Research Article - Journal of Pregnancy and Neonatal Medicine (2017) Volume 1, Issue 1
Predictors of poor suckling among neonates delivered at 37 weeks and beyond from obstetric perspective: a five-year observational study.
- *Corresponding Author:
- Dawn W Foster
Psychiatry Department at Yale Schol of Medicine Yale University, New Haven, CT 06519, USA
Tel: 203 974 7892
E-mail: dawn.foster@yale.edu
Accepted date: November 15, 2017
Citation: Masood A, Emarh M, Al-Halaby A, et al. Predictors of poor suckling among neonates delivered at 37 weeks and beyond from obstetric perspective: A five-year observational study. J Preg Neonatal Med 2017;1(1):27-30.
DOI: 10.35841/neonatal-medicine.1.1.28-31
Visit for more related articles at Journal of Pregnancy and Neonatal MedicineAbstract
Objective: To assess prospectively the predictors of poor suckling among term neonates delivered at 37 weeks and beyond from obstetric perspective. Methods: This five-year observational study was conducted on 326 term neonates who experienced poor suckling compared to a cohort of 9482 term neonates with normal suckling. Predictors of poor suckling were explored by univariate and multivariate analyses. Data was collected and tabulated. Results: Mothers of neonates with poor suckling have significantly higher rates of medical disorders (p<0.001). Maternal hypertensive disorders (OR 2.52 with 95% CI of 0.96-3.38), elective CS before 39 weeks (OR 1.68 with 95% CI of 0.78-3.44), delivery by CS under general anesthesia (OR 1.86 with 95% CI of 0.76-2.32), PROM >18 hours (OR 2.04 with 95% CI of 0.96-4.28), meconium or blood stained amniotic fluid (OR 1.98 with 95% CI of 0.78-2.39), Induction and/or augmentation of labor (OR 2.42 with 95% CI of 0.98-4.66), gestational age <39 weeks (OR 1.54 with 95% CI of 0.66-1.98) and Prolonged labor >24 hours (OR 1.44 with 95% CI of 0.72-1.96) are predictors of poor suckling among term neonates. Conclusion: Term neonates are not immune against poor suckling which could be attributed to maternal medical disorders, intrapartum complications and mode of delivery. Obstetricians and Pediatricians should be aware of these issues.
Keywords
Poor suckling, Term neonates, NICU admission.
Introduction
Breastfeeding confers short-term and long-term benefits for both the mother and infant. In addition to satisfying the infant’s nutritional needs, it decreases infants’ acute conditions as diarrhea, pneumonia, meningitis and infant’s mortality [1-3].
The sucking pattern of full-term infants is composed of the rhythmic alternation of suction and expression. Two forms of sucking are distinguished: nutritive sucking (NS) and nonnutritive sucking (NNS). The ability to integrate breathing with sucking and swallowing is a prerequisite for coordinated feeding [4,5].
The most reported causes of poor suckling include preterm babies, low birth weight babies, those with neurological disorders or congenital anomalies as well as maternal administration of drugs as lorazepam [6-10].
The aim of this study was to assess the predictors of poor suckling among term neonates delivered at 37 weeks and beyond from obstetric perspective.
Materials and Methods
This was a prospective observational study conducted at the department of Obstetrics and Gynecology in collaboration with the Neonatal intensive care unit (NICU) at the Pediatrics department, Menoufia University hospital, Menoufia governorate, Egypt during the period between the beginning of August 2012 and the end of September 2017.
The study protocol was formally reviewed and approved by the local review board and the ethical committee for human research at Menoufia Faculty of Medicine prior to conducting the study.
Parents of the included neonates with poor suckling signed the informed consent form after thorough explanation of the study objectives.
All neonates who were delivered at the Delivery or Operating room at the department of Obstetrics and Gynecology at term (37 weeks and beyond) during the study period, were examined by trained Neonatologist and neonates diagnosed with poor suckling after careful observation for 1-2 hours who needed admission to NICU were included in the study.
