- Biomedical Research (2012) Volume 23, Issue 4
PPAR expression and its association with SOD and NF-?B in rats with obstructive jaundice
Peng Gong1,*, Haibo Xu2, Jianing Zhang3, Zhongyu Wang1
1Department of General Surgery, the First Affiliated Hospital of Dalian Medical University, Dalian 116011, China.
2Department of Emergency Surgery, the Second Affiliated Hospital of Soochow University, Suzhou 215004, China.
3Department of Biochemistry, Dalian Medical University, Dalian 116011, China.
- Corresponding Author:
- Zhongyu Wang
Department of General Surgery The First Affiliated Hospital of Dalian Medical University, Dalian 116011 China.
Accepted date: September 01 2012
Abstract
Peroxisome-proliferator responsive element (PPRE) and nuclear factor-κB (NF-κB) response element have been found in the gene sequence of superoxide dismutase (SOD). This study determines the PPARs and NF-κB expression and SOD activity in damaged livers of rats with obstructive jaundice. Sprague-Dawley rats (n = 120) were randomly assigned into four groups: sham 7 days post-surgery (Sham 7), bile duct ligation (BDL) 7 days post-surgery (BDL 7), sham 19 days post-surgery (Sham 19), BDL 19 days post-surgery (BDL 19). Rats were sacrificed and blood samples and liver tissue were preserved at 7 days and 19 days postsurgery. SOD enzyme activity was detected by a commercially available kit. PPAR mRNA expression was determined by RT-PCR. PPAR protein expression and NF-κB expression and activation were determined by immunohistochemistry. Student’s t-test and Pearson correlation were employed using SPSS statistical software. Total SOD and Cu/Zn-SOD activity was decreased in the BDL groups compared with the sham group (P < 0.01). PPARs mRNA and protein expressions in the BDL groups liver were also reduced compared with the sham group (P < 0.01). Both SOD and Cu/Zn-SOD activity and PPAR expression was significantly decreased between the BDL 7 and BDL 19 groups. PPAR protein expression positively correlated with total SOD activity (P < 0.01), and negatively correlated with NF-κB p65 protein expression in the rats (P < 0.01). PPARs may play a role in liver damage in rats with obstructive jaundice through regulation of SOD and NF-κB gene expression.
Keywords
peroxisome proliferators-activated receptors, PPARs; obstructive jaundice; liver; superoxide dismutase, SOD; nuclear factor-κB, NF-κB
Introduction
Peroxisome proliferator-activated receptors (PPARs), members of the nuclear hormone receptor superfamily [1], have been demonstrated to play multiple roles in cellular signaling. PPAR activation results in adipocyte differentiation and lipid metabolism, improved insulin sensitivity and maintainance of glucose homeostasis, inhibition of pro-inflammatory cytokine production and tumor cell proliferation, and cardiovascular protective effects [2].
There are three main PPAR isoforms, including PPARα, PPARβ/δ and PPARγ [3]. Among these isoforms, PPARα and PPARγ have been the most extensively investigated and found to be the molecular targets of hypolipidemic fibrates and anti-diabetic thiazolidinediones. PPARα is mainly expressed in the liver. Its expression is upregulated by the starvation state, and it helps provide energy through regulating multiple genes involved in fatty acid mobilization, activation and degradation. PPARα- mediated events negatively regulate lipid metabolism. In contrast, PPARγ expression is localized mainly to adipose tissue. Under physiological conditions, PPARγ expression is activated after eating, promoting fat accumulation in adipose tissue.Its target genes include adipocyte fatty acid binding protein (A-FABP, or aP2), phosphoenolpyruvate carboxykinase (PEPCK), lipoprotein lipase (LPL), fatty acid transport protein (FATP), and fatty acid transporters (FAT) [4].
Both PPARα and PPARγ regulate the inflammatory process. PPARα downregulates transcriptional activity of nuclear factor-κB (NF-κB), and decreases the production of pro-inflammatory cytokines, such as tumor necrosis factor- α (TNF-α), interleukin-1 (IL-1), IL-10 and IL-6 [5]. PPARγ also exerts an anti-inflammatory effect; PPARγ ligands inhibit macrophage activation and reduce produc tion of pro-inflammatory cytokines [6]. In addition, PPARγ can inhibit the synthesis of inducible nitric oxide synthase (iNOS) through decreasing the activity of transcription factors, such as activator protein 1 (AP-1), signal transducer and activator of transcription (STATs), and NF-κB [7] Decreased PPAR protein expression and increased TNF-α can also lead to disorders in adipocyte differentiation, proliferation and metabolism.
Our previous study showed that lipid peroxidation was involved in organ damage induced by obstructive jaundice. Synthesis of the antioxidant enzyme, super oxide dismutase (SOD), was significantly decreased while proinflammatory cytokines including TNF-α were significantly increased during obstructive jaundice, showing a negative correlation [8-10]. Furthermore, the peroxisomeproliferator responsive element (PPRE) and NF-κB response element have been found in the promoter region of the superoxide dismutase (SOD) gene [9]. PPARs may act the protective effects against the obstructive jaundiceinduced liver damage by regulating gene transcription. Therefore, we investigated whether PPARs regulate the transcription of SOD and/or NF-κB in liver during the pathogenesis and progression of obstructive jaundice.
Materials and Methods
Animals and treatments
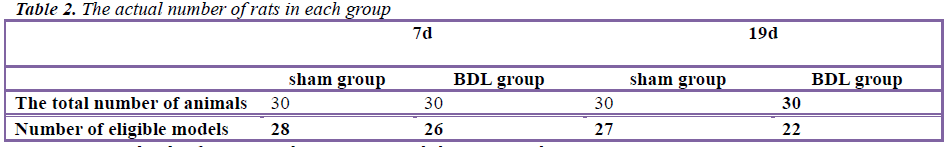
Healthy adult Sprague-Dawley rats (n = 120, 50% female and 50% male, body weight = 200-250 g) were provided by Experimental Animal Center of Dalian Medical University. The animals were bred and maintained in a pathogen- free environment with free access to laboratory chow and sterilized water. The rats were divided into four groups using a simple randomized grouping method (n = 30 for each group): sham operated for 7 days (Sham 7), bile duct ligation (BDL) 7 days post-surgery (BDL 7), sham 19 days post-surgery (Sham 19), and BDL 19 days post-surgery (BDL 19). The obstructive jaundice model in rats was established as previously described [12]. In brief, all the rats were deprived of food and water 4 hours before operation, and then those in the treatment group were anesthetized with ether and restrained. Laparotomy was performed from the middle of the upper abdomen under the xiphoid, exposing the hepatic portal, the hepatic bile duct was isolated, and the common bile duct was double ligated near the liver with #1 line and transected between the two ligatures. Only bile duct separation was performed on the rats in the sham group. Rats were sacrificed and blood samples and livers were collected immediately at 7 days and 19 days post-surgery. Part of the fresh livers were fixed and preserved in formalin for hematoxylin and eosin (HE) staining and immunohistochemistry (IHC), and the rest of the livers were stored at -80°C for molecular analysis.
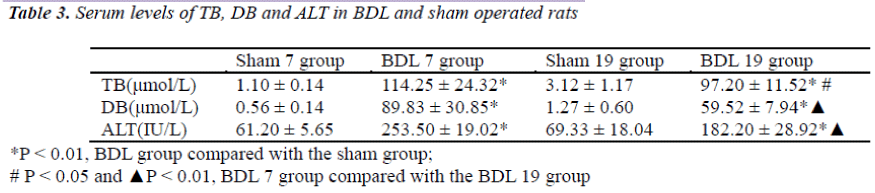
Serum biochemical testing
TB, DB and alanine aminotransferase (ALT) were detected using commercially abailable kits (Zhejiang ELIKAN Biological Technology Co. Ltd, Wenzhou, China) on the Beckman LX-20 automatic biochemical analyzer (Beckman Coulter, Brea, CA).
HE staining of liver tissue
Formalin (10 %) fixed liver tissue was embedded in paraffin, sectioned, stained and then observed using a Nikon E600 optical microscope (Japan) as described previously [13]
IHC staining of liver tissue
Paraffin-embedded sections were deparaffinized, dehydrated, antigen-repaired and then treated following the IHC staining procedures according to the manufacturer’s instructions [14] Primary antibodies used were anti- PPARα (Santa-Cruz Biotechnology Inc. ,California,USA) (1:200), anti-PPARβ (Santa Cruz Biotechnology Inc. ,California, USA) (1:150), anti-PPARγ (Santa Cruz Biotechnology Inc. ,California, USA) (1:200) and anti-NF-κB p65 (1:200).All IHC slides were photographed using an Olympus microscope camera system (400x) (Japan), and then analyzed using Image-Pro Plus image analysis system purchased from Media Cybernetics Inc.(USA) after calibration of the standard intensity. The average optical density of positive expression was calculated by dividing integrated optical density (IOD) by area of interest (AOI).
Liver homogenization and determining SOD activity
After rinsing in ice-cold saline, fresh liver tissues were dried, weighed (0.25 g), cut into pieces and then homogenized using 2.25 g ice-cold saline by manual control. The homogenates were centrifuged at 3000 x g for 15 minutes, and supernatants were diluted with distilled water (1:9), yielding a panel of liver tissue homogenates at a concentration of 1 %. SOD was determined by the colorimetric method (Nanjing Jiancheng Bioengineering Institute Nanjing, China) following the manufacturer’s instructions [15].
