Research Article - Current Pediatric Research (2024) Volume 28, Issue 5
Postnatal care utilization and associated factors among rural women in Northwest Ethiopia: Cross-sectional study.
Yoseph Merkeb Alamneh*
Department of Biomedical Sciences, Debre Markos University, Debre Markos, Ethiopia
- Corresponding Author:
- Yoseph Merkeb Alamneh
Department of Biomedical Sciences,
Debre Markos University,
Debre Markos,
Ethiopia
E-mail: ymerkeb11@gmail.com
Received: 29 April, 2024, Manuscript No. AAJCP-21-28950; Editor assigned: 02 May, 2024, Pre QC No. AAJCP-21-28950 (PQ); Reviewed: 16 May, 2024, QC No. AAJCP-21-28950; Revised: 23 May, 2024, Manuscript No. AAJCP-21-28950 (R); Published: 30 May, 2024, DOI:10.35841/0971-9032.28.05.2239-2244.
Abstract
Globally, of the reported 289,000 maternal deaths, 67% occurred within 42 days of the postnatal period and 75% of newborn deaths occurred during the first week of life. Although the use of postnatal care services showed little improvement in Ethiopia, it is far below the expected level. In Ethiopia (2016), only 17% of women aged 15 to 49 years got postnatal care within two days of delivery, while 81% did not have postnatal care until 42 days. Despite this evidence, the data concerning the utilization of postnatal care services in the study area is scarce. Thus, this study aims to determine postnatal care services utilization and its associated factors among women in Gozamen woreda, Northwest Ethiopia. A cross-sectional community-based study was conducted between May and July 2020 among women in Northwest Ethiopia who had child aged 43 days to 6 months. A multi-stage sampling method was used to select a total of 756 participants using systematic random sampling method. The overall utilization of the postnatal health service in Gozamen woreda is said to be low. Mothers' education, ANC follow up, place of delivery and postnatal care awareness had a positive impact on the use of postnatal care services. Interventions aimed at increasing women's awareness about the importance of postnatal services and improving accessibility, particularly in rural areas, are required. In addition, Gozamen woreda health office and other stakeholders should help and promote rural health extension workers in order to enhance women's knowledge about the importance of postnatal care services utilization.
Keywords
Postnatal care service, Utilization, Northwest Ethiopia, Maternal deaths.
Introduction
Postnatal Care (PNC) is described as services for women and newborns immediately after birth and up to six weeks, to ensure optimal health for both mothers and their infants. The postnatal period (the first six weeks of life) is highly pertinent for newborns and mothers. PNC is a major part of continuum of quality of maternity care that help to prevent complications after childbirth and reducing maternal and infant morbidity and mortality. Nearly 30% of mothers used postnatal care services worldwide, 13% in sub-Saharan Africa, of whom 17% received PNC within the first two days of childbirth. A study in Northwest Ethiopia showed that 30.8% of mothers take postnatal care services within 3-7 days after delivery.
Postnatal care services given for the first hours, days and weeks after childbirth is a critical time for both the mothers and the newborns; but this period has received less attention from health care providers compared to pregnancy and delivery care [1]. In the first two days after birth, two thirds of maternal and neonatal deaths occur; thus postnatal care is necessary for both the mother and the child to alleviate the risk of preventable death. The World Health Organization (WHO) recommends postnatal care visit within the first 24 hours, on day 3, between 7-14 days and 6 weeks after birth.
According to Ethiopian Demographic and Health Survey (EDHS, 2016), only 17% of women aged 15 to 49 years got postnatal check within two days of delivery, while 81% did not have postnatal check until 42 days.
About 99% maternal and neonatal deaths occur in the developing world and most maternal and infant deaths occur within the first six weeks of birth. Neonatal death accounted for 62% of all infant deaths and accounted for 45% of under five deaths. In Ethiopia, Pregnancy-Related Mortality Ratio (PRMR) has declined from 676 deaths in EDHS 2011 to 412 deaths in EDHS 2016 per 100,000 live births. According to EDHS 2016, child mortality has declined from 97 deaths per 1,000 live births in 2000 to 48 deaths in 2016, while infant mortality rates in the Amhara region were reported as 85 per 1,000 live births. Additional, EDHS reported PNC utilization remained below 10% (3.4% in 2000, 5.8% in 2005 and 7% in 2011). This report also showed that 32% of women in urban areas provided PNC services compared to 2% in rural communities.
