Research Article - Allied Journal of Medical Research (2017) Volume 1, Issue 1
Preparing medical graduates in Sri Lanka for a productive internship and beyond: The "Good Intern Program"
Padeniya AB1, de Alwis S2, Mahesh B1, Senanayake S1, Ranasinghe D1, De Silva AP3, Ferdinando R4, Mahipala PG5, Dharmagunawardene D2, Epitakaduwa C1, Subramaniam N1, Askin S1, Weerasinghe S1, Herath N1, Jinadasa L1 and Haniffa R3,6*
1Government Medical Officers’ Association, Sri Lanka
2Office of Deputy Director General (Education, Training and Research), Ministry of Health, Sri Lanka
3National Intensive Care Surveillance, Sri Lanka
4National Institute of Health Sciences, Sri Lanka
5Office of Director General of Health Services, Ministry of Health, Sri Lanka
6Network for Improving Critical care Systems and Training, YMBA Building, Sri Lanka
- *Corresponding Author:
- Rashan Haniffa
National Intensive Care Surveillance, Quality Secretariat Building
Castle Street Hospital for Women, Sri Lanka
Tel: 0094 112679038
Fax: 0094 112679039
E-mail: rashan@nicslk.com
Accepted date: 19 June 2017
Citation: Padeniya AB, de Alwis S, Mahesh B, et al. Preparing medical graduates in Sri Lanka for a productive internship and beyond: The “Good Intern Program” Allied J Med Res 2017;1(1):10-15.
DOI: 10.35841/medical-research.1.1.10-15
Visit for more related articles at Allied Journal of Medical ResearchAbstract
Introduction: The transition from undergraduate student to independent practitioner for medical graduates is a challenging one. This paper describes a multi-faceted training model-the “Good Intern Programme (GIP)”-that aims to provide such training for newly qualified doctors (pre-interns, PI) in Sri Lanka.
Methods: The development and implementation of the GIP included the following: focus group discussions to understand the requirements; a needs assessment including identification of the main stressors; a 10-day practical Tamil language-training programme; a 4-day acute care skills training (ACST) program; and a 4-day Good Medical Practice (GMP) workshop based on the system building blocks of the WHO.
Results: 980 PIs participated in the needs assessment; 383 (39.1%) stated that the first half of their internship was more stressful than the second (p<0.003). Amongst the 866 PI who registered for the GIP, 783 (90.4%) considered knowledge of medical administrative matters to be of importance to doctors. Hospital based clinical training, conducted in 28 hospitals island-wide, was attended by 278 PI; a statistically significant increase for all surveyed skills was demonstrated. The feedback for the GMP workshop, attended by 796 PI, was broadly positive with the session on “essential skills for interns” receiving the highest positive rating for relevance.
Conclusion: The GIP provides a comprehensive opportunity to facilitate the transition of medical graduates in Sri Lanka using a multimodal, integrated and sustainable platform. This national program may have applicability beyond Sri Lanka.
Keywords
Good intern program, Internship, Medical education, Good medical practice, training, Lower-middle income country
Introduction
Medical internship is the mandatory first step in the development of a medical professional from a medical graduate [1]. During this period interns are required to contribute significantly to all the six building blocks identified by the World Health organization (WHO) [2]. Studies show that the first year of practice is an extremely challenging and stressful period for new doctors and the term ‘transition shock’ has been used to describe it [3-8]. Interns found the routine administrative tasks and medico legal duties to be stressful [9-11]; the fear of the medico legal consequences of their actions had a negative impact on their learning process [13]. Studies also report low levels of competence in all clinical skills including resuscitation, with potentially negative consequences for both the patients and interns [6,8,10-12]. This possibly gives rise to the ‘July effect’-an increase in morbidity and mortality of patients observed to coincide with the changeover of interns [14,15].
In Sri Lanka more than 1000 medical graduates-around 150 of whom have graduated overseas-begin their internship annually often a year after completing medical school [16]. Although aged 25 years or older, internship is often their first substantive post of employment; the long waiting period, which results in a deterioration of knowledge and skills, and the need to be trilingual add to the pressures they face [17].
