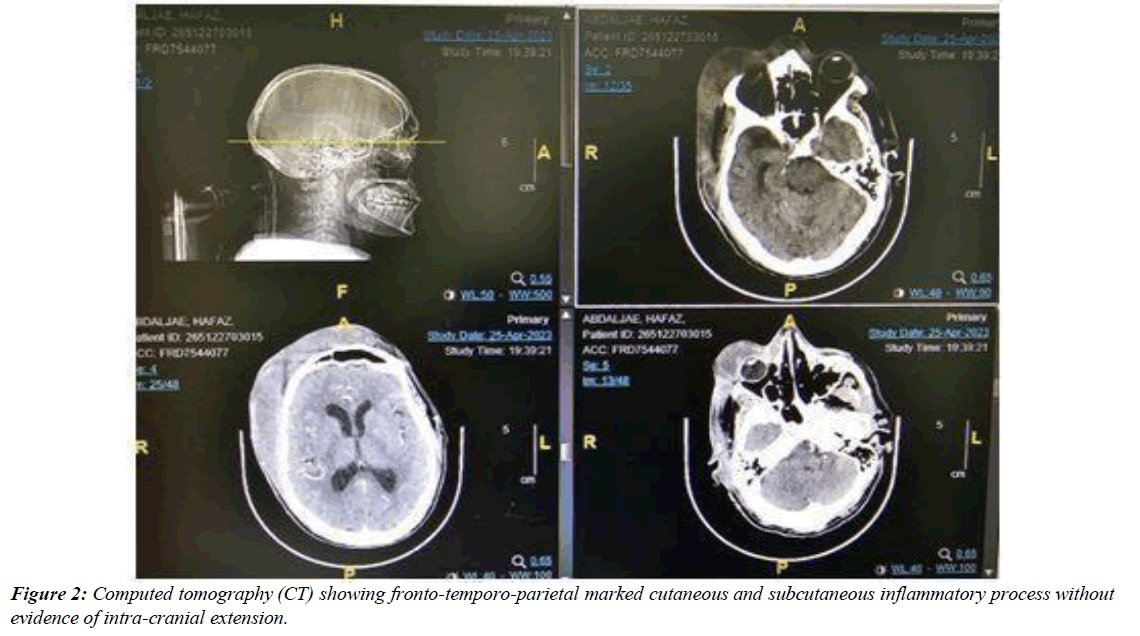
Ophthalmic initial examination showed multiple pus-filled blisters and a bluish discoloration in the skin of the scalp and forehead and with dried scales. The lid swelling was extensive that precluded right eye examination. The left eye showed normal eye movements, and healthy anterior and posterior segments (Figure 1). Skin swabs and blood cultures were taken, and intravenous Ceftriaxone 1g, Metronidazole 500mg and Meropenem 1g were commenced. Initial blood tests revealed neutrophil leukocytosis (white blood cell count 22.9 x109 /L, 76.8 % neutrophils), and an elevated C-Reactive Protein (CRP) level of 111 mg/dL (reference range, < 8 mg/L). High blood sugar level (12.1mmol/L), lactate levels 0f 1.57 m mol/L and Hepatitis -B positive. The general condition of the patient was not stable developing acute kidney insult (Albumin<10g/L and creatinine level of 165umol/L). Computed Tomography (CT) showed large right fronto-parietal subglaleal soft tissue swelling with marked cutaneous and subcutaneous edema extending to left frontal and temporal regions and both preseptal regions (more on the right side), associated with ill-defined few small fluid density locules (Figure 2), but no orbital cellulitis.
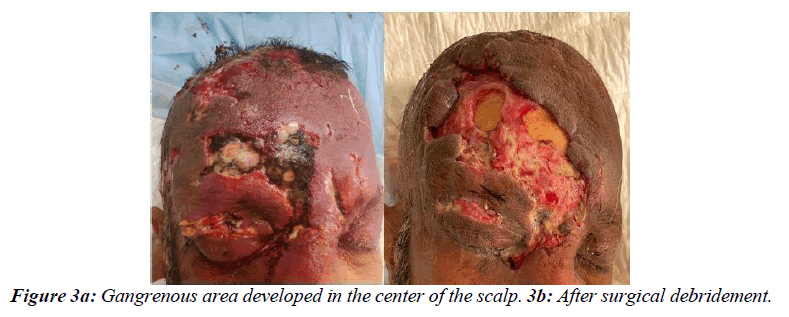
Urgent drainage of right upper lid abscess was done complemented by draining of the scalp pus. Pus was sent for microbiological analysis. Next day, blood culture grew Streptococcus agalactiae and Staphylococcus aureus. Over the next two days frequent drainage of the lid and scalp abscess was carried on. Pus specimen showed growth of Methicillin-Resistant S. aureus (MRSA) so Vancomycin was added. After 2 days a central gangrenous area developed in the scalp (figure 3a). Plastic surgery team was consulted and necrotizing fasciitis was diagnosed clinically, recommending surgical debridement. At surgery, a right upper eyelid abscess was drained again, and surrounding necrotic tissue was debrided down to healthy orbicularis muscle (Figure 3b). Repeated debridement was carried on the next weeks. Histopathology of the scalp debrided tissue revealed marked necrotic tissues with purulent exudate. The debrided area is scheduled for later closure with a skin flap. Last ophthalmic follow up showed resolving of the right upper lid abscess with marked improvement of the periorbital edema with full ocular motility and vision stable bilaterally (Figure 4). Laboratory investigation results mostly returned to normal levels apart from MRSA infection (CRP=7mg/L and WBC dropped to 10.8x109/L, neutrophil 71.2%).