Poor suckling was diagnosed after thorough assessment of the new-born oral cavity via palpation of the soft and hard palate, gingivae, sublingual areas as well as ruling out the ability of the new-born to compress milk ducts via putting gloved finger in baby’s mouth to assess function. Also, Arterial blood gases and blood glucose were measured and found normal immediately after admission to NICU.
Preterm neonates, low birth weight (<2.5 kg) neonates, and neonates with respiratory complications (Respiratory distress syndrome and transient tachypnea of the new-born) as well as those with congenital malformations of any type were excluded from the study.
Mothers with breast abnormalities such as breast enlargement/ reduction surgery, breast hypoplasia, gigantomastia as well as nipple abnormalities were listed also as an exclusion criterion.
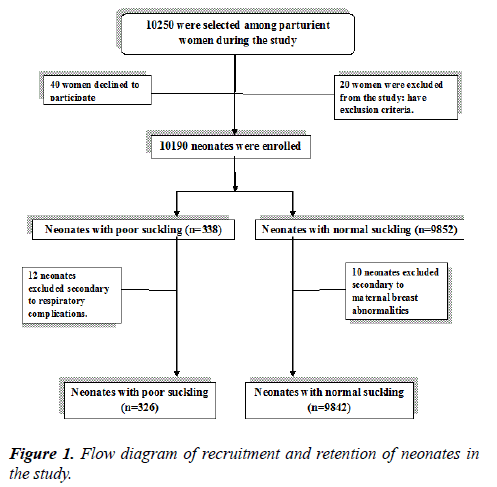
For better interpretation of results, neonates with poor suckling (n=326) was compared to a cohort of term neonates with normal suckling (n=9482) who were delivered during the same period at the same gestational age (Figure 1).
Outcome measures
Assessment of predictors of poor suckling among term neonates from obstetrics perspective.
Statistical analysis
Statistical analysis was performed using Statistical Package for The Social Sciences Version 22 (IBM Corp, Armonk, NY, USA). Quantitative data are expressed as means and standard deviations. Chi-squared test, t-test and Mann Whitney test were used to compare the two groups. P value ≤ 0.05 was considered to indicate significance and p ≤ 0.001 was considered to indicate strong significance. Logistic regression was used to assess the crude association between risk factors and poor suckling. Covariates exhibiting an association with poor suckling (p<0.05) were included when developing univariate and multivariate regression analyses.
Results
All included neonates admitted to NICU with poor suckling did not suffer from hard outcome as need for ventilation or neonatal death and discharged from NICU after 2-4 days in a good health.
Table 1 depicts maternal characteristics. There was no significant difference between both groups regarding age, parity and body mass index (p>0.05). Mothers of neonates with poor suckling have significantly higher rates of medical disorders (p<0.001).
| Term neonates with poor suckling (n=326) | Term neonates with good suckling (n=9, 482) | Student t-test | P-value | |
|---|---|---|---|---|
| Age (years) | 24.9 ± 4.3 | 25.1 ± 3.8 | 0.93 | >0.05 |
| Parity | 1.4 ± 1.2 | 1.3 ± 1.2 | 1.48* | >0.05 |
| Body mass index (Kg/m²) | 23.8 ± 3.2 | 23.6 ± 3.1 | 1.14 | >0.05 |
| Medical disorders: | ||||
| -Hypertensive disorders | 124 | 652 | 415.7 | <0.001 |
| -Diabetes mellitus | 86 | 384 | 339.5 | <0.002 |
| -APS | 42 | 344 | 68.9 | <0.003 |
| -Others | 36 | 266 | 68.9 | <0.004 |
Table 1: Flow time of natural rubber latex in xylene.