This paper describes the “Good Intern Programme” (GIP), a multi-faceted training model based on “Good Medical Practice” [18].
Materials and Methods
The GIP was initiated by the Government Medical Officers’ Association (GMOA) and the Ministry of Health-at the behest of medical graduates-as a means of facilitating their transition to internship. Focus group discussions were held with pre-interns, interns, post-interns, clinicians, professional medical colleges and faculties of medicine. The aim of these discussions was to understand the requirements and devise a suitable and sustainable programme that could be integrated into the existing health system.
The needs assessment consisted of an anonymous self-administered questionnaire. The aims were to identify tasks the participants were least prepared for, the main stressors they encountered and what assistance they would have liked. All post-interns nationally and interns in two provinces (chosen for logistical reasons) were requested by email to complete the survey form.
Subsequent to the needs assessment and the focus group discussion, it was decided that a national multi-modal transitional programme led by the Ministry of Health in collaboration with the GMOA and medical academic colleges would be conducted annually.
The GIP was designed to include;
1. A residential language training program for non-Tamil speaking graduates.
2. A hospital based four-day skills training program to improve acute care skills (ACST).
3. A multimodal 4-day workshop based on the “System building blocks” framework of the WHO [1].
4. A handbook for graduates as a reference manual.
5. A website (www.medicalintern.lk) as a portal to access relevant material.
The objectives, collaborators, format and assessment for each facet are summarised in Table 1.
| Intervention | Objectives | Description | Parties involved | Format | Assessment |
|---|---|---|---|---|---|
| Language course | To enhance Tamil language ability for Doctors, as part of the National language policy to provide equal care to all through improved communication | A 150 hours (10 day) residential programme | Ministry of Languages, Government Medical Officers’ Association (GMOA) |
Interactive group sessions | End of course written and oral assessment* |
| Clinical skills sessions | To increase quality of care by optimizing the knowledge and skills essential for a successful internship | A 4 day session including advanced life support, blood transfusion, breast feeding promotion, IV canulation etc. | Multiple medical academic Colleges, GMOA |
Practical sessions, demonstration, audio-visual presentations |
Pre and post training self-assessment |
| Workshop on GMP related to internship | To inculcate a culture of GMP in the intern in accordance with “System building blocks” framework of WHO | A 4 day workshop on GMP | Ministry of Health (MOH) GMOA |
Symposia, Lecture discussions, Audio-visuals, Demonstrations, Brain storming sessions |
Post workshop feedback |
| Handbook for medical interns | To provide practical knowledge required for internship | A guide to tackle common problems encountered during internship and beyond | GMOA, MOH, Subject experts |
Published handbook | Not assessed |
| Website: www.medicalintern.lk | To provide continuous and up to date information required for a successful internship | A website for medical interns | GMOA | Guidelines Circulars Forums Portal IRS and AIRS Portfolio and CV assistance. | Not assessed |
Table 1: Activities of the Good Intern Program. *Not available for analysis.
The 10-day practical Tamil language-training programme was devised in collaboration with the Ministry of National Languages and Social Integration and delivered to the participants, in small groups, at the National Institute of Language Education and Training (NILET). The language-training programme was developed to improve the young medical professionals’ Tamil language skills during clinical interactions with staff, patients and their relatives.
The 4-day acute care skills training (ACST) program was organised for small groups (up to 6 pre-interns) to train in day-to-day acute care clinical skills, under the supervision of a consultant anaesthetist and physician. The training was held island-wide and the participants maintained logbooks.
The GMP workshop was held over 4 days at a central location in Colombo approximately two weeks prior to the commencement of internship. The sessions were devised in accordance with the principles of GMP. The speakers were eminent academics and professionals who were free to choose the content and manner of their sessions.
