Case Report - Journal of Orthopedic Surgery and Rehabilitation (2018) Volume 2, Issue 1
Periprosthetic, interprosthetic, and refractures after interprosthetic femoral fractures - Extension of the currently used Vancouver, Rorabeck and Platzer classification
- *Corresponding Author:
- Mirko Velickovic
Department of Orthopedic Surgery, Sports
Traumatology and Trauma Surgery, Städtisches Klinikum
Wolfenbüttel ,Wolfenbüttel Municipal Hospital, Germany
Tel: +49 5331 9340
E-mail: mirko.velickovic@gmx.de
Accepted date: May 14th, 2018
Citation: Velickovic M, Hockertz T. Periprosthetic, interprosthetic, and refractures after interprosthetic femoral fractures - Extension of the currently used Vancouver, Rorabeck and Platzer classification. J ortho Rehab Surg. 2018;2(1):1-8
Abstract
As life expectancy of the population increases the number of total hip [THA] and total knee [TKA] arthroplasties are increasing as well. Accordingly, the number of complications and revision surgery will also rise. Periprosthetic femoral fractures are largely classified by the Vancouver classification for periprosthetic fractures of the hip as well as the Rorabeck classification for periprosthetic femur fractures knee. However, the established classification does not cover the whole spectrum of periprosthetic femoral fractures
Keywords
Osteoarthritis, Orthopedic surgery, Periprosthetic fracture, Interprosthetic fracture, Femoral fractures.
Introduction
As life expectancy of the population increases the number of total hip [THA] and total knee [TKA] arthroplasties are increasing as well. The incidence associated with periprosthetic femoral fractures becomes more common. For example in 2011, 286 hip THA and 207 TKA per 100,000 inhabitants were performed in Germany. In an international comparison, Germany thus occupies a leading position. In terms of THA Germany ranks second in Switzerland, and third in TKA after the US and Austria [1] this trend will continue to intensify in the coming years. Accordingly, the number of complications and revision surgery will also increase. Periprosthetic femoral fractures are devastating fractures and a challenging problem for the surgeon. Periprosthetic femoral fractures after THA and TKA are largely classified by the Vancouver as well as the Rorabeck classification. Interprosthetic fractures are widely classified by Platzer. However, the established classification does not cover the whole spectrum of periprosthetic femoral fractures [2].
Etiology, Incidence and Risk Factors
Basically one must distinguish between intraoperative and postoperative occurring periprosthetic fractures. In case of THA, the risk of intraoperative periprosthetic fractures for cemented prostheses is 1%, for cementless prostheses 3-7% [3,4]. The incidence of postoperative periprosthetic fractures varies between 0.4-1.1% for primary THA [5,6]. In revision surgery, the incidence for intraoperatively occurring fractures is approximately 6% of the cemented THA and 17% of the cementless THA [7]. Among the postoperatively occurring fractures, the rate varies between 2.1-24% [5,6,3]. Periprosthetic femoral fractures occur with an average of 7.4 years after primary implantation and 3.9 years after revision surgery [5,8]. The etiology for periprosthetic fractures is multifactorial but there are several predictors. Intraoperative periprosthetic fracture in primary surgery usually occur after reaming of the femur or inserting cementless stems in pressfit technique in a narrow medullary canal. In revision procedures preexisting osteolysis, poor bone quality, complicated hardware removal such as extrication of remaining cement can cause periprosthetic fractures [9]. In general patients with periprosthetic fractures often show a high rate of comorbidities at a higher age. There are several diseases associated with a higher incidence for periprosthetic fractures such as osteoporosis, osteomalacia, brittle bone disease [Osteogenesis Imperfecta], Paget's disease, rheumatic diseases, low bone stock, osteolysis, septic or aseptic loosening of implant [8,10]. There are several risk factors. For example the tip of a loose stem acts as a stress riser, while a well-fixed stem not. Interestingly the gap between two ipsilateral femoral stems does not affect peak tensile stress on the femur [11]. According to Singh et al. there is a U-shaped relationship between age and periprosthetic fracture risk. According to the authors patient under 60 and over 80 years have a 45% higher risk compared to patients in the age group of 71-80 years. They suspected that younger patients have a more active lifestyle with athletic activities and also have a higher corticosteroid use which may lead to steroid-induced osteoporosis [12]. For example the risk of a fracture between an intramedullary nail and a cemented prosthesis is higher than between two cemented prostheses so it is likely that this type of fracture will also increase in the future [13]. In summary the incidence of periprosthetic fractures is multifactorial.