Table 2 reveals delivery data. Mothers of neonates with poor suckling exhibit higher rates of delivery by CS, elective CS before 39 weeks, suffered PROM longer than 18 hours, had meconium or blood stained amniotic fluid during labor, underwent induction and/or augmentation of labor, received general anesthesia, had prolonged labors >24 hours and delivered before 39 weeks gestation (p<0.001).
| Term neonates with poor suckling (n=326) | Term neonates with good suckling (n=9, 482) | Chi square test | P-value | |
|---|---|---|---|---|
| Mode of delivery: | ||||
| -Vaginal | 160 | 5984 | 25.9 | <0.001 |
| -Vacuum | 42 | 1204 | 0.001 | >0.05 |
| -Caesarean section | 124 | 2294 | 31.7 | <0.001 |
| Elective CS before 39 weeks | 58 | 586 | 67.4 | <0.001 |
| PROM >18 hours | 68 | 482 | 145.2 | <0.001 |
| Meconium or blood stained amniotic fluid | 42 | 398 | 53.5 | <0.001 |
| Induction and/or augmentation of labor | 56 | 524 | 74.8 | <0.001 |
| Maternal administration of general anesthesia | 44 | 366 | 70.7 | <0.001 |
| Gestational age <39 weeks | 38 | 296 | 67.2 | <0.001 |
| Prolonged labor >24 hours | 28 | 234 | 43.1 | <0.001 |
| Abnormal fetal heart rate tracing | 22 | 660 | 0.001 | >0.05 |
| Apgar scores: | ||||
| -At one minute | 6.35 ± 1.38 | 6.39 ± 1.32 | 0.54 | >0.05 |
| -At five minutes | 8.16 ± 1.22 | 8.20 ± 1.18 | 0.6 | >0.05 |
Table 2: Delivery data.
Table 3 shows predictors of poor suckling among term neonates by univariate and multivariate analyses. Maternal hypertensive disorders (OR 2.52 with 95% CI of 0.96-3.38), elective CS before 39 weeks (OR 1.68 with 95% CI of 0.78-3.44), delivery by CS under general anesthesia (OR 1.86 with 95% CI of 0.76-2.32), PROM >18 hours (OR 2.04 with 95% CI of 0.96-4.28), meconium or blood stained amniotic fluid (OR 1.98 with 95% CI of 0.78-2.39), Induction and/or augmentation of labor (OR 2.42 with 95% CI of 0.98-4.66), gestational age <39 weeks (OR 1.54 with 95% CI of 0.66-1.98) and Prolonged labor >24 hours (OR 1.44 with 95% CI of 0.72-1.96) are predictors of poor suckling among term neonates.
| Risk factor | Crude Odd’s ratio | Upper and lower limit (Confidence interval 95%) |
|---|---|---|
| Maternal hypertensive disorders | 2.52 | 0.96-3.38 |
| Elective CS before 39 weeks | 1.68 | 0.78?3.44 |
| Delivery by CS under general anesthesia | 1.86 | 0.76-2.32 |
| PROM >18 hours | 2.04 | 0.96-4.28 |
| Meconium or blood stained amniotic fluid | 1.98 | 0.78-2.39 |
| Induction and/or augmentation of labor | 2.42 | 0.98-4.66 |
| Gestational age <39 weeks | 1.54 | 0.66-1.98 |
| Prolonged labor >24 hours | 1.44 | 0.72-1.96 |
Table 3: Predictors of poor suckling among term neonates by univariate and multivariate analyses.
Discussion
The current study explored the predictors of poor suckling among term neonates from obstetric perspective.
Maternal hypertensive disorders, elective CS before 39 weeks, delivery by CS under general anesthesia, PROM >18 hours, meconium or blood stained amniotic fluid, Induction and/or augmentation of labor, gestational age <39 weeks and prolonged labor >24 hours were predictors of poor suckling among term neonates.
Emergency CS performed for failure to progress or nonreassuring fetal status was associated with poorer neonatal outcome as reported in recent large retrospective study conducted on 4706 women delivered at term [11].
Caesarean section was the only independent predictor of breastfeeding problems among 400 mothers delivered at term who were assessed for breastfeeding problems before discharge from hospital and at 60 ± 12 hours of discharge, as reported by another prospective cohort [12].
A recent two center retrospective study of 1577 woman who underwent indicated inductions of labor revealed greater NICU admissions among neonates delivered by CS upon failed induction but the specific causes of NICU admissions were not listed [13].