The “Handbook for Medical Interns” was developed as a pocket reference; it is intended as a quick source of reliable, relevant and useful information for an intern doctor in Sri Lanka. Special emphasis was given to administrative and medico-legal matters; dealing with emergencies; and avenues to seek help or expert information when needed in the clinical setting, for example contacting the National Poisons Centre when faced with an uncertain overdose.
The medical intern website (www.medicalintern.lk) was a designed to be a complimentary portal. It provides a means of communication and information for interns during their internship and serves as an administrative platform for the GIP.
The evaluations related to GIP consisted of an assessment of the knowledge, (self-perceived) skills and attitudes, of medical graduates awaiting internship, via an online form at the point of registration; a pre and post skills training (self-assessed) measure from those attending the skills training program; and feedback from participants attending the 4-day multi-modal workshop, including a session-by session feedback via an anonymous paper form to provide an overall rating for each session. An examination was conducted at the end of the language course, though the language course results were not accessible for reporting in this paper. The medicalintern.lk website and the handbook for medical interns, which was provided to all the attendees of the 4-day GMP workshop, were not formally evaluated.
The cost of the GIP was borne by the Ministry of Health and Ministry of National Languages and Social Integration with a nominal fee payable by pre-interns for administrative expenses.
Ethical clearance was not sought as this was a standard evaluation of a training programme and all information collected was after verbal consent.
Results
Survey of post-interns and interns-needs assessment
Nine hundred and eighty doctors completed the needs assessment. Of them 740 were post interns and 240 were interns. Amongst both intern and post intern groups, stress was more prevalent during the first half with 264 (35.7%) post-interns and 119 (49.6%) interns finding the first six months of internship to be “too stressful”. The proportion stating that internship was too stressful during the first appointment was significantly higher than those who did so during the second appointment, for both post interns (p=0.003) and interns (p<0.001). It is to be noted that 80 (10.9%) post-interns and 24 (10%) interns admitted to crying either alone or in public during internship. The proportions of doctors crying were significantly higher in the first as opposed to the second appointment and higher amongst females (77.6%) when compared with males. The speciality causing greatest stress during the first appointment for both post interns and interns was obstetrics and gynaecology (30.3% and 36.1% respectively) followed by internal medicine (29.5%, and 26.9% respectively). Among the interns working in obstetric wards, 62% were stressed at the beginning of the internship and the majority (54%) found the labour room to be the most stressful place.
In the post-intern group, the association between a stated desire to leave the state health sector and the stressful first appointment of internship or crying due to a stressful event in the first appointment of internship was statistically significant (p<0.05 and p<0.001). Further, stress during communication was significantly associated with the feeling of internship being too stressful (p<0.0001). 49% of the interns and 31% of the post interns found communicating with consultants during the ward round to be stressful.
Five hundred and seventy two (77.3%) of the post interns and 75.4% (n=181) of the interns felt the need for an external support mechanism, an “internship support centre”. This included 87.1% of the post interns who found internship to be too stressful, and 82.3% of those who did not. Importantly, of the interns working in obstetric units, 91.7% and 95.8% felt that a dedicated period of training or transition prior to the commencement of internship would be of benefit to them and that it would enhance patient management.
Tamil language-training programme
Seven hundred and ninety graduates attended the residential language course. The results of the language course were not accessible for reporting in this paper.
GIP registration assessment
Eight hundred and sixty six graduates registered through medicalintern.lk for the GIP program. A large majority (90.4%, n=783) considered knowledge of medical administrative matters to be important for doctors; nearly half (46.9%, n=406) felt that doctors did not have adequate knowledge regarding administrative affairs while 44.4% (n=385) considered attending to such tasks to be difficult as shown in (Table 2).
| Factor (n=866) | Response | ||||
|---|---|---|---|---|---|
| Strongly agree | Agree | Neutralopinion | Disagree | Strongly disagree | |
| Administrative knowledge is important for doctors | 383 (44.20%) |
400 (46.20%) |
56 (6.50%) |
6 (0.70%) |
21 (2.40%) |
| Attending to administrative matters is difficult | 34 (3.90%) |
351 (40.50%) |
301 (34.80%) |
156 (18.00%) |
24 (2.80%) |
| Doctors should be given inputs on administrative issues | 146 (16.90%) |
534 (61.70%) |
152 (17.60%) |
14 (1.60%) |
20 (2.30%) |
Table 2: Attitudes of pre interns on administrative issues.
Skills training course
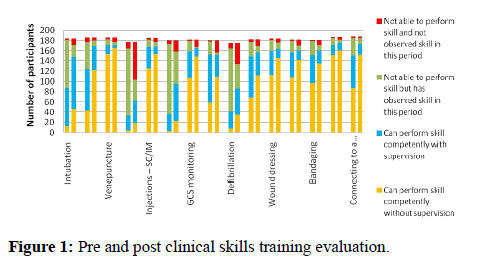
Two hundred and seventy eight graduates attended the hospital based clinical training sessions, which were carried out in 28 hospitals island-wide; 208 of them completed the pre and post skills training assessments. Their self-assessment of skills, pre and post training, and the self-assessment of all interns who registered for the GIP are summarised in (Figure 1). All surveyed skills showed an increase in the proportion of those who could perform the skill competently without supervision after the hospital based skills training program when compared to those before participation.
The main suggestions received from the participants included conducting this training 2-3 months prior to the commencement of internship and increasing the duration of the training sessions to at least 2 weeks. They particularly encouraged inclusion of ETUs, PCUs, Gynaecology and Obstetrics wards, Labour rooms and Paediatric wards in the program. It was advocated that the training should be made mandatory and that the skills training should be delivered in a more intensive manner in fewer training centres.
GMP workshop
Seven hundred and ninety six graduates attended the 4-day Good Medical Practice workshop; 491 of them returned the feedback forms provided. A majority of them were females (55%, n=476) while 191 (22.1%) resided in Colombo.
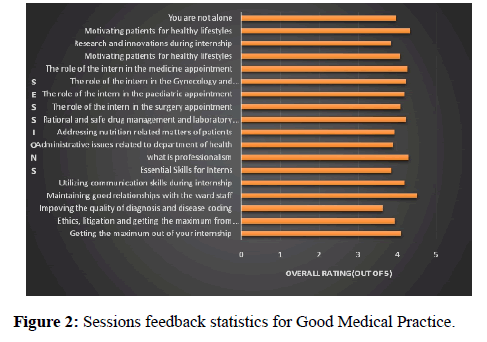
The session on “Essential skills for interns” received the highest positive rating, as perceived by the participants, for relevance while sessions on “Administrative issues related to Department of Health” and “You are not alone” were also particularly well received. Overall, 11 out of the 18 sessions received cumulative ratings of 4 and above. The results are summarised in (Figure 2).
Discussion
This paper details the Good Intern Programme, a sustainable multi-modal programme based on GMP, which aims to facilitate the internship of medical graduates in Sri Lanka.
Good Medical Practice, as described by the General Medical Council, UK [18], sets out universal principles and guidelines that should be adhered to by every practicing doctor in order to maintain high standards of patient care and professionalism. Described in four domains, it requires a doctor to be competent in knowledge, skills and performance; to ensure safety and quality; to develop skills in communication, partnership and teamwork; and to maintain trust with patients and colleagues. These domains are as applicable to interns as they are to all other medical professionals.
Many medical schools have introduced pre-internship time periods into their curricula, and many hospitals encourage safe trainee changeovers that include a period of induction and paid shadowing prior to the year of internship [19,20]. There is evidence that such programs have a positive effect on the pre-interns [5,21-24] and there have been calls for similar efforts in Sri Lanka [9,25].
Due to administrative and logistical reasons, the details of internship posting in Sri Lanka are only available almost one year after graduation. The lack of soft skills, such as teamwork [3,26], communication [9], organisation and time management [10,26,27], which play a large part in the medical professional’s skill set and directly affect patient care, is also of concern.