Terminology
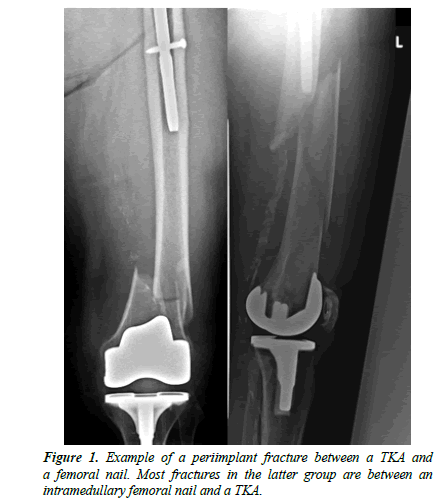
As life expectancy growth the number of total joint replacement increases too. On the other hand more and more patient already has implants due to prior surgeries of the hip or knee. Therefore, a precise definition of fracture morphology is all the more important. Different periprosthetic femoral fractures must be subclassified. Periprosthetic femur fractures are fractures of the femur with adjacent THA or TKA. Interprosthetic femur fractures are fractures of the femur between a THA and a TKA. Periimplant fractures are fractures with one arthroplasty of the hip or knee and one osteosynthesis for example an intramedullary nail (Figure 1).
Classifications
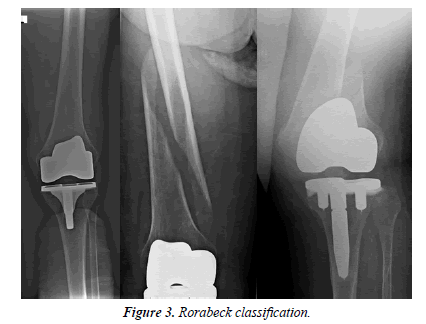
The two most common classifications for femoral periprosthetic fractures are based on the Vancouver classification for periprosthetic femoral fractures of the hip (Figure 2) as well as the Rorabeck classification for the knee (Figure 3). In case of interprosthetic fractures the Platzer classification is widely used.
Vancouver classification
• Type A: Fracture in trochanteric region
A1: Trochanter major.
A2: Trochanter minor.
• Type B: Fracture around stem or just below it
B1: Well-fixed stem.
B2: Loose stem but good proximal bone stock.
B3: Loose stem with poor proximal bone stock.
• Type C: Fracture occurs well below the prosthesis.
Rorabeck classification
Type 1: Stable, non-displaced fracture, well fixed prosthesis.
Type 2: Displaced fracture with a well fixed prosthesis.
Type 3: Loose or failing prosthesis regardless of the fracture displacement.
Platzer classification
Modified the Vancouver classification in order to classify interprosthetic femoral fractures. He distinguished interprosthetic fractures into three types, depending on the fracture site and the vicinity of the prosthesis:
Type I: No adjacency.
Type II: Adjacency to one prosthesis.
Type III: Adjacency to both prostheses.
Extension of the Vancouver, Rorabeck and Platzer classification
While in the past the established classifications have been able to classify the periprosthetic fractures completely, nowadays not all fractures can be classified due to the increase in operations and complications. Fractures with long stem as seen in revision total hip or total knee replacement cannot be classified. Also the refracture after interprosthetic femoral fracture is not classifiable with the established classification. We therefore suggest the following extensions of the established classifications.
Vancouver Type D
Periprosthetic femoral fracture around revision prosthesis of the hip
Rorabeck Typ 3
Periprosthetic femoral fracture with a long stem of the total knee replacement
Platzer Type 4
Refracture after interprosthetic femoral fracture
Case Studies
On the basis of several examples we would like to demonstrate our considerations below:
Case one
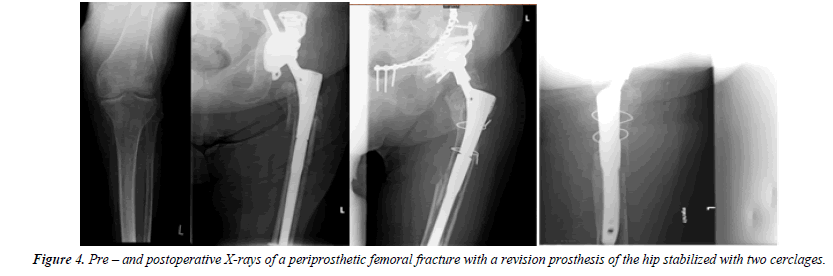
An 88-year-old female fell at home. Several years ago a total hip replacement was changed due to loosening of the prosthesis and revision prosthesis (Prevision Modular Hip Revision Stem - B. Braun-Aesculap, Tuttlingen, Germany) was implanted.