Different studies have showed that several factors have an important impact on the utilization of PNC services. For example, mother education, mother employment, husband education, place of delivery, mother's level of awareness of the need for postnatal check-up, distance to the health care institution, number of antenatal care visits, household income, awareness of early postnatal care, length of hospitalization after delivery, past experience of PNC use, appointment for PNC, complication of delivery, mode of delivery were reported as factors significantly associated with the use of PNC services.
Ethiopia has introduced high impacts and cost-effective health programs in order to enhance the health status of the population and reduce maternal and neonatal deaths, as well as reinforce the health infrastructure [2]. These initiatives include expansion of family planning services, recruitment and implementation of additional health providers, referral system like referral system, service enhancement, health extension program, routine immunization. Despite numerous measures by the Ethiopian government, maternal and neonatal mortality rates remain high.
Though PNC has many benefits and significantly decreases maternal and infant mortality, utilization of postnatal services in Ethiopia is limited. PNC services are made available free of charge to all women but the use of services is very limited. Postnatal care services given for the first hours, days and weeks after childbirth is a critical time for both the mothers and the newborns; but this period has received less attention from health care providers compared to pregnancy and delivery care.
It is strongly recommended that well-structured and up-to-date information on the use of postnatal care services have been used to reduce maternal and neonatal mortality by providing adequate postnatal care services. Despite few facility-based studies have been performed in Ethiopia that indicates the magnitude of PNC service use and related factors; there is limited evidence of the use of postnatal care services in Ethiopia, particularly in the area of study. Moreover, there is no community based studies done to assess utilization of PNC services and associated factors among rural women in Gozamen Woreda, Northwest Ethiopia. Further, even though a few studies have been conducted in Ethiopia, these studies have failed to consider important factors, such as distance to health institutions and women’s knowledge on when to access PNC services, which significantly affect the utilization of PNC services. Thus, this study was conducted to address the gap in the utilization of PNC services by identifying the factors affecting the utilization of PNC services among women who have given birth in the last 6 months in Gozamen Woreda, Northwest Ethiopia.
Materials and Methods
A community-based cross-sectional study was conducted from May to July 2020 among women who had children aged 43 days to 6 months in Gozamen Woreda Northwest Ethiopia. The study was conducted in Gozamen Woreda, East Gojjam zone, Amhara Region Northwest Ethiopia, which is one of 17 woreda in East Gojjam zone, located 299 km from the capital Addis Ababa and 265 km from the city of Bahia Dar, regional city of Amhara. The Woreda consists of 26 kebeles.
According to 2020 1st quarter report of Gozamen there is a total of 164,816 population, of which 82078 (49%) are males and 82738 (51%) are females. In the Woreda, there are six health center, one private pharmacy, one private clinic and 26 health posts.
The study participants were selected using a multi-stage sampling technique. There are 26 kebeles in the Woreda, one urban and twenty-five rural kebeles, of which seven kebeles were randomly selected by lottery method at stage one. In stage two, 8,122 households with mothers who gave birth in the 6 months were identified from 38,329 households. Of these households, 2141 were registered in selected kebeles that gave birth in the 6 months using health extension family registry files. Then, in stage three, 756 mothers who had been born in the last six months were selected using a simple random sampling technique and a proportional allocation of the size of each kebele. Finally, the mothers who gave birth in the 6 months, prior to the study, were interviewed. One woman engaged in the study per household and three visits were made for absence in the first visits.
The dependent variable in this study is the utilization of postnatal care services. Independent variables include: variables of socio-demography (age of mother, religion, educational status, occupation, current marital status, ethnicity, household economy), reproduction related variables (obstetric complication, postpartum complication, gravidity and parity, length of stay at health facility after delivery, previous history of PNC service, ANC service utilization, mother’s child experience), health facility related variables (delivery attaining, place of delivery, advice on discharge).