Discussion
Necrotizing fasciitis is a severe infection characterized by a rapid and devasting progression involving the superficial fascia leading to skin necrosis. Periorbital NF is rare in adults and even more so in children as the mean age of diagnosis reported by Lazzeri et al is 50.18 years [5]. One report found preceding local blunt trauma in 17% of cases, penetrating injury in 22%, and facial surgery in 11%, but there was no identifiable cause in one-third of cases [5]. Amrith et al., reported unidentifiable triggers in approximately 27% of cases [6]. Our patient did not report any trauma prior to his condition. He was not taking any medications, though we discovered his high blood sugar, which was unknown for him.
Diagnosis of NF is primarily clinical based on symptoms and disease progression. According to the Infectious Disease Society of America (IDSA) guidelines for NF, features that may help differentiate cellulitis from NF are: severe pain that seems disproportional to clinical findings; failure to respond to initial antibiotic therapy; hard, wooden feeling of the subcutaneous tissue, extending beyond the area of apparent skin involvement; systemic toxicity; edema or tenderness extending beyond the cutaneous erythema; crepitus; bullous lesions; and skin necrosis or ecchymosis [7]. Diagnosis is confirmed with a deep tissue biopsy with gram stain and culture [8]. Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) Score uses values of C-Reactive protein, white blood cells, hemoglobin, sodium, creatinine, and glucose to help distinguish NF from other soft tissue infections [9]. A LRINEC score of greater than 6 warrants further investigation.
In the current study, the patient was not presented with typical clinical signs as IDSA guidelines specially the pain. The patient was not complaining of pain only slight tenderness over the scalp. This might be related to diabetic neuropathy as the patient had uncontrolled DM paired with the dehydrating state of the patient. The wooden texture of the subcutaneous tissue was not evident owing to the fluctuating nature of the pus collection underneath. He was diagnosed as fulminant herpes zoster with secondary bacterial infection from dermatology side. Owing to the critical renal condition of the patient on admission, systemic antiviral medications were held until the skin swab and culture result could confirm the diagnosis. The viral origin of the condition was then ruled out according to the culture results that supported the diagnosis of necrotizing fasciitis.
The most common organism responsible for necrotizing fasciitis is Group A beta hemolytic Streptococcus (GAS) which has been linked to 50% of cases. Streptococcus agalactiae was the causative organism in our case which was also reported in many published studies [6, 10, 11]. In previous reports, fungal infections were also isolated in immunocompetent cases following trauma [12, 13]. One case of herpes zoster ophthalmicus complicated by a staphylococcal super infection in the periorbital area causing necrotizing fasciitis has also been reported [6].
Unlike patients with ‘usual’ periorbital cellulitis who generally do not require surgical intervention except in cases of an eyelid abscess; the mainstay of management for NF is surgical intervention. Serial debridement together with aggressive antibiotic therapy, fluid resuscitation, and blood pressure support are fundamentals for treatment [6]. Our patient received early administration of empirical antimicrobial therapycoverage includes aerobes and anaerobes this was followed by drainage of the abscess. Meanwhile, necrotic tissue started to appear and the diagnosis of NF was established followed by prompt decision for debridement. The patient responded well to the treatment without any ophthalmic complications.
Conclusion
Accurate diagnosis and expeditious treatment is crucial as the infection can extend posteriorly into the orbit causing orbital cellulitis, sub periosteals abscess or orbital abscess. Early initiation of treatment helps to decrease morbidity and mortality.
References
- Amrith S, Hosdurga Pai V, Ling WW. Periorbital necrotizing fasciitis–a review. Acta Ophthalmol. 2013;91(7):596-603.
- Childers BJ, Potyondy LD, Nachreiner R, et al. Necrotizing fasciitis: A fourteen-year retrospective study of 163 consecutive patients. Am Surg. 2002;68(2):109-16.
- Doorenbos-Bot AC, Hooymans JM, Blanksma LJ. Periorbital necrotising fasciitis due to Cryptococcus neoformans in a healthy young man. Doc ;Ophthalmol. 1990;75:315-20.
- Elner VM, Demirci H, Nerad JA, et al. Periocular necrotizing fasciitis with visual loss: pathogenesis and treatment. Ophthalmol. 2006;113(12):2338-45.
- Goldstein EJ, Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: Diagnosis and management. Clin ;Infect ;Dis. 2007;44(5):705-10.
- Jensen SL, Amato JE, Hartstein ME, et al. Bilateral periorbital necrotizing fasciitis. ; ;Arch ;Dermatol. 2004;140(6):664-6.
- Lazzeri D, Lazzeri S, Figus M, et al. Periorbital necrotising fasciitis. Br J Ophthalmol. 2010;94(12):1577-85.
- Lee S, Roh KH, Kim CK, et al. A case of necrotizing fasciitis due to Streptococcus agalactiae, Arcanobacterium haemolyticum, and Finegoldia magna in a dog-bitten patient with diabetes. Korean J ;Lab ;Med. 2008;28(3):191-5.
- Rath S, Kar S, Sahu SK, et al. Fungal periorbital necrotizing fasciitis in an immunocompetent adult. Ophthalmic Plast Reconstr Surg. 2009;25(4):334-5.
- Shayegani A, MacFarlane D, Kazim M, et al. Streptococcal gangrene of the eyelids and orbit. Am ;J ;Ophthalmol. 1995;120(6):784-92.
- Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):10-52.
- Stone LA, Harshbarger III RJ. Orbital necrotizing fasciitis and osteomyelitis caused by Arcanobacterium haemolyticum: a case report. Ophthalmic Plast Reconstr Surg. 2015;31(2):31-3.
- Wong CH, Khin LW, Heng KS, et al. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32(7):1535-41.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref