Research Article - Otolaryngology Online Journal (2016) Volume 6, Issue 4
Possible Participation of Irregularly Surfaced Carotid Plaques in the Genesis of Idiopathic Transient Vestibulopathy
- *Corresponding Author:
- Tomoe Yoshida, MD, phD, Department of Otorhinolaryngology, Toho University Sakura Medical Center, 564-1 Shimoshizu, Sakura, Chiba 285-8741, Japan, Tel: +81-43-462-8811, Fax: +81-43-487-9061, E-mail: tomoe@med.toho-u.ac.jp
Received date: September 26, 2016; Accepted date: October 20, 2016; Published date: October 24, 2016
Abstract
Objective: In our specialist vertigo center, patients with vertigo of sudden onset and rapid recovery (within 24 hour), which we call “idiopathic transient vestibulopathy’ (ITV), are not uncommon. The present study aimed to clarify the underlying mechanism(s) of ITV.
Methods: Consecutive ITV patients (n=39) who attended the Vertigo Center of Toho University Sakura Hospital were enrolled with a control group of 64 consecutive patients with vestibular neuritis (VN). At their visit, a caloric test and carotid ultrasonography (CUS) were performed.
Results: By caloric test, most of the ITV patients had no vestibular dysfunction whereas the majority of the VN patients had severe vestibular dysfunction. By CUS, atherosclerosis was more advanced in the ITV patients. 39% of ITV and 18% (p=0.003 vs. ITV) of VN patients had irregularly surfaced plaques. Conclusion: Irregularly surfaced carotid plaque, which often indicates the presence of thrombogenic ulcer, fissure or previous disruption, was frequent in ITV patients, suggesting its participation in transient ischemic vestibular nerve dysfunction and consequent vertigo in at least one-third of ITV patients.
Keywords
Caloric test; Carotid ultrasonography; Microembolism; Plaque characteristics; Vestibular neuritis
Introduction
Vertigo is defined as a rotational sensation associated with nystagmus and often accompanied by nausea and vomiting, and somatic instability such as gait disturbance [1]. In patients with vertigo that occurs suddenly and subsides rapidly (within 24 hour) the caloric test, a vestibular dysfunction test, is generally negative. Because its underlying disease is poorly understood, and does not satisfy the criteria of vestibular neuritis (VN), in which vertigo continues for more than 24 hour, the caloric test is positive, and steroid therapy is usually effective [2-4], in our specialist vertigo center we arbitrarily called this type of vertigo “idiopathic transient vestibulopathy” (ITV). There are a number of diseases that cause vertigo (i.e., vestibular nerve disease, regional and systemic circulatory diseases that cause vestibular ischemia, cerebrocerebellar disease, and so on) [5-7]. The underlying diseases for other than ITV are well known, but that for ITV is poorly understood.
In ophthalmologic diseases, there is a symptom known as “amaurosis fugax”, which is characterized by abrupt but transient loss of unilateral or bilateral vision. Amaurosis fugax is often caused by occlusion of the retinal artery or its mother artery by microemboli originating from the carotid artery, heart, aortic arch or cerebral arteries [8,9]. Of these, the carotid artery is considered to be the most important source of the emboli [9]. Because ITV and amaurosis fugax resemble each other in their abrupt onset and transient nature, there is a possibility that ITV is caused by transient blood flow disturbance in the vestibular artery caused by microemboli originating mainly from the carotid artery with resultant vestibular ischemia and dysfunction. Therefore, in the present study we used ultrasonography to examine the relationship between ITV and the characteristics of carotid artery plaque.
Materials and methods
Ethical Statement
This retrospective study was performed in the Department of Otorhinolaryngology, Toho University Sakura Hospital. Because routine clinical examinations were used for the diagnosis of vertigo and its underlying diseases, approval by the Ethical Committee of Toho University for the present study was not required. Informed consent on the use of the clinical data was given by all patients enrolled in the present study.
