Research Article - Journal of Pain Management and Therapy (2019) Volume 3, Issue 1
Postural torsion syndrome algorithm (PTSA) as a method to quantify musculoskeletal health and predict injury.
Armia Abdo*, Vikas Sharma
AZA Health & Wellness LLC, California, USA
- *Corresponding Author:
- Dr Armia Abdo
AZA Health & Wellness LLC
California, USA
E-mail: contact@azahw.com
Accepted Date: April 18, 2019
Citation: Postural torsion syndrome, Postural torsion syndrome algorithm, Predictor of musculoskeletal health, Gravitational biology, Physical therapy assessment, Injury prevention, Physical therapy, Predictor of health.
Abstract
Introduction: In Physical Therapy, developing proper preventive healthcare will require screening tools effective in identifying predictors of pain and injury. Postural Torsion Syndrome Algorithm (PTSA) is a musculoskeletal screening tool that uses a 5-point system measuring a specific angle of hypomobility in twenty key articulations on each side of the body. This measurable dysfunction can be used to predict injury and serve as a treatment guide justifying preventative care. Objective: The goal of this research was to determine PTSA ability to assess and quantify musculoskeletal health and potential of injury. Method: The subjects reported medical history, number of pathologies, severity of pain, and comorbidities. They were then assessed using PTSA. Severity of pain was graded as: 1 – Mild pain; 2 – Moderate; 3 – Severe. PTSA score of 70%, 65%, and 60% were used to find out the cut-off values and thus, the study subjects were divided into 2 groups, i.e., ≥ 70% and < 70%, ≥ 65% and < 65%, and ≥ 60% and < 60%, respectively. Receiver Operating Characteristic (ROC) curve was used to find out the cut-off values of PTSA score, and thus, an appropriate sensitivity and specificity. Conclusion: The present study reported inverse correlation between PTSA score for participants, number of pathologies, severity of pain, and comorbidities. In addition, sensitivity and specificity was found to be 100%. Future studies should be performed with larger number of subjects to prove PTSA assessment effectiveness in quantifying musculoskeletal health and potential of injury.
Keywords
Morphofunctional zones, 6 cambial cells, Scr and Rho proteins, Cancer, Aging
Introduction
Currently in the United States healthcare model, treatment occurs after the patient becomes symptomatic. Waiting until we recognize the problem by patient complaints limits our capacity for quality physical and mental health. With this model, the US spends more on healthcare per capita than every other nation.
In Physical Therapy, developing proper preventive healthcare will require screening tools effective in identifying predictors of pain and injury. Our current tools render themselves ineffective, because they only measure function, which is too variable for accurate assessment [1]. Nevertheless, these inadequate tools are the standard practice for determining a need for skilled interventions and insurance coverage.
Musculoskeletal health depends upon the body’s ability to support itself under gravity by way of efficient form. The loss of this efficiency results in a predictable collapse due to constant gravitational force, creating the foundation for Postural Torsion Syndrome Algorithm (PTSA). Gravitational biology dictates, “As a consequence, all biological processes are accustomed to the ever-present force of gravity and even small variations in this force can have significant impact on the health and function of organisms” [2,3]. These disease processes that result from a failure in our Musculo-Skeletal System (MSS) are not limited to the MSS but will result in a myriad of pathologies affecting all other systems [4].
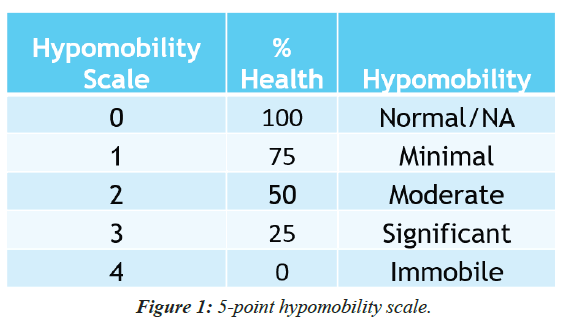
PTSA is a musculoskeletal screening tool that uses a 5-point system measuring a specific angle of hypomobility in twenty key articulations on each side of the body (Figure 1).