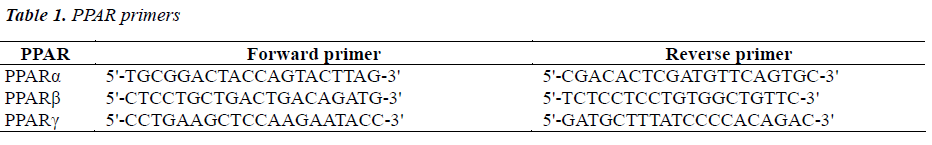
PPAR detection in liver by RT-PCR
Liver samples (100 mg per sample) were quickly frozen in liquid nitrogen and then homogenized. Total RNA was extracted using RNAiso Reagent (AMV) Ver 3.0 (Takara Biotechnology Co. Ltd., Dalian, China) and reverse transcription was performed using the RNA PCR Kit (AMV) Ver 3.0 (Takara Biotechnology Co. Ltd., Dalian, China) following the manufacturer’s instructions [16]. PPAR primers used in the PCR reaction are listed in Table 1. Taq DNA Polymerase were purchased from Takara Biotechnology Co. Ltd. (Dalian, China).PCR conditions were as follows: 95°C for 5 min, 1 cycle; 95°C for 30 s, 60°C for 45 s, and 72°C for 60 s, 40 cycles; 72°C for 10 min, 1 cycle. β-actin expression was used as an internal reference. PCR amplification product (8 μl) was resolved by 3 % agarose gel electrophoresis and visualized by ethidium bromide staining. Quantification of the electrophoretic bands was determined using Bandscan 4.50 software (Glyco Band-Scan software, version 4.50) and normalized to β-actin for each sample.
Statistical analysis
All data are expressed as mean ± standard deviation. Student’s t-test and Pearson correlation were performed using SPSS 13.0 statistical software (SPSS Inc.) between groups. Figures were prepared using SigmaPlot v9.0 software (SYSTAT Inc., California, USA). A p-value of <0.05 was considered statistically significant.
Results
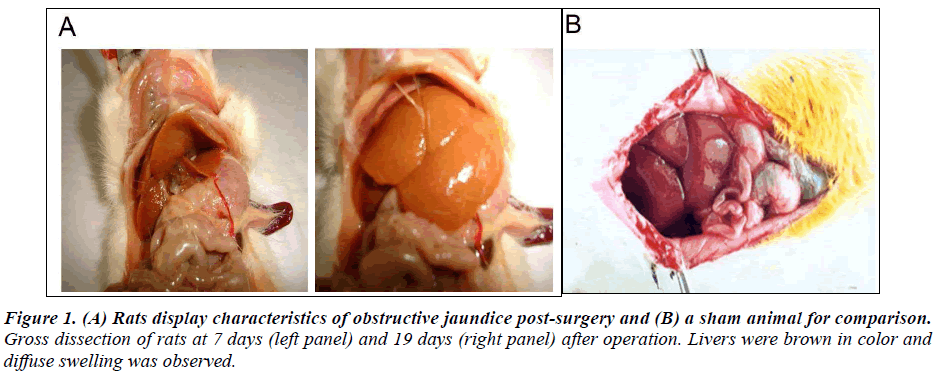
Post-surgery rats demonstrate characteristics of obstructive jaundice
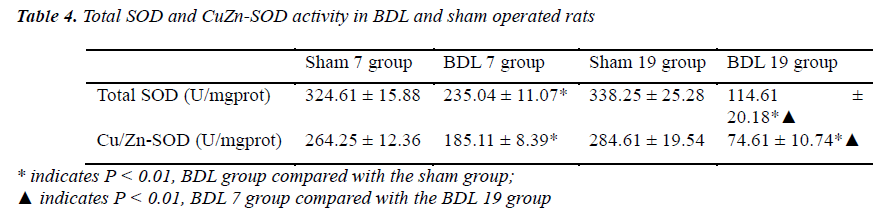
In order to induce obstructive jaundice in a rat model, hepatic ligation surgery was performed. Cystic dilation of the common bile duct associated with the liver and accumulation of bile in this area was observed at 7 days and 19 days post-surgery. Livers were brown in color and diffuse swelling was found in obstructive jaundice rats (Figure 1). In the BDL 7 group, intrahepatic biliary dilatation, hepatocyte swelling, vacuolar degeneration, and focal necrosis were found upon pathological examination of tissue sections (data not shown). Furthermore, fibrous tissue and new bile duct hyperplasia were also found in the portal area (data not shown). In the BDL 19 group, a wide range of hepatocyte degeneration, necrosis, inflammatory cell infiltration, and lobular morphology disorder were observed around the portal area. The rats that did not meet the characteristics of obstructive jaundice in gross observation, biochemical testing and pathological examination were excluded from this study (Table 2). Furthermore, serum levels of total bilirubin (TB), direct bilirubin (DB) and alanine aminotransferase (ALT) in the BDL 7 and BDL 19 groups were significantly higher than the sham group (P < 0.01, Table 3), indicating defective liver function. In addition, total liver super oxide dismutase (SOD) and Cu/Zn-SOD activity was significantly reduced in both the BDL 7 and the BDL 19 groups compared with the sham group (P < 0.01, Table 4). Total liver SOD and Cu/Zn-SOD activity decreased with time after surgery (P < 0.01, Table 4, compare 7 days versus 19 days postsurgery).