Case two
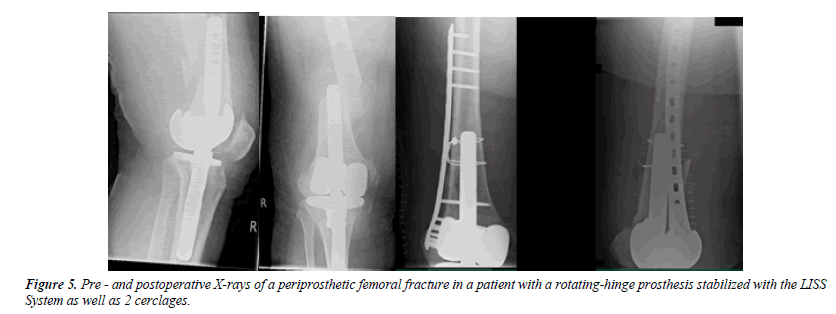
A 77-year-old male fell at night at home. X-rays showing a distal periprosthetic femoral fracture with a rotating-hinge prosthesis (B. Braun-Aesculap, Tuttlingen, Germany).
Case three
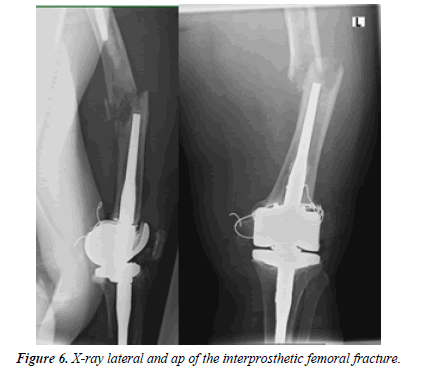
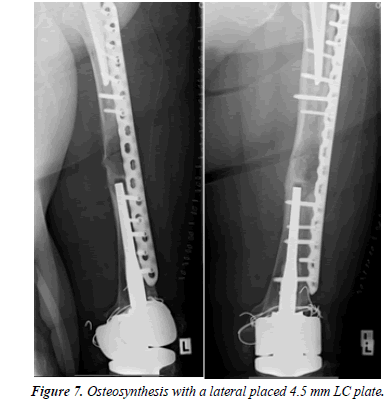
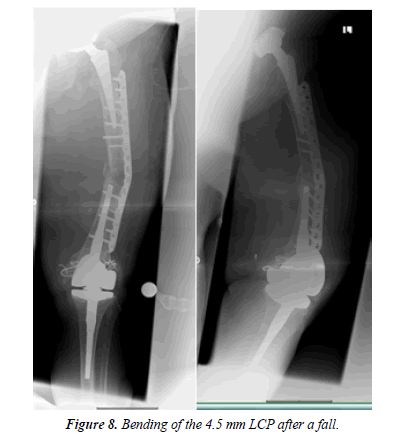
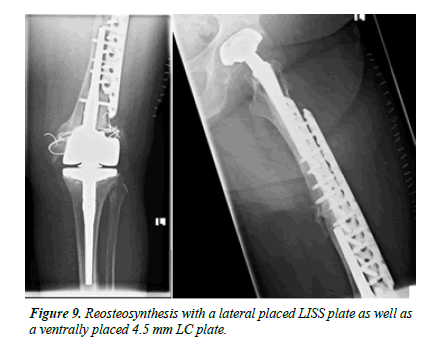
An 88-year-old patient fell at home. Even before the fall, the patient was restricted in her mobility after several revision surgeries of the knee including a change of the TKA due to infection. On x-rays, there was an interprosthetic femoral fracture with several cerclages (Figures 4-6). Although we suspected a loosening of the distal prosthesis, both prostheses were firm. We performed an open reduction and internal fixation with a 16 hole 4.5 mm laterally placed LC plate (Figure 7). We mobilized the patient with full weight-bearing. There were no wound healing disturbances or signs of infections. The patient was discharged in a rehabilitation clinic. 4 