The needs assessment confirms that internship for Sri Lankan doctors is a stressful undertaking for which they feel underprepared as is common with medical graduates around the world [28]. The lack of communication skills, identified in this study, is especially concerning since it has the potential to extend beyond the internship period affecting both doctor-patient contact and the personal lives of the participants.
The large numbers of graduates participating in the program-with the collaboration of Ministry of Health, the GMOA, academic medical colleges, medical schools, hospitals, language and communication skills trainers-has created an important opportunity to positively influence the knowledge and skills of the medical graduates and ease their transition, thus potentially improving patient care. The largely positive feedback and suggestions for expansion to include further clinical training, suggests that these initiatives are well received, despite the obvious difficulties in catering to such large numbers in a cost-effective and efficient manner.
The strengths and limitations of the GIP are summarised in (Table 3). In summary; the training sessions were of short duration; the four-day workshop was carried out in a single location for a very large group; the pre and post training skills were self-assessed; furthermore as the post skills assessment was carried out immediately after each session the retention of knowledge and skills could not be ascertained. In addition, the opportunity to improve GIP, ensure sustainability and facilitate related measures deserve consideration. The use of the medicalintern.lk internet portal to convey guidelines, communications and informal support needs to be pursued. The initiation of an independent intern support centre for mentoring and support has the support of the interns and provides an opportunity to improve intern wellbeing, and subsequently, their performance. The provision of a more structured skills training program alongside the hospital based model maybe beneficial and may enable a more controlled learning environment and opportunity for objective assessment of the effectiveness of training. Finally, it is likely that “on the job” orientation and mandatory shadowing with a staged handover and a paid supernumerary position with named mentorship would enhance the GIP and can result in a better outcome for graduate doctors and their patients.
| Intervention | Strengths | Limitations |
|---|---|---|
| Tamil language training | Language skills focused to clinical requirements-spoken and listening centred. Residential course Taught by experts |
Inadequate time Assessment and impact not available for evaluation |
| Clinical skills training | Actual clinical settings utilised Small groups Specialist trainers-Physicians and Anaesthetists |
Resource heavy Quality assurance and standardisation No objective assessment Short time period |
| Workshop for reinforcing Good Medical Practice | High overall rating from pre-interns for content and presentation Broad spectrum of topics National experts delivered content-credibility very high Multidisciplinary input Holistic approach Focused not on internship but on lifelong learning. |
Difficulty in accommodating the large number of participants Large number restricts training format to predominantly lectures |
| Handbook for medical interns | Comprehensive Practical, pocket sized manual Written by content experts Informal positive feedback from all stakeholders |
Handbook will need to be updated |
| Website medicalintern.lk | Accessible on demand A continuing portal for up to date information A two way communication channel High uptake of the website with all participants for the GMP workshop registering online through the website |
Access limited by internet facilities |
Table 3: Strengths and limitations of interventions of the Good Intern Programme.
The Good Intern Program, likely to be unique in a LMIC, provides an opportunity to improve the transition of medical graduates in Sri Lanka using a multi-modal and sustainable methodology. Further iterations and expansion of the program are warranted, with assessment of its impact and acceptability needing further research.
Acknowledgement
The authors would like to acknowledge the employees of the Ministry of Health, especially in the DDG (ET&R) office, Government Medical Officers’ Association staff, The academic medical colleges (in particular Colleges of Physicians, Surgeons, Obstetricians and Gynaecologists, Anaesthesiologists,) staff at NILET and Ministry of National Languages and reconciliation, Directors and Consultants of the 28 hospitals island wide who facilitated clinical skills training. The executive committee of the GMOA; Tennakone A.D.T.M.S.S, Kudagama K.M., Herath H.M.N.P., Soysa H.N.D., Dharmarathne C.S., Wijesooriya W.I.N., Mallwarachchi K.P., Lathaharan A., Sainiranjan B. are especially acknowledged.
References
- Brennan N, Corrigan O, Allard J, et al. The transition from medical student to junior doctor: today’s experiences of Tomorrow’s Doctors. Med Educ. 2010;44:449-58.