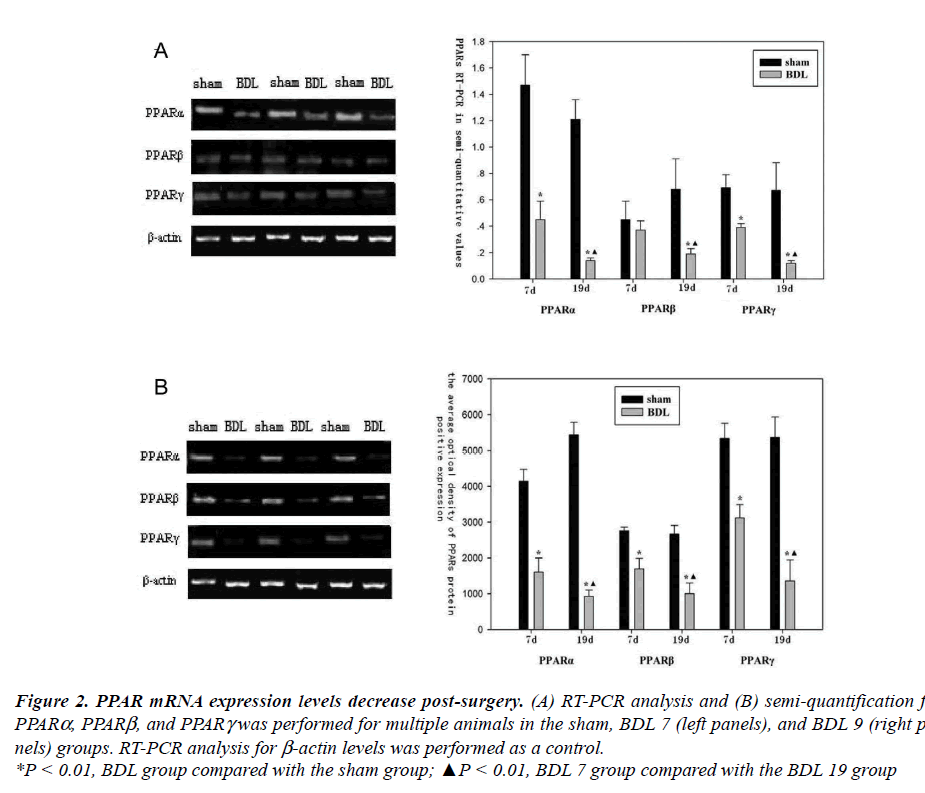
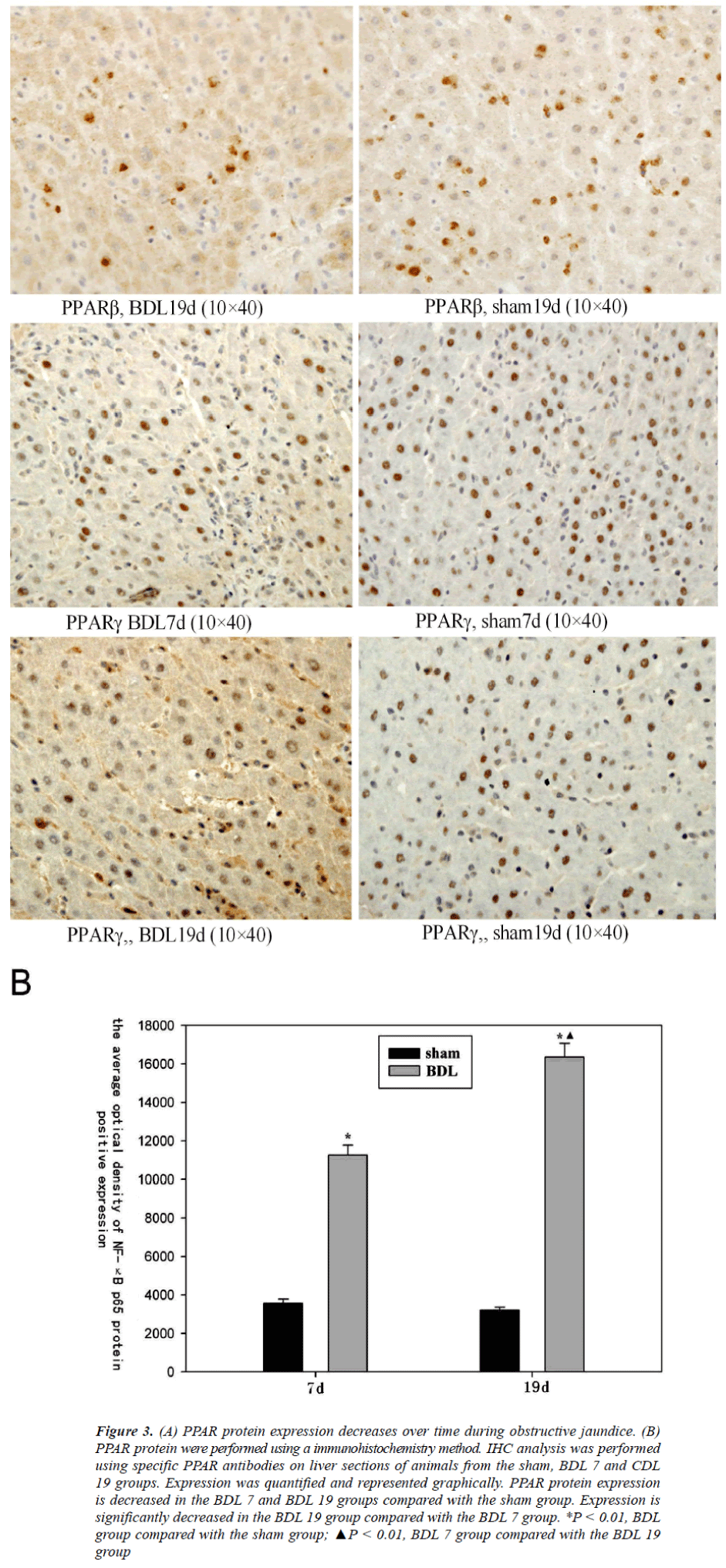
PPAR mRNA and protein expression is downregulated over time post-surgery
In order to determine whether modulation of PPAR mRNA expression occurs during obstructive jaundice RTPCR analysis was performed. PPARα and PPARγ expression was significantly lower than the sham group in both the BDL 7 and the BDL 19 groups (P < 0.01, Figure 2). However, PPARβ mRNA expression was reduced in only the BDL 19 group. In addition, there was a significant reduction in PPAR mRNA expression in the BDL 19 group compared with the BDL 7 group (P < 0.01, Figure 2). Additionally, PPARα, PPARβ and PPARγ protein expression was examined by IHC analysis. All PPARs examined were significantly lower in both the BDL 7 and the BDL 19 groups, compared with the sham group (P < 0.01, Figure 3). In addition, PPAR protein expression in the BDL 19 group was significantly lower than those in the BDL 7 group (P < 0.01, Figure 3).
Figure 2. PPAR mRNA expression levels decrease post-surgery. (A) RT-PCR analysis and (B) semi-quantification for PPARa, PPARb, and PPARg was performed for multiple animals in the sham, BDL 7 (left panels), and BDL 9 (right panels)
groups. RT-PCR analysis for b-actin levels was performed as a control.