Data collection tools and procedures
Data were obtained by face-to-face interview using a pre-tested and standardized questionnaire. The questionnaire was initially written in English and translated into Amharic (local language), then reverted to English to ensure consistency. The questionnaire was developed by examining relevant literature in Ethiopia and internationally. Questions on socioeconomic status, demographic factors, reproductive history, prenatal care and postnatal care were included in the questionnaire.
Data processing and analysis
The data were checked, cleaned, entered into Epi-Data version 3.1 and exported for analysis to SPSS version 20. To summarize the data and identify the association of independent variables with outcome variables, both descriptive statistics and multivariate analytical models were used. Binary logistic regression has been used to identify factors associated with the use of PNC services on mothers and P-value variables of less than or equal to 0.2 have been selected in multiple logistic regression models to control the potential effect of confounders. Interaction, mediation and multi co-linearity between independent variables were checked on the basis of assumptions such as tolerance, Variance Inflation Factors (VIF), interaction correlation coefficient and others to ensure the fitness of the logistic regression model.
Then, the final model was tested for its fitness by Hosmer and Lemeshow p-value and p-value>0.05 are good fit. Finally, the modified Odds Ratios (AORs) with 95% CI were used to determine the associations at p-value ≤ 0.05 for statistical significance as independent associated factors of the PNC service utilization.
Results
Socio-demographic descriptive characteristics of participants
A total of 756 mothers, who gave birth in the last six months, were interviewed in this study, ages ranging from 15-47 years of age, 230 (30.4%) aged 30-34 years. The mothers' mean age was 27 years with Standard Deviation (SD) ± 6.25 years. With regards to educational level, nearly a quarter of 245 (32.4%) attended elementary school and 70 (9.3%) completed college and above. About 513 mothers (67.9%) were housewives while 633 (83.7%) were married. Around one-third, (31.7%) of the respondents indicated that they lived more than an hour's walk to the nearest health facility. For descriptions of other sociodemographic characteristics identified.
Obstetric history and knowledge of women on PNC services
Nearly half of the respondents, 350 (46.3%) planned and supported the nature of the pregnancy. About 559 (73.9%) of respondents attended ANC at least once during pregnancy and 81 (10.7%) women had a history of childbirth. Of the total respondents, 219 (29.0%) were faced postpartumcomplications.
Two hundred and thirty-three respondents (30.8%) delivered at home. With respect mode delivery, most respondents, 579 (76.6 %) delivered via spontaneous vaginal delivery. Five hundred and forty (68.0%) of respondents knew of the availability of PNC services at health facilities [3].
Utilization of postnatal care services
Two hundred six (27.2%) mothers used postnatal care services from a total of respondents. Of whom, 52 (25.2%) mothers accessed the service more than three times and most postnatal care users accessed the service from health extension workers. Among mothers who received postnatal care services, 154 (74.8%) of respondents said that they received postnatal care services after two weeks of delivery. With regards to the types of service use during the postnatal visit, 40 (19.4%) of the respondents were consulted on exclusive breast feeding and support for appropriate feeding practices, 19 (9.2%) were assessed for danger signs, measurement and record weight and temperature monitoring.
Respondents who visited ANC at least once used PNC services 199 (96.6%). About 181 (87.9%) respondents who knew that PNC service was available used PNC services. Ninety-four (45.6%) respondents who experienced complications during delivery had used PNC services. About 139 (67.5%) respondents who had previous history of obstetrics problems, used PNC services. One hundred and seventy respondents (56.8%) who knew the time of PNC services, used PNC services.
| Type of service | Frequency (%) |
|---|---|
| Assess and check for bleeding, temperature | 24 (11.7) |
| Counseling on nutrition and give vitamin A supplementation | 30 (14.6) |
| Counseling on exclusive breast feeding | 40 (19.4) |
| Provide counseling for family planning | 26 (12.6) |
| Counsel on danger signs and home care for mothers and newborns | 28 (13.6) |
| Assess for danger signs, measure and record weight | 19 (9.2) |
| Counseling on refer for complications such as bleeding, infections or postnatal depression | 25 (12.1) |
| Counseling on hygiene and cord care | 14 (6.8) |
Table 1. Contents of PNC services which women had received during on recommended time of visit in Gozamen Woreda, Northwest Ethiopia, 2020 (n=756).