Arbitrary Definitions of ITV and VN
Because the definition and mechanism(s) of ITV are not settled, vertigo with sudden onset and termination within 24 hour without new cerebral or cerebrovascular disease was categorized as ITV and that lasting more than 24 hour without cerebral or cerebrovascular disease was categorized as VN (Table 1).
| Variables | ITV | VN |
|---|---|---|
| (1) Subjective symptoms | ||
| Onset of vertigo | Sudden | Sudden |
| Terminate | £24 hour | >24 hour |
| Rotary vertigo | Present | Present |
| Nausea/vomiting | Present | Present |
| Somatic disability | Absent | Absent |
| (2) Physical examination | ||
| Positional nystagmus | Fixed direction | Fixed direction |
| Auditory disturbance | Absent | Absent |
| (3) Vestibular function tests | ||
| Caloric test | Usually negative | Usually severe |
| Stabilometry | Severely positive | Severely positive |
| (4) Cerebral disease | Absent | Absent |
| (5) Cerebrovascular disease | Absent | Absent |
Table 1: Arbitrary Criteria for Idiopathic Transient Vestibulopathy (ITV) and Comparison with Vestibular Neuritis (VN).
Subjects
There were 8228 consecutive patients with vertigo who visited the emergency room or vertigo center of Toho University Sakura Hospital between December 2008 and March 2015. Of them, 39 patients were diagnosed as ITV and 64 as VN by the arbitrary criteria shown in (Table 1). The clinical characteristics of the ITV and VN patients are shown in (Table 2). A caloric test was performed at first visit (2.35 ± 1.83 days after the onset of ITV, and 2.71 ± 1.71 days with VN), followed by carotid ultrasonography, and magnetic resonance imaging (MRI) and angiography (MRA) of the brain. For the present retrospective study, medical records were reviewed to determine clinical presentation, caloric test results, carotid ultrasonographic results, treatment and recovery. The patients with acute cerebrocerebellar infarction or significant cerebral arterial stenosis were excluded.
| Variables | ITV n=39 |
VN n=64 |
P value |
|---|---|---|---|
| Age (years±SD) | 67.1±12.0 | 56.4±14.6 | 0.0002* |
| Sex (M/F) | 16/23 | 35/29 | 0.1546 |
| Early history | |||
| Cardiac disease | 7 | 4 | 0.0975 |
| Cerebrovascular disease | 4 | 1 | 0.0667 |
| Dizziness | 12 | 4 | 0.0015* |
| Smoking | 8 | 16 | 0.9354 |
| Alcohol intake | 14 | 24 | 0.5447 |
| Hypertension | 23 | 18 | 0.0012* |
| Diabetes mellitus | 9 | 14 | 0.6844 |
| Dyslipidemia | 17 | 30 | 0.7413 |
| Hyperuricemia | 2 | 7 | 0.562 |
| *p<0.01 | |||
Table 2: Clinical Characteristics of the Patients with Idiopathic Transient Vestibulopathy (ITB) or Vestibular Neuritis (VN).
Clinical Examination
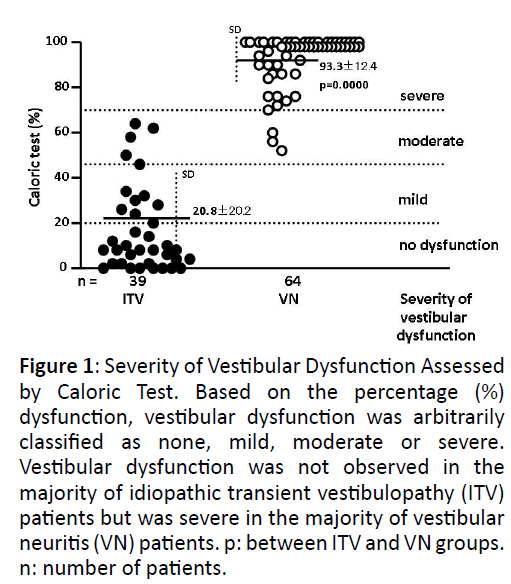
Caloric test: Routine caloric test was performed and the severity of vestibular dysfunction was graded stepwise from 0 to 100% in which 0 -< 20, ≥ 20-< 45, ≥ 45-< 70 and ≥ 70 were classified as no, mild, moderate or severe dysfunction, respectively.
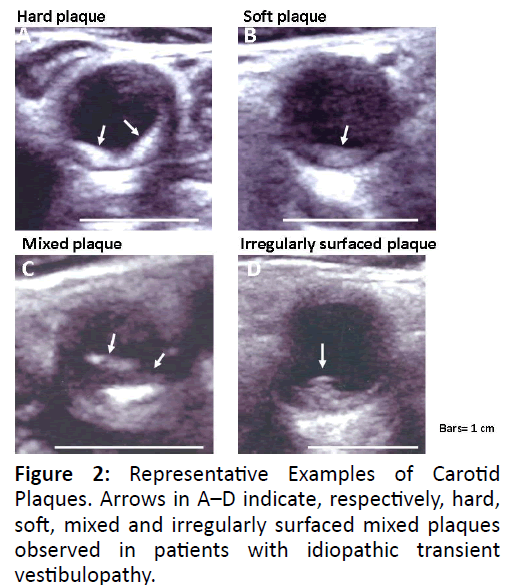
Carotid ultrasonography: An ultrasonic apparatus (Ascendus XG, Hitachi Co, Tokyo, Japan) was used for the present study. The obtained records were analyzed and the plaque morphology was classified independently by two observers who did not participate in the carotid ultrasonographic study and did not know the purpose of analysis but were specialists in vascular ultrasonography.
The following parameters were analyzed by the observers
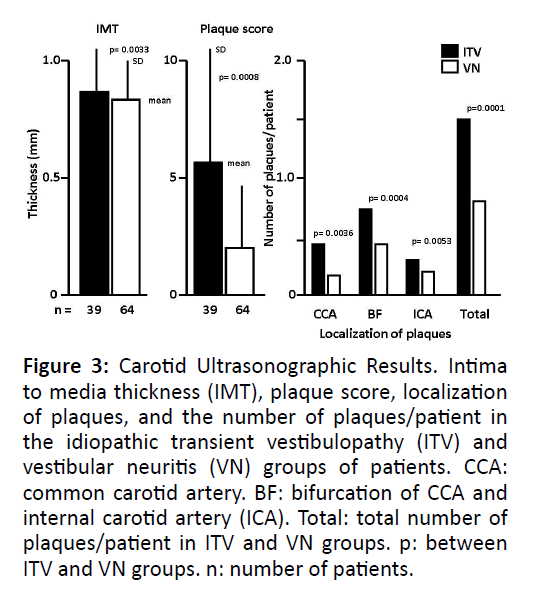
(1) Intima–media thickness (IMT): The distance between the luminal surface and the internal elastic lamina. Plaque was defined as IMT>1.1.
(2) Plaque score: Thickest IMT in the proximal and distal segments of the common carotid artery, bifurcation and internal carotid artery was measured and the sum was calculated. The average value of the sum of the IMT of the left and right carotid arteries was called the “plaque score”.
(3) Carotid stenosis: IMT on both sides and the distance between the internal elastic laminae ≥ 0.50 was determined as significant stenosis and expressed as percentage (%) stenosis.
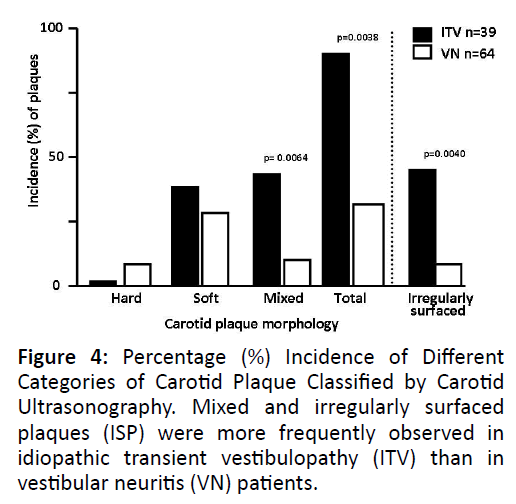
(4) Plaque morphology: plaques were classified as hard when the echo intensity of the plaque was greater than the echo intensity of the media; soft when the echo intensity of the plaque was less than the echo intensity of the media; mixed when both hard and soft portions existed in the same plaque. The plaques were further classified as calcified when the high echo characteristic of calcium existed; as ulcer when a defect in the plaque existed. Plaques with an irregular surface were classified as irregularly surfaced plaques (ISP), because ISP is a risk factor for cerebrovascular events, including amaurosis fugax.