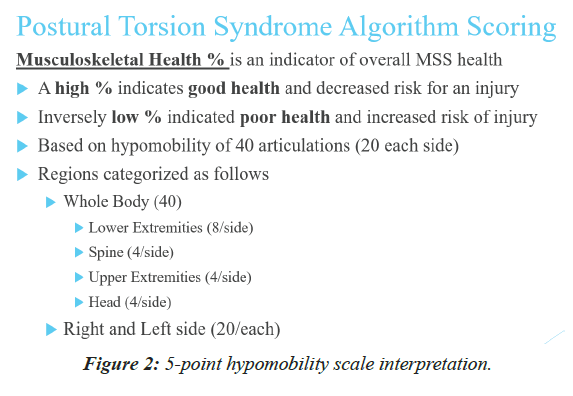
These articulations are susceptible to gravitational forces and can collapse when gravities forces exceed their thresholds for sustaining structural integrity [5]. As a result, these articulations are key drivers of posture and movement. Limitations can be measured in a way that reflects the group dysfunction of that region. This measurable dysfunction can be used to predict injury and serve as a treatment guide justifying preventative care (Figure 2) [6].
Methodology
Design
Quantitative study.
Participants
This study recruited participants associated with AZA Health & Wellness LLC.
Inclusion criteria
Participants between the ages of 34 to 73 with education appropriate to complete questionnaires.
Exclusion criteria
Participants who were unable to complete questionnaires were excluded.
Outcome measures
Participants complete information general health questionnaire listing medical history, body chart identifying symptomatic regions using pain scale 0-10, and assessed using PTSA.
Procedure
The pilot study was completed at AZA Health & Wellness office in California, USA in February 2019. Participants completed questionnaire, body chart, and physical therapy functional outcome tools then submitted information to a 3rd party to prevent bias from Dr. Armia Abdo, DPT performing PTSA assessment. PTSA assessment was gathered and entered in an excel spreadsheet.
PTSA assessment was performed in supine for each posture driver by stabilizing the proximal segment was placed into a neutral position or close as possible and then stabilized. Distal segment was then into a down and in direction (flexion, adduction, and internal rotation) with amount of assistance graded using hypomobility scale (Table 1). Exceptions were noted for first 3 articulations of the foot given their orientation to midline; using flexion, abduction, and internal rotation. See 1.A for posture drivers assessed. Assessment was performed in order presented in graph.
| SUBJECT # |
HEAD PATHOLOGIES | HEAD SCORE PTSA |
SPINE PATHOLOGIES | SPINE SCORE PTSA |
LEG PATHOLOGIES | LEG SCORE PTSA |
ARM PATHOLOGIES | ARM SCORE PTSA |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 INTERMITTENT MODERATE PAIN |
58.00% | 1 INTERMITTENT MODERATE-SEVERE |
73.00% | 2 MODERATE PAIN | 71.00% | 75.00% | |
| 3 | 4 MINIMAL PAIN |
55.00% | 9 MINIMAL- MODERATE PAIN |
45.00% | 4 MINIMAL- MODERATE PAIN |
56.00% | 4 MINIMAL PAIN |
68.00% |
| 4 | 3 MINIMAL- MODERATE PAIN |
55.00% | 3 | 65.00% | 3 MINIMAL | 68.00% | 3 | 68.00% |
| MINIMAL PAIN | MINIMAL PAIN | |||||||
| 5 | 3 MINIMAL PAIN | 60.00% | 2 MINIMAL PAIN | 70.00% | 3 INTERMITTENT MINIMAL- MODERATE PAIN |
74.00% | 2 MINIMAL PAIN | 68.00% |
| 6 | 2 MINIMAL PAIN |
65.00% | 1 MINIMAL PAIN |
70.00% | 10 MINIMAL PAIN |
60.00% | 3 MINIMAL PAIN |
55.00% |
| 7 | 1 INTERMITTENT MODERATE PAIN |
70.00% | 65.00% | 3 MODERATE PAIN | 61.00% | 90.00% | ||
| 8 | 2 MINIMAL PAIN |
65.00% | 2 MINIMAL PAIN |
63.00% | 65.00% | 1 MINIMAL PAIN |
68.00% | |
| 9 | 1 MINIMAL PAIN |
60.00% | 3 MINIMAL- MODERATE PAIN |
53.00% | 2 MINIMAL- MODERATE PAIN |
58.00% | 70.00% | |
| LEGEND | MEANING | |||||||
| <70% PTSA SCORE | ||||||||
| OTHER SYSTEM DYSFUNCTION INVOLVED | ||||||||
Table 1. Summary of subjects with their PTSA scores, pathologies, pain severity, and comorbidities.