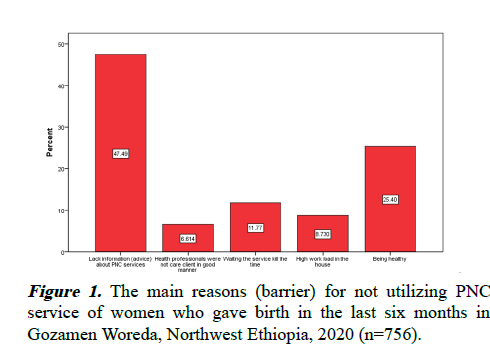
The mothers have offered various reasons for not attending postnatal care services. Nearly one-third of respondents 242 (32.0%) indicated that the reason they did not use postnatal services was because they did not realize the availability of PNC services in health facilities. The most common reason was that women were not informed by health care providers of the importance of postnatal care.
Among these, the most frequent reasons provided by the participants for not using postnatal care were the lack of awareness (advice) on postnatal care services, followed by the apparently healthy (Figure 1). Assess for danger signs, measure and record weight.
Factors associated with postnatal care service utilization
The postnatal care services utilization was associated to demographic and obstetric variables. Thus, both bivariate and multivariate analyzes were performed to identify independent demographic and obstetric variables showing an important association for the utilization of PNC services [4].
During the bivariate analysis, all variables showing a statistically significant association with p-value<0.2 were entered into multivariate analysis and a statistically significant was determined at p<0.05. In bivariate analysis, demographic variables associated with the use of postnatal care services were educational status, occupation of women and walking distance of health facilities. Obstetric variables such as nature of the pregnancy, number of pregnancies, ANC visit, place of delivery, birth outcome, postpartum complication, postnatal care in the previous delivery, knowledge about availability of PNC, knowledge about the time of visit of PNC services showed statistically significant association. In multivariable analysis, women's education level, walking distance from the health facility, ANC visit, place of delivery, complication, knowledge of the availability of PNC, knowledge of the time of use of PNC services showed statistically significant association for the use of PNC services.
College and above educational level (AOR: 3.53, 95% CI: 1.57, 7.97), Knowledge about availability of PNC (AOR: 5.42, 95% CI: 2.36, 12.42), At least one ANC visit (AOR: 2.46, 95% CI: 1.65, 9.39) distance to health facility (AOR: 5.25, 95% CI: 3.56, 7.74) delivery at hospital (AOR: 7.31, 95% CI : 2.98, 17.91), postpartum complication (AOR: 5.69, 95% CI: 3.98, 8.13) and knowledge on when to access PNC services ( AOR: 2.66, 95% CI: 1.86, 3.79) were found to be significantly associated with postnatal care service utilization in multivariate logistic regression analysis [5].
The educational status of women shows strong association with the use of postnatal care services. Likewise, women who completed college and beyond and read and write were 3.53 and 2.07 times more likely to use postnatal care services than those who were unable to read and write respectively.
Moreover, women's knowledge on PNC service availability was another indicator variable for use in postnatal care services. Since women's knowledge of the availability of postnatal care services increased the use of PNC service 5.42 times more likely than women without knowledge of the services. Furthermore, all mothers who attended at least one ANC visit were 2.46 times more likely than mothers who did not attend ANC to use postnatal care services. In comparison, mothers who gave birth at the health center and hospital were 4.43 and 7.31 times more likely to use for postnatal care than mothers who gave birth at home. In addition, all mothers who used postnatal care in the previous birth were 5.69 folds (AOR: 5.69, 95% CI: 3.98, 8.13) higher than their counter parts to use postnatal care in the next birth. Besides that, knowledge of the time of visit for PNC services was yet another predictor variable for the use of postnatal care services. As knowledge of women about the time of PNC visit increased, the use of PNC service increased by 2.66 folds higher than women who lacked knowledge about the time of PNC visit (AOR: 2.66, 95% CI: 1.86, 3.79). Finally, mothers traveling to health facilities less than an hour's walking distance is 5.25 times more likely to use postnatal care than mothers traveling longer than an hour (AOR: 5.25, 95% CI: 3.56, 7.74).