Statistical Analysis
The obtained data were expressed as mean ± SD and were analyzed by Fisher’s exact test or Mann- Whitney U-test. The value of p<0.05 was considered statistically significant.
Results
Patients’ Characteristics
Patients in the ITV group were older than those in the VN group. Also, the incidence of a history of dizziness and hypertension was significantly higher in the ITV group than in the VN group (Table 2).
Caloric Test
The severity of vestibular dysfunction assessed by caloric test was severe in the majority of VN patients, but absent in the majority and mild to moderate in a small number of ITV patients (Figure 1).
Figure 1: Severity of Vestibular Dysfunction Assessed by Caloric Test. Based on the percentage (%) dysfunction, vestibular dysfunction was arbitrarily classified as none, mild, moderate or severe. Vestibular dysfunction was not observed in the majority of idiopathic transient vestibulopathy (ITV) patients but was severe in the majority of vestibular neuritis (VN) patients. p: between ITV and VN groups. n: number of patients.
CUS
Figure 2 shows representative examples of the ultrasonic appearance of carotid plaques (i.e., hard, soft, and mixed, and ISP). Both the carotid plaque score and the number of plaques/patient in the ITV group were significantly higher than in the VN group. Significant stenosis was observed in 2 patients of the ITV group, but in none of the VN group, indicating carotid atherosclerosis was more advanced in the ITV group (Figure 3).
Figure 3: Carotid Ultrasonographic Results. Intima to media thickness (IMT), plaque score, localization of plaques, and the number of plaques/patient in the idiopathic transient vestibulopathy (ITV) and vestibular neuritis (VN) groups of patients. CCA: common carotid artery. BF: bifurcation of CCA and internal carotid artery (ICA). Total: total number of plaques/patient in ITV and VN groups. p: between ITV and VN groups. n: number of patients.
Plaque Morphology
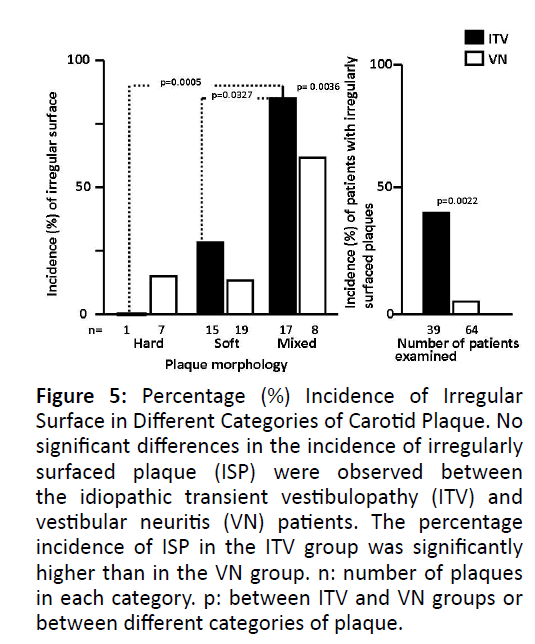
The incidence of plaques was higher in the ITV group, irrespective of the segment of the carotid artery. Soft and mixed plaques were more frequently observed in the ITV than in the VN group. The incidence of mixed plaques and ISP in the ITV group was significantly higher than in the VN group (Figure 4). ISP was observed more frequently in the ITV than in the VN group. ISP was observed more frequently in mixed plaques than in the other categories of plaque. The incidence of patients having ISP was higher in the ITV than in the VN group (Figure 5).
Figure 5: Percentage (%) Incidence of Irregular Surface in Different Categories of Carotid Plaque. No significant differences in the incidence of irregularly surfaced plaque (ISP) were observed between the idiopathic transient vestibulopathy (ITV) and vestibular neuritis (VN) patients. The percentage incidence of ISP in the ITV group was significantly higher than in the VN group. n: number of plaques in each category. p: between ITV and VN groups or between different categories of plaque.