*P < 0.01, BDL group compared with the sham group; ▲P < 0.01, BDL 7 group compared with the BDL 19 group PPAR, SOD and NF-κB in obstructive jaundice rats
Figure 3. (A) PPAR protein expression decreases over time during obstructive jaundice. (B) PPAR protein were performed using a immunohistochemistry method. IHC analysis was performed using specific PPAR antibodies on liver sections of animals from the sham, BDL 7 and CDL 19 groups. Expression was quantified and represented graphically. PPAR protein expression is decreased in the BDL 7 and BDL 19 groups compared with the sham group. Expression is significantly decreased in the BDL 19 group compared with the BDL 7 group. *P < 0.01, BDL group compared with the sham group; ▲P < 0.01, BDL 7 group compared with the BDL 19 group
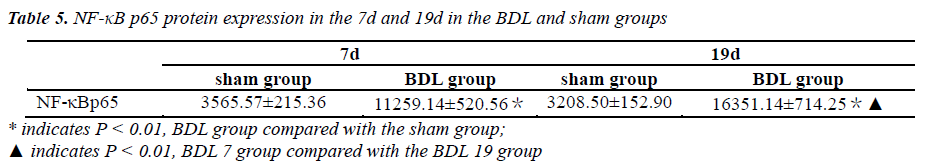
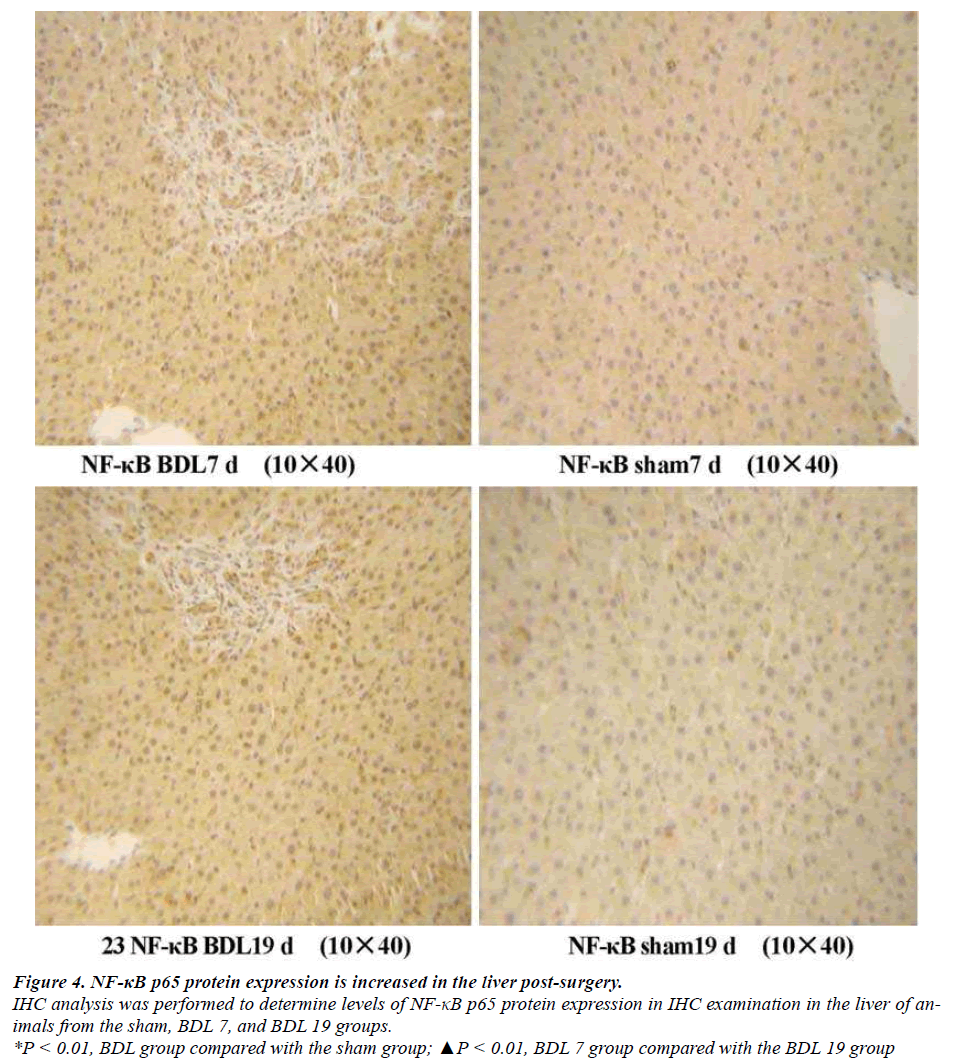
NF-κB p65 expression is increased post-surgery(Table 5) As a NF-κB response element is found within the promoter region of SOD we examined whether NF-κB p65 protein levels are regulated post-surgery by IHC analysis. NF-κB p65 protein expression was not observed or weakly positive in liver tissue of the sham group animals. Enhanced cytoplasmic staining (brown) and visible nuclear staining were seen in the BDL 7 group, and the average optical density of positive expression was higher than that of the sham group (P < 0.01, Figure 4). Moreover, the amount of positive staining per cell and the average number of positive cells was significantly increased in the liver of BDL 19 group animals compared to animals from the BDL 7 group (P < 0.01, Figure 4).
Figure 4. NF-κB p65 protein expression is increased in the liver post-surgery.
IHC analysis was performed to determine levels of NF-κB p65 protein expression in IHC examination in the liver of animals
from the sham, BDL 7, and BDL 19 groups.