Discussion
This study is important for the understanding of current PNC practices and factors that influence the use of PNCs by individuals, families and communities, as well as by policy makers, to develop strategies that can be implemented and integrated into the continuum of care at the facility, home and community level, to improve the quality of maternal and newborn health services [6].
PNC coverage is 34.3% in Ethiopia and 44.5% in Amhara region. The Government of Ethiopia has adopted a policy aimed at improving the health system in order to provide quality care, especially skilled birth attendance and preventive services through a comprehensive referral system that involves zonal hospitals and health centers as well as health posts. Although PNC has many benefits, it significantly lowers maternal and infant mortality and all women offer free PNC services, the use of PNC services in Ethiopia is very limited. This research was aimed at assessing the extent of women's use of postnatal care and identified factors that affect the utilization of the service among women who gave birth in the last six months in Gozamen Woreda, Northwest Ethiopia. The study showed low utilization PNC services in the study area. The key reason why PNC service was not used was lack of knowledge of the availability of PNC service in health facilities. Women were more likely to access postnatal services if they completed more than a primary education, had at least one ANC visit, delivered at health facilities and had knowledge of the time of PNC services visit. In overall, the result of this study revealed that of 756 participants, 206 (27.2%) with confidence interval (24.0%, 30.4%) had accessed PNC services within 6 weeks of delivery.
According to this study, the use of postnatal care service is lower than a study done in India 35.86%, in Nepal 43.2%, in Kenya 33%, in Malawi 41% and in Mozambique 40%.
The plausible explanation for the inconsistencies may be attributed to cultural disparities and regional variables, social status and governments' political concerns. Another possible explanation for the difference may be related to variation in methodology, service delivery and accessibility of health organizations. For investigating and understanding such variation, however, further analysis is required [7].
This result is also lower than the studies in Addis Ababa, 65.6%, Gondar, 66.83% and Adwa 78.3%, Oromiya 31.7% and Debre Markos 33.5%. However, the use of postnatal care services in this report is higher than that of a study done in, South Ethiopia 22.7%, Jabitena district, 20.2%. The present findings were also higher than a study carried out in four regions in Ethiopia (Amhara, Oromia, SNNP and Tigray), in which only 10.6% of women used PNC services. Methodological discrepancies of the studies and the variations in residency and length of study subjects may be the potential reasons for these variations. Another potential cause for this disparity may be due to low educational status and disadvantaged women give less attention to the need for postnatal care services. Furthermore, it may be attributed to lack of awareness on postnatal care, low maternal understanding of danger signs and low attention of health care providers in postnatal care counseling.
In this study, lack of knowledge on the availability of PNC services was the key reasons why PNC services were not used. Even if most of the respondents came to ANC and delivered at health facilities, they did not know or hear about the availability and provision of PNC services [8].
In addition, the opportunities of the postnatal services are influenced by socio-economic factors. According to this study, there have been 3.5 times the chances of using PNC service for women who completed college and above in education than those who couldn't read and write. This finding was in line with a study done in Nepal, Cambodia, Africa, Northwest Ethiopia. This may be related to the fact that as women are educated, they have high levels of choice and use of health care services; furthermore, education contributes to awareness of mothers and more knowledge on the utilization of postnatal care services. Likewise, this study also revealed that women who gave birth at the hospital were 7.31 folds more likely to use PNC service than those who gave birth at home. This result is in line with researches carried out in Tanzania, Nepal and Northwest Ethiopia. The possible reason for the similarity between place of delivery and use of postnatal care services can be demonstrated by women who gave birth in health institutions, have greater chances to obtain postnatal carerelated health information, access to PNC services benefits during their stay in health facilities. Moreover, knowledge of availability of postnatal care services was reported as a major factor impacting the utilization of PNC services; women who were informed about PNC services were more likely to use PNC services than those who did not know. This result supported the studies done conducted in Nepal and Tanzania. Moreover, mothers who attended four or more ANC visits were more likely to receive postnatal service which is comparable to those reported the studies done in Amhara Region, Ethiopia.