- World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva: World Health Organization 2010.
- Duchscher JE. Transition shock: the initial stage of role adaptation for newly graduated Registered Nurses. J Adv Nurs. 2009;65:1103-13.
- Paice E, Rutter H, Wetherell M, et al. Stressful incidents, stress and coping strategies in the pre‐registration house officer year. Med Educ. 2002;36:56-65.
- Berridge EJ, Freeth D, Sharpe J, et al. Bridging the gap: supporting the transition from medical student to practicing doctor-a two-week preparation programme after graduation. Med Teach. 2007;29:119-27.
- Wall D, Bolshaw A, Carolan J. From undergraduate medical education to pre-registration house officer year: how prepared are students? Med Teach. 2006;28:435-9.
- Sen S, Kranzler HR, Krystal JH, et al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry. 2010;67:557-65.
- Laack TA, Newman JS, Goyal DG, et al. A 1-week simulated internship course helps prepare medical students for transition to residency. Simul Healthc. 2010;5:127-32.
- Bogg J, Gibbs T, Bundred P. Training, job demands and mental health of pre-registration house officers. Med Educ. 2001;35:590-95.
- Illing J, Morrow G, Kergon C, et al. How prepared are medical graduates to begin practice. A comparison of three diverse UK medical schools. Newcastle: University of Newcastle 2008.
- Gome JJ, Paltridge D, Inder WJ. Review of intern preparedness and education experiences in General Medicine. Intern Med J. 2008;38:249-53.
- Chandraguptha SM. An audit on knowledge of intern house officers on cardio pulmonary resuscitation. Sri Lankan J Anaesth. 2011;19:43-6.
- Sein N, Tumbo J. Determinants of effective medical intern training at a training hospital in North West Province, South Africa. Afr J Health Prof Edu. 2012;4:10-4.
- Phillips DP, Barker GEC. A July Spike in Fatal Medication Errors: A Possible Effect of New Medical Residents. J Gen Intern Med. 2010;25;774-9.
- Young JQ, Ranji SR, Wachter RM, et al. “July effect”: impact of the academic year-end changeover on patient outcomes: a systematic review. Ann Intern Med. 2011;155:309-15.
- Nonis NJ, Herath HMSSD. Sri Lanka Medical Council Annual report 2010. Colombo: Sri Lanka Medical Council 2010.
- Sri Lank a Health Sector Development Project. Measures of Equity, Efficiency and Quality of Selected Healthcare Services. Colombo: Ministry of Healthcare & Nutrition 2008.
- General Medical Council. Good medical practice. London: General Medical Council 2013.
- Leeder SR. Preparing interns for practice in the 21st century. Medi J Aust. 2007;186:6-8.
- Academy of Medical Royal Colleges. Recommendations for safe trainee changeover. London: NHS Employers 2013.
- Dare A, Fancourt N, Robinson E, et al. Training the intern: the value of a pre-intern year in preparing students for practice. Med Teach. 2009;31:345-50.
- Fisher JW, Thompson BM, Garcia AD. Integrative clinical experience: an innovative program to prepare for internship. Teach Learn Med. 2007;19:302-7.
- Australian Medical Association. Position Statement, Core Terms in Internship.
- Brunt LM, Halpin VJ, Klingensmith ME, et al. Accelerated skills preparation and assessment for senior medical students entering surgical internship. J Am Coll Surg. 2008;206:897-904.
- Teo AR, Harleman E, O’Sullivan PS, et al. The key role of a transition course in preparing medical students for internship. Acad Med. 2011;86:860.
- Hannon FB. A national medical education needs’ assessment of interns and the development of an intern education and training programme. Med Educ. 2000;34:275-84.
- Calman KC, Donaldson M. The pre‐registration house officer year: a critical incident study. Med Educ. 1991;25:51-9.
- Abeykoon P, Bandaranayake RC, Jayasena K, et al. An analysis of internship training in Sri Lanka. Med Educ. 1981:15:161-6.