A previous multicenter survey included 207 late preterm (≥ 34 and <37 weeks) and 117 preterm infants (<34 weeks) who were admitted to NICU secondary to breastfeeding problems reported that maternal medical diseases, obstetric complications and mode of delivery were among the most common influencing factors affecting breastfeeding [14].
Previous studies have attributed poor suckling to factors affecting the new-born neurological system as neonatal hypermagnesemia resulted from maternal administration of magnesium sulphate, neonatal hyperbilirubinemia and meconium aspiration syndrome [15-17].
Inability to explore the neonatal laboratory work up and to record their outcome in NICU in details constitutes unintended limitations of this study.
Future research should explore other causes of poor suckling among term neonates.
In conclusion, term neonates are not immune against poor suckling which could be attributed to maternal medical disorders, intrapartum complications and mode of delivery. Obstetricians and Pediatricians should be aware of these issues.
Acknowledgements
The authors would like to acknowledge the contribution of the residents and nursing staff of the delivery ward and NICU of Menoufia University Hospital.
Disclosure Statement
No potential conflict of interest was reported by the authors.
References
- Rajeshwari K, Bang A, Chaturvedi P, et al. Infant and young child feeding guidelines: 2010. Indian Pediatr. 2010;47(12):995-1004.
- Jones G, Steketee RW, Black RE, et al. How many child deaths can we prevent this year? Lancet. 2003;362:65-71.
- Blair A, Cadwell K, Turner-Maffei C, et al. The relationship between positioning, the breastfeeding dynamic, the latching process and pain in breastfeeding mothers with sore nipples. Breastfeed Rev. 2003;11:5-10.
- Palmer MM, Crawley K, Blanco I. The neonatal oral-motor assessment scale: a reliability study. J Perinatol 1993;13(1):28-35.
- Lau C, Kusnierczyk I. Quantitative evaluation of infant?s nonnutritive and nutritive sucking. Dysphagia. 2001;16(1):58-67.
- Lemons PK, Lemons JA. Transition to breast/bottle feedings: the premature infant. J Am Coll Nutr. 2001;2:126-35.
- Banerjea MC, Wirbelauer J, Trusen A, et al. Bilateral hypoxic-ischaemic thalamic lesions in newborns. Z Geburtshilfe Neonatol. 2002;206(6):242-6.
- Whitelaw AG, Cummings AJ, McFadyen IR. Effect of maternal lorazepam on the neonate. Br Med J (Clin Res Ed). 1981;282(6270):1106-8.
- Lefebvre F. Breast-feeding among Mothers of Low Birth Weight Infants. Can Fam Physician. 1990;36:1533-615.
- Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003;92(6):721-7.
- Grace L, Greer RM, Kumar S. Perinatal consequences of a category 1 caesarean section at term. BMJ Open. 2015;5(7):e007248.
- Suresh S, Sharma KK, Saksena M, et al. Predictors of breastfeeding problems in the first postnatal week and its effect on exclusive breastfeeding rate at six months: experience in a tertiary care centre in Northern India. Indian J Public Health. 2014;58(4):270-3.
- Magann EF, Ounpraseuth ST, Miller CD, et al. Maternal and perinatal outcomes of indicated inductions of labor. J Matern Fetal Neonatal Med. 2016;29(14):2240-4.
- Jang GJ, Lee SL, Kim HM. Breast feeding rates and factors influencing breast feeding practice in late preterm infants: comparison with preterm born at less than 34 weeks of gestational age. J Korean Acad Nurs. 2012;42(2):181-9.
- Riaz M, Porat R, Brodsky NL, et al. The effects of maternal magnesium sulfate treatment on newborns: a prospective controlled study. J Perinatol. 1998;18:449-54.
- Bromiker R, Medoff-Cooper B, Flor-Hirsch H, et al. Influence of hyperbilirubinemia on neonatal sucking. Early Hum Dev. 2016;99:53-6.
- Beligere N, Rao R. Neurodevelopmental outcome of infants with meconium aspiration syndrome: report of a study and literature review. J Perinatol. 2008;28(3):S93-S101.