Additionally, the use of postnatal services was higher among women with complications during delivery which is comparable to a study done in Northwest Ethiopia.
With respect to distance from the healthcare facility, the study found that mothers going less than one hour on foot were 5.25 times more likely to use postnatal care services than women going more than one hour. This finding is consistent with study outcomes done in, China, Dembecha and Gondar. The explanation for this may be that mothers are getting exhausted and also because having a local health center increases access to health services [9].
Furthermore, distance from the healthcare organization was a major problem in rural residency and some participants complained that they needed to walk for up to 2 hours to reach the nearest health center; this could be impacted in terms of time and travel costs. This finding is supported by the study done in Cambodia, Nepal and Palestine. The possible explanation to this might be due to that women only attend health services while they are faced by complications and sickness. Also, the potential reasons for this can be that mothers with complications during delivery are consulted immediately after delivery by their health care providers and advised about the need for PNC services.
Therefore, this study should give special attention to all identified factors to policy makers, programmers, researchers and providers engaged in caring for women and newborns following birth. The new guidelines also required timing and content of special considerations for post-natal care tailored for mothers and newborns in low income countries. Additional studies are also recommended to generate additional factors that have been positively linked to the access and use of PNC services globally and in developing countries in particular [10].
Conclusion
The overall utilization of the postnatal health service in Gozamen Woreda is said to be low. Mothers' education, ANC follow up, place of delivery, postnatal care awareness had a positive impact on the use of postnatal care services. Interventions aimed at increasing women's awareness of the importance of postnatal services and improving accessibility, particularly in rural areas, are required. In addition, the health office and other stakeholders should help and promote rural health extension workers and health facilities to increase the availability of health education in order to enhance women's knowledge of the importance of post-natal care services.
References
- Lawn JE, Blencowe H, Oza S, et al. Every Newborn: Progress, priorities and potential beyond survival. Lancet 2014; 384: 189-205.
[Crossref] [Google Scholar] [PubMed]
- Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: Examining the scale of the problem and the importance of context. Bull World Health Organ 2007; 85: 812-819.
[Crossref] [Google Scholar] PubMed]
- Alemayeh H, Assefa H, Adama Y. Prevalence and factors associated with post natal care utilization in Abi-Adi Town, Tigray, Ethiopia: A cross sectional study. Int J Pharm Biol Sci 2014; 8: 23-35.
- Bhaisare KA, Khakase GM. Study of utilization of postnatal care services in tribal area, Maharashtra. Int J Med Sci Public Health 2014; 3: 1487-1492.
- Ronsmans C, Graham WJ. Maternal mortality: Who, when, where, and why. Lancet 2006; 368: 1189-1200.
[Crossref] [Google Scholar] [PubMed]
- Wudineh KG, Nigusie AA, Gesese SS, et al. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: A community-based cross-sectional study. BMC Pregnancy Childbirth 2018; 18: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Limenih MA, Endale ZM, Dachew BA. Postnatal care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos town, northwestern Ethiopia: A community-based cross-sectional study. Int J Reprod Med 2016; 2016.
[Crossref] [Google Scholar] [PubMed]
- Abie A, Belay G, Asmare E, et al. Male partner involvement in postnatal care service utilization and associated factors: A community-based cross-sectional study in Motta district, Northwest Ethiopia. PLoS One 2023; 18: e0276477.
[Crossref] [Google Scholar] [PubMed]
- Berhe A, Bayray A, Berhe Y, et al. Determinants of postnatal care utilization in Tigray, Northern Ethiopia: A community based cross-sectional study. PLoS One 2019; 14: e0221161.
[Crossref] [Google Scholar] [PubMed]
- Yoseph S, Dache A, Dona A. Prevalence of early postnatal-care service utilization and its associated factors among mothers in Hawassa Zuria district, Sidama regional state, Ethiopia: A cross-sectional study. Int J Gynaecol Obstet 2021; 2021: 1-8.
[Crossref] [Google Scholar] [PubMed]