Discussion
Possible Participation of ISP in ITV
By histology, hard plaque is composed mainly of collagen and elastic fibers, which maintain plaque architecture, with scant lipid content and therefore resistant to disruption, whereas soft plaque is composed mainly of rich lipids and scant collagen and elastic fibers and therefore prone to disrupt, and mixed plaque is usually composed of both lipids and collagen and elastic fibers [11]. Among the mixed plaques by ultrasonography, calcium deposits, which are highly echoic, are mixed with lipids and cause the ISP appearance [11,12].
In the present study, the incidence of soft plaque in the ITV group was significantly higher than in the VN group. Although this type of plaque is more vulnerable to disruption, but it does not mean that it is the source of thromboemboli. ISP was more frequently observed in the mixed plaque group in the present study. ISP is a risk factor for ischemic cerebral events [13]. In the present study, the incidence of ISP in ITV patients was significantly higher than in those with VN. In ischemic heart disease, ISP is a feature of so-called complex plaques and represents disruption, ulcer or fissure [14,15]. Thin mural thrombi attached to ISP are frequently detected by percutaneous angioscopy [16] and similarly, ISP represents ulcer, fissure or disruption [17]. Participation of ISP in amaurosis fugax has been reported [18]. Although not visualized by ultrasonography in the present study, there is the possibility of thin mural thrombi on the ISP and that microthrombi detached from the ISP flowed into the arteries that irrigate the vestibulum, causing transient ischemia, leading to vestibular nerve dysfunction and resultant vertigo in ITV patients. Emboli from the heart lodge selectively in the anterior vestibular artery, causing vertigo, nausea, vomiting and postural instability [19].
Reason for High Incidence of ISP in ITV Patients
The higher incidence of mixed plaque, which is a more advanced stage of atherosclerosis, in the ITV group was probably partly because of the higher incidence of hypertension, which is a risk factor for atherosclerosis. The incidence of mixed plaque also showed a tendency to be higher than that of hard or soft plaques in the VN group. When advanced, an ulcer, fissure or disruption frequently occurs not only in coronary but also in carotid plaques that often exhibiting an irregular surface. This was probably the reason for the higher incidence of ISP among the mixed plaques.
Reason for Rapid Recovery of Vertigo in ITV Patients
Severe cerebrovascular events are frequently associated with significant carotid artery stenosis, and symptoms often persist [19,20]. When the microemboli are small and sufficient blood flow is maintained because of the absence of severe carotid stenosis, the emboli are rapidly washed out or lysed, with resultant transient vestibular ischemia, dysfunction and vertigo, and their rapid resolution. This process might be an underlying mechanism of ITV, similar to the rapid recovery from vision loss in patients with amaurosis fugax.
ITV as a Possible Ischemic Cerebrovestibular Event
Carotid plaque participates in transient ischemic attacks [20] and carotid plaque-related amaurosis fugax develops alone or with cerebral events [21-23]. Vestibular dysfunction presenting as vertigo also develops alone or with cerebral events [24]. It is probable that the size of the emboli and blood flow are the determinants of the arteries to be occluded and accordingly the territory of ischemia; small emboli occlude the vestibular artery but those occluding small cerebral arterial branches does not manifest symptoms depending on the irrigating territory, whereas large emboli cannot enter small-diameter arteries such as the vestibular artery and therefore obstruct the larger arteries that irrigate the brain and cause cerebral or cerebellar symptoms; in the case of a mixture of large and small emboli, both cerebral and vestibular arteries are involved and both cerebral or cerebellar symptoms and vertigo may develop.
ITV Patients with Positive Caloric Test
Mild to moderate but not severe vestibular dysfunction was observed in a small number of ITV patients who recovered within 24 hour, possibly because of early performance of the caloric test or a relative delay of recovery from vestibular dysfunction, although involvement of VN could not be denied.
Other Sources of Microemboli
Cerebral events are often associated with heart disease (valvular disease, atrial fibrillation, patent foramen ovale, etc.) [25,26], aortic arch plaques [27], and atherosclerosis or spasm of the intracranial arteries. It remains to be elucidated whether these diseases are the source of thromboemboli in the patients with ITV without ISP in the carotid arterial tree.