1.A Posture drivers
Lower extremity (8/side):
• 1st MTP
• Naviculocuneiform
• Talocalcaneal
• Talocrural
• Distal Tibiofibular
• Proximal Tibiofibular
• Tibiofemoral
• Patellofemoral
Spine (4/side):
• Anterior Superior Iliac Spine on femur
• R7 costosternal
• R2 costosternal
• Sternoclavicular
Upper extremity (4/side):
• 1st MCP
• Distal radioulnar/scaphoid
• Proximal Radioulnar/humeral
• Glenohumeral
Head (4/side):
• C7 on T1
• C1 on C2
• Temporomandibular
• Pterion
Excel spread was sent for data analysis. Subjective information was consolidated into an excel spread sheet and sent for analysis.
After data analysis, correlation was examined between PTSA scores, pain severity, number of pathologies, and co morbidities. Sensitivity and specificity were also determined for PTSA scores for various cut off values.
Data Analysis
The subjects were enquired about the number of pathologies, severity of pain, and comorbidities. They were then subjected to the standard questionnaires and final PTSA scores of Head, Arms, Spine, and Legs were calculated. For statistical analysis, the higher grade of pain was considered, i.e., whenever the pain was graded as minimal to moderate and moderate to severe, it was considered as moderate and severe, respectively. Similarly, severity of pain was graded as: 1-Mild pain; 2-Moderate; 3-Severe. PTSA score of 70%, 65% and 60% were used to find out the cut-off values and thus, the study subjects were divided into 2 groups, i.e., ≥ 70% and <70%, ≥ 65% and <65%, and ≥ 60% and <60%, respectively. ROC curve was used to find out the cut-off values of PTSA score, and thus, an appropriate sensitivity and specificity.
Results
The subjects were enquired about the number of pathologies, severity of pain, and comorbidities. They were then subjected to the standard questionnaires and final PTSA scores of Head, Arms, Spine, and Legs were calculated. For statistical analysis, the higher grade of pain was considered, i.e., whenever the pain was graded as minimal to moderate and moderate to severe, it was considered as moderate and severe, respectively. Similarly, severity of pain was graded as: 1-Mild pain; 2-Moderate; 3-Severe. PTSA score of 70%, 65%, and 60% were used to find out the cut-off values and thus, the study subjects were divided into 2 groups, i.e., ≥ 70% and <70%, ≥ 65% and <65%, and ≥ 60% and <60% respectively. ROC curve was used to find out the cut-off values of PTSA score, and thus, an appropriate sensitivity and specificity
The present pilot study involved 9 subjects, of which 8 completed the questionnaire and their data is presented in following tables. Subjects with their PTSA scores, pathologies, pain severity, and comorbidities are summarized in Table 2.
| Demographic parameters | N = 8 |
|---|---|
| Age (Mean ± SD) (Years) | 53 ± 16.46 |
| Gender ratio (Male:Female) | 1:1 |
Table 2: Demographic profile of the study subjects.
Mean age of the study subjects was 53 ± 16.46 years, and age ranged from 34 to 73 years. Men and women were equally distributed (1:1) (Table 3).
| Characteristics | Head | Spine | Legs | Arms |
|---|---|---|---|---|
| Number of pathologies (Mean ± SD) | 2.13 ± 1.13 | 2.63 ± 2.77 | 3.38 ± 2.92 | 1.63 ± 1.59 |
| Severity of pain (Median) | 1 | 1 | 2 | 1 |
| Number of subjects with comorbidities | 6/8 (75%) | 4/8 (50%) | 3/8 (37.5%) | 2/8 (25%) |
Table 3: Clinical characteristics of the study subjects.