*P < 0.01, BDL group compared with the sham group; ▲P < 0.01, BDL 7 group compared with the BDL 19 group
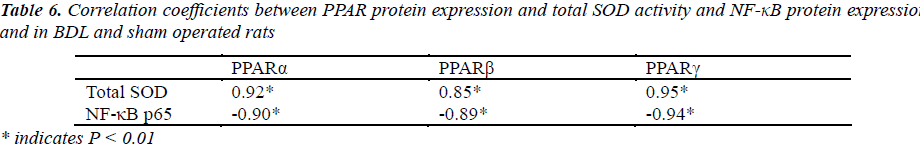
Correlation between total SOD activity, and NF-κB p65 protein and PPAR protein expression
PPARα, PPARβ and PPARγ protein expression in IHC examination positively correlates with total SOD activity (P < 0.01, Table 6) and negatively correlates with NF-κB p65 protein expression in the rats (P < 0.01, Table 6).
Discussion
The results presented here show that total SOD and Cu/Zn-SOD activity were decreased significantly in the liver of rats with obstructive jaundice, decreasing the total anti-oxidant capacity and leading to lipid peroxidationinduced damage of the liver. Thus, if the upstream regulatory factors for SOD can be found, it may provide new insight for correcting the imbalance between free radical generation and scavenging in obstructive jaundice in order to protect organ function. Toyoma et al. found that PPARα ligand agonist, Wy-14643, and fenofibrate were able to reduce peroxide damage by antagonizing catalase inhibition in liver damage [18]. Moreover, a PPRE sequence has been identified upstream of the rat Cu/Zn- SOD promoter, and PPARα and PPARγ agonists significantly increase the expression of Cu/Zn-SOD, thereby enhancing oxygen free radical scavenging [19]. Therefore, PPARs may play a role in protection against obstructive jaundice via regulation of SOD expression. Furthermore, IHC examination determined that NF-κB expression in both the BDL 7 and BDL 19 groups was significantly increased. The BDL 19 group showed even significantly increased expression and more pronounced nuclear translocation, suggesting that a large number of reactive oxygen species (ROS) accumulated in the rats with obstructive jaundice thereby inducing the expression and translocation of NF-κB. Activated NF-κB may subsequently promote liver damage via upregulation of a variety of pro-inflammatory factors, such as TNF-α, IL-1 and IL-6 [20-22].
The main physiological role of PPARs is to transform various environmental, nutritional or inflammatory stimuli into intracellular signals that regulate lipid metabolism, cell proliferation and differentiation [1,23]. A number of natural and synthetic PPAR ligands, including fatty acid and its derivatives, have been found in the past years, which has opened up new prospects for understanding the role of PPARs in the control of energy metabolism and inflammation [21]. The current study presented here shows that liver function is significantly impaired and the mRNA and protein expression of PPARs in the liver are reduced in obstructive jaundice rats. These data indicate that PPARs may play a fundamental role in the attenuation of liver damage in obstructive jaundice. The reason for low expression of PPARs in the livers of rats with obstructive jaundice may be the result of lipid peroxidation through ROS accumulation and reduction of PPAR ligands, such as unsaturated fatty acids.
Notably, we found that PPAR protein expression positively correlated with total SOD activity and negatively correlated with activation of NF-κB p65 protein expression in obstructive jaundice rats. PPARs have been shown to bind to a gene regulatory sequence (PPRE) which is present upstream of the SOD promoter. Therefore, reduction in PPAR expression would decrease SOD protein expression and enzyme activity, weakening the body's resistance to oxidative damage and exacerbating lipid peroxidation in the liver. Furthermore, decreased expression of PPARs may weaken the negative regulatory role of NF-κB. Subsequently, NF-κB activation will induce downstream pro-inflammatory cytokine expression, increasing lipid peroxidation and inflammation, leading to liver damage. However, more experiments are required to validate the proposed molecular regulation mechanisms.
In conclusion, PPARs may play a role in liver damage in rats with obstructive jaundice through regulation of SOD and NF-κB gene expression.
References
- Issemann I, Green S. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature 1990; 347: 645-650.
- Staels B, Fruchart JC. Therapeutic Roles of Peroxisome Proliferator–Activated Receptor Agonists. Diabetes 2005; 54: 2460-2470.
- Berger J, Moller DE. The mechanisms of action of PPARs. Annu Rev Med 2002; 53: 409-435
- Ricote M, Li AC, Willson TM, et a1. The peroxisome proliferator-activated receptor-gamma is a negative regulator of macrophage activation. Nature 1998; 391: 79-82.
- Moraes LA, Piqueras L, Ishop-Bailey D. Peroxisome proliferator-activated receptors and inflammation. Pharmacol Ther 2006; 110: 371-385.