Treatment of ITV
VN patients are usually treated with corticosteroids, often with favorable results [28]. In contrast, the present retrospective study suggested the effectiveness of antiplatelet therapy in preventing recurrence in ITV patients.
Study Limitations
Microemboli originating from carotid plaques were strongly suspected as a cause of ITV, but direct evidence that supports microemboli flowing from the ISP into the vestibular artery and occluding it is lacking. By visualizing microemboli flowing through the carotid or cerebral artery, known as “highintensity transient signals [29,30],” whether or not this possibility is true could be determined. The patient populations were not age-matched. Further studies by matching age are required to clarify that ISP is frequent in ITV patients.
Conclusion
The underlying mechanism(s) of vertigo that develops suddenly and subsids within 24 h (i.e., ITV) was examined in 39 consecutive patients, using 64 patients with VN as a control group. Vestibular dysfunction assessed by caloric test was absent or mild in the majority of ITV patients but severe in the majority of VN patients. By carotid ultrasonography, the incidence of ISP, which often represents ulcer, fissure or previous disruption, was high. The results suggested microemboli from these plaques caused transient vestibular nerve ischemia and dysfunction leading to ITV in at least one-third to half of the ITV patients.
References
- Hanley K, O’Dowd T (2002 )Symptoms of vertigo in general practice: a prospective study of diagnosis. Br J Gen Pract52: 309-312.
- Cooper CW (1993) Vestibular neurinitis: a review of a common causes of vertigo in general population. Br J Gen Pract 43:164-167.
- Batuecas-Caletrio A, Yanetz-Gonzalez R,Sanchez-Blanco C, Perez PB,Gonzalez-Sanchez PB, et al. (2015) Glucocorticoids improve acute dizziness symptoms following acute unilateral vestibulopathy. J Neurol262: 2578-2582.
- M Strupp,T Brandt (2009) Vestibular neuritis. SemNeurol 29: 509-519.
- Adams RD (1943) Occlusion of the anterior and inferior cerebellar artery. ArchNeurol Psych 49:765-770.
- Lee H, Kim HA (2013) Nystagmus in SCA territory cerebellar infarction: pattern and a possible mechanism. J NeurolNeurosurg Psychiatry 84:446-445.
- Edlow JA, Newman-Toker D (2016) Using the physical examination to diagnose patients with acute dizziness and vertigo. The Journal Emergency Medicine50: 617-628.
- Feng X, Ye C, Mu Mand Chen H (2014) Correlation analysis on retro bulbar vascular hemodynamic characteristics and carotid artery color Doppler ultrasonographic features of amaurosisfugax. [Zhonghuayankezazhi]Chinese journal of ophthalmology50:421-425.
- Shwarz F, Bayer-Karpinska A, Poppert H, Buchholtz M, Cyran C, et al. (2013) Serial carotic MRI identifies rupture of a vulnerable plaque resulting in amaurosisfugax. Neurology 80:1171-1172.
- Komatuzaki A, Futaki T, Y Harada (1988) Document for diagnosis standardization of the dizziness-Report of diagnostic criteria committee of dizziness on 1987. Equilibrium Research 47: 255-256.
- Y Uchida (2001) Histological basis for interpretation of angioscopic and ultrasonographic (IVUS) images of atherosclerotic coronary plaquesin Coronary angioscopy. Y. Uchida, Ed.,Futura Publishing Ltd, Armonk, NY.pp: 29-41.
- Lee KB, Budoff MJ, Zavodoni A, Polak JF, Jeffrey Carr J et al. (2012) Coronary artery calcium is associated with degree of stenosis and surface irregularity of carotid artery. Atherosclerosis223: 160-165.
- Prabhakaran S,Rundek T, Ramas R,Elkind MS, Paik MC, et al. (2006) Carotid plaque surface irregularity predicts ischemic stroke: the northern Manhattan studyStroke37:2696-2701.