Maximum number of pathologies (3.38 ± 2.92) and maximum severity of pain (median=2) were observed in legs (Table 4).
| Total no. of subjects with painful symptoms | PTSA Scores | Severity of pain | p-value |
|---|---|---|---|
| 8/8 | Head Score | - 0.115* | 0.787 |
| 7/8 | Spine Score | - 0.058* | 0.891 |
| 7/8 | Leg Score | - 0.069* | 0.872 |
| 5/8 | Arm Score | - 0.900* | 0.002 |
| * - Spearman’s correlation coefficient; p-value < 0.05 was considered as statistically significant. | |||
Table 4: Correlation between various PTSA score and severity of pain.
PTSA scores were correlated with the severity of pain and it was observed that the PTSA scores were inversely correlated to the severity of pain i.e., as severity of pain decreases, PTSA score increases (Table 5). However, none of the PTSA scores were significantly correlated to severity of pain, except Arm PTSA score (p-value=0.002).
| Total no. of subjects with pathologies | PTSA Scores | No. of pathologies | p-value |
|---|---|---|---|
| 8/8 | Head Score | - 0.575# | 0.136 |
| 7/8 | Spine Score | - 0.693* | 0.057 |
| 7/8 | Leg Score | - 0.331* | 0.423 |
| 5/8 | Arm Score | - 0.817* | 0.013 |
| # - Pearson’s correlation coefficient; * - Spearman’s correlation coefficient; p-value < 0.05 was considered as statistically significant. | |||
Table 5: Correlation between various PTSA score and number of pathologies.
Similarly, various PTSA scores were correlated with the number of pathologies and it was observed that PTSA scores were inversely correlated to the number of pathologies (Table 6). However, none of the PTSA scores were significantly correlated to number of pathologies, except Arm PTSA score (p-value=0.013).
| Total no. of subjects with comorbidities | PTSA Scores | Comorbidities | p-value |
|---|---|---|---|
| 6/8 | Head Score | - 0.257* | 0.540 |
| 4/8 | Spine Score | - 0.828* | 0.011 |
| 3/8 | Leg Score | - 0.845* | 0.008 |
| 2/8 | Arm Score | - 0.604* | 0.113 |
| * - Spearman’s correlation coefficient; p-value < 0.05 was considered as statistically significant. | |||
Table 6: Correlation between various PTSA score and comorbidities.
Moreover, PTSA scores were also observed to be inversely correlated to the number of pathologies (Table 7). However, in this case, both Spine (p-value=0.011) and Leg PTSA scores (p-value=0.008) were significantly correlated to the comorbidities.
| Hypomobility scale | % Health | Hypomobility | Number of study subjects |
|---|---|---|---|
| 0 | 76-100 | NO | 0 |
| 1 | 51-75 | Minimal | 8 |
| 2 | 26-50 | Moderate | 0 |
| 3 | 1-25 | Significant | 0 |
| 4 | 0 | Immobile | 0 |
Table 7: Distribution of study subjects based on hypomobility.
After comparing hypomobility scale with PTSA score (%), it was observed that all the study subjects had minimal hypomobility (Table 1).