- David Bishop-Bailey, Jonas Bystrom.Emergingroles of peroxisome proliferator-activated receptor-β/δ in inflammation. Pharmacology & Therapeutics 2009; 2: 141-150.
- Rodríguez-Calvo R, Serrano L, Coll T, et a1. Activation of peroxisome proliferator-activated receptor beta/delta inhibits lipopolysaccharide-induced cytokine production in adipocytes by lowering nuclear factor-kappaB activity via extracellular signal-related kinase 1/2. Diabetes 2008; 57: 2149−2157.
- Gong P, Wang Z, Zhao Z, et a1. Expression of TNF-α and Superoxide Dismutase mRNA in Myocardium of Rats with Obstructive Jaundice. Chinese Journal of Bases and Clinics in General Surgery 2004; 11: 502- 504.
- Gong P, Wang Z, Wang H, et a1. Protective effects on toxicity of bile by SOD gene transfection hepatocytes of rat. Chinese Journal of Practical Surgery 2003; 22: 346-347.
- Gong P, Wang Z, Wang H, Chen H, Guan F. Effect and Significance of Astragalus Membranaceus(AM) on Expression of TNFα and SOD Gene mRNA in Injury of Rat Myocardium with Obstructive Jaundice. Chinese Journal of Surgery of Integrated Traditional and Western Medicine 2003; 9: 165-170.
- Gong P, Wang ZY, Wang HJ. Protective effects of pLNCX-SOD gene transfection on hepatocyte injury induced by obstructive jaundice in rats. Hepatobiliary Pancreat Dis Int 2007; 6: 194-198.
- Musa Dirlik, Aydin Karahan, Hakan Canbaz. Effects of sulfasalazine on lipid peroxidation and histologic liver damage in a rat model of obstructive jaundice and obstructive jaundice with lipopolysaccharide-induced sepsis. Current Therapeutic Research 2009; 70: 299- 315.
- Wang P, Guan YF, Du H, et al. Induction of autophagy contributes to the neuroprotection of NAMPT in cerebral ischemic stroke. Autophagy 2011;Epub.
- Wang P, Xu TY, Guan YF, et al. Nicotinamide phosphoribosyltransferase protects against ischemic stroke through SIRT1-dependent adenosine monophosphate- activated kinase pathway. Ann Neurol 2011; 2: 360-374.
- Wang P, Yang FJ, Du H, et al. Involvement of leptin receptor long isoform (LepRb)-STAT3 signaling pathway in brain fat mass- and obesity-associated (FTO) downregulation during energy restriction. Mol Med 2011; 5-6: 523-532.
- Göttle P, Kremer D, Jander S, et al. Activation of CXCR7 receptor promotes oligodendroglial cell maturation. Ann Neurol 2010; 68: 915-924.
- Caglikulekci M, Dirlik M, Pata C, et al. Effect of Nacetylcysteine on blood and tissue lipid peroxidation in lipopolysaccharide-induced obstructive jaundice. J Invest Surg 2006; 19:175-184.
- Toyama T, Nakamura H, Harano Y, et a1. PPARalpha ligands activate antioxidant enzymes and suppress hepatic fibrosis in rats. Biochem Biophys Res Commun 2004; 324: 697-704.
- Inoue I, Goto S, Matsunaga T, Nakajima T, et a1. The ligands/activators for peroxisome proliferator-activated receptor alpha (PPARalpha) and PPARgamma increase Cu2+,Zn2+-superoxide dismutase and decrease p22phox message expressions in primary endothelial cells. Metabolism 2001; 50: 3-11.
- Schoemaker MH, Gommans WM, Conde de la Rosa L, et a1. Resistance of rat hepatocytes against bile acidinduced apoptosis in cholestatic liver injury is due to nuclear factor-kappa B activation. J Hepatol 2003; 39: 153-161.
- Wullaert A, Heyninck K, Beyaert R. Mechanisms of crosstalk between TNF-induced NF-kappaB and JNK activation in hepatocytes. Biochem Pharmacol 2006; 72: 1090-1101.
- Bonofiglio D, Aquila S, Catalano S, et a1. Peroxisome proliferator-activated receptor-gamma activates p53 gene promoter binding to the nuclear factor-kappaB sequence in human MCF7 breast cancer cells. Mol Endocrinol 2006; 20: 3083-3092.
- Lee SS, Pineau T, Drago J, et a1. Targeted disruption of the alpha isoform of the peroxisome proliferatoractivated receptor gene in mice results in abolishment of the pleiotropic effects of peroxisome proliferators. Mol Cell Biol 1995; 15: 3012-3022.
- Staels B, Fruchart JC. Therapeutic roles of peroxisome proliferator-activated receptor agonists. Diabetes 2005; 54: 2460-2470.