- Ambrose JA, Winters SL, Arora RR, Haft JI, Goldstein J,et al. (1985) Coronary angiographic morphology in myocardial infarction: a link between the pathogenesis of unstable angina and myocardial infarction. J Am CollCardiol6: 1233-1238.
- Stary HC,Chandler AB, Dinsmore RE,Fuster V,Glagov S,et al. (1995) A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis: a report from the Committee on Vascular Lesions of the Council on atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology15: 1512-1531.
- Y Uchida (2001) Clinical classification of atherosclerotic coronary plaques. Coronary angioscopy. Y. Uchida. Ed.Futura Publishing Ltd, Armonk, NY pp: 71-81.
- Chiu B, Beletsky V, Spence JD,Parraga G, Fenster A (2009) Analysis of carotid lumen surface morphology using three-dimensional ultrasound imaging. Physics in Medicine and Biology54: 1149-1167.
- O’Farrell CM,FitzGerald DE (1993) Prognostic value of carotid ultrasound lesion morphology in retinal ischemia: result of a long term follow up. British Journal of Ophthalmology77: 781-784.
- Kim HA, LeeSr, Lee H (2007) Acute peripheral vestibular syndrome of a vascular cause. Journal of the Neurological Sciences254: 99-101.
- Verhoeven B, Hellings WE, Moli FL,de Vries JP, de Kleijn DP,et al. (2005) Carotid atherosclerotic plaques in patients with transient ischemic attacks and stroke have unstable characteristics compared with plaques in asymptomatic and amaurosisfugax patients. Journal of Vascular Surgery42: 1075-1081.
- Feng X,Ye C,Mu M, Chen H (2014) Correlation analysis on retrobulbar vascular hemodynamic characteristics and carotid artery color Doppler ultrasonographic features of amaurosisfugax. ZhonghuayankezazhiChinese journal of ophthalmology 50: 421-425.
- Nicolaides AN, Kakkos SK, Kyriacou E,Griffin M, Sabetai M, et al. (2010) Asymptomatic Carotid Stenosis and Risk of stroke (ACSRS) Study Group: asymptomatic internal carotid artery stenosis and cerebrovascular risk stratification. J VascSurg52:1486-1496.
- Verhoeven B,Hellings WE,Moli FL, de vries JP, de Kleijn DP, et al. (2005) “Carotid atherosclerotic plaques in patients with transient ischemic attacks and stroke have unstable characteristics compared with plaques in asymptomatic and amaurosisfugax patients,” Journal of Vascular Surgery. 42:1075-1081.
- Lee H, Kim HA (2013) Nystagmus in SCA territory cerebellar infarction: pattern and a possible mechanism. Journal of Neurology, Neurosurgery & Psychiatry 8: 446-451.
- Hahne K, Moennig G, Samol A (2016) Atrial fibrillation and silent stroke; link, risks, and challenges. Journal of Vascular Health and Risk Management 12: 65-74.
- Kawada S, Hamaguchi T, Kitayama M, Imamura T, Ohno M, et al. (2015) Multidetector computed tomography angiography to detect the cause of multiple brain infarctions. Journal of Stroke & Cerebrovascular Diseases 24: 348-353.
- 27.Wang B, Sun S, Liu G, Li Y, Zhang L, et al. (2013) Correlation between aortic/carotid atherosclerotic plaques and cerebral infarction. Experimental and Therapeutic Medicine 6: 407-410.
- Goudakos JK, Markou KD, Psillas G, Vital V, Tsaligopouros M (2014) Corticosteroids and vestibular exercises in vestibular neuritis: single-blind randomized clinical trial. JAMA Otolaryngology–Head & Neck Surgery 140: 434-440.
- Orlandi G, Parenti G, Bertolucci A, Puglioli M, Collavoli P, et al. (1997) Carotic plaque features on angiography and asymptomatic cerebral microembolism. ActaNeurologicaScandinavica96: 183-186.
- Koenenecke HC, Mast H, Trocio SH, Sacco RL, Ma W, et al. (1998) Frequency and determinants of microembolic signals on transcranial Doppler in unselected patients with acute carotid territory ischemia: a prospective study. Cerebrovascular Diseases 8: 107-112.