Receiver operating characteristic (ROC) curve analysis
Spine (p-value=0.025), Leg (p-value=0.046), and Arm (p-value=0.025) PTSA scores had a sensitivity and specificity of 100% with cut-off values of 67.5, 69.5, and 69.0, respectively. Similarly, Head PTSA (p-value=0.025) score had a sensitivity and specificity of 100% with cut-off values of 62.5 (Table 8).
| Total no. of subjects | PTSA Score |
Total no. of subjects with PTSA score more than or equal to indicated | Area under ROC curve | p-value | Cut-off value | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|
| Head PTSA Score | |||||||
| 8 | ≥ 70% | 1 | 1.000 | 0.127 | 67.5 | 100% | 100% |
| 8 | ≥ 65% | 3 | 1.000 | 0.025 | 62.5 | 100% | 100% |
| 8 | ≥ 60% | 5 | 1.000 | 0.025 | 59.0 | 100% | 100% |
| Spine PTSA Score | |||||||
| 8 | ≥ 70% | 3 | 1.000 | 0.025 | 67.5 | 100% | 100% |
| 8 | ≥ 65% | 5 | 1.000 | 0.025 | 64.0 | 100% | 100% |
| 8 | ≥ 60% | 6 | 1.000 | 0.046 | 58.0 | 100% | 100% |
| Leg PTSA Score | |||||||
| 8 | ≥ 70% | 2 | 1.000 | 0.046 | 69.5 | 100% | 100% |
| 8 | ≥ 65% | 4 | 1.000 | 0.021 | 63.0 | 100% | 100% |
| 8 | ≥ 60% | 6 | 1.000 | 0.046 | 59.0 | 100% | 100% |
| Arm PTSA Score | |||||||
| 8 | ≥ 70% | 3 | 1.000 | 0.025 | 69.0 | 100% | 100% |
| 8 | ≥ 60% and ≥65% | 7 | 1.000 | 0.127 | 61.5 | 100% | 100% |
Table 8: Various PTSA scores and their ROC curves with sensitivity and specificity for each cut-off value.
Thus, Spine, Leg, and Arm PTSA scores start revealing statistically significant cut-off value at a PTSA score of ≥ 70%.While, Head PTSA score start revealing statistically significant cut-off value at a PTSA score of ≥ 65%.
Discussion
The goal of this research was to assess PTSA ability to assess and quantify musculoskeletal health and potential of injury. The results show an inverse correlation between PTSA score for participants, number of pathologies, severity of pain, and comorbidities. In addition, Spine (p-value=0.025), Leg (p-value=0.046), and Arm (p-value=0.025). PTSA scores had a sensitivity and specificity of 100% with cut-off values of 67.5, 69.5, and 69.0 respectively. Similarly, Head PTSA (p-value=0.025) score had a sensitivity and specificity of 100% with cut-off values of 62.5. Thus, Spine, Leg, and Arm PTSA scores start revealing statistically significant cut-off value at a PTSA score of ≥ 70%. While, Head PTSA score starts revealing statistically significant cut-off value at a PTSA score of ≥ 65%.
The results of this research indicate value with PTSA scoring to identify when subjects will experience symptoms of musculoskeletal pain, severity of the pain, and co morbidities in region below the cut off value identified.
A limitation of the current study was the small sample size (8 participants), which limited the statistical power. Therefore, the results of the present study must be interpreted with caution.
Conclusion
The present study reported correlation between PTSA score for participants, number of pathologies, severity of pain, and comorbidities. In addition, sensitivity and specificity was found to be 100%. Future studies should be performed with larger number of subjects to prove PTSA assessment effectiveness in quantifying musculoskeletal health and potential of injury.
References
- Catling DC. Astrobiology: A Very Short Introduction. Oxford University Press 2014.
- Bureau of Labor Statistics - http://1.usa.gov/1uCQQXn
- Cuddy AJC, Wilmuth CA, Yap AJ, et al. Preparatory power posing affects nonverbal presence and job interview performance. J Appl Psychol. 2015;100:1286-95.
- Bizzarri M, Masiello MG, Giuliani A, et al. Gravity Constraints Drive Biological Systems toward Specific Organization Patterns: Commitment of cell specification is constrained by physical cues. Bioessays. 2018; 40.
- Moran RW, Schneiders AG, Mason J, et al. Do Functional Movement Screen (FMS) composite scores predict subsequent injury? A systematic review with meta-analysis. Br J Sports Med. 2017;51:1661-9.
- Pujitha K, Parvathi G, Sekhar KM. Postural changes in heart rate and blood pressure with ageing. Int J Physiother Res. 2014;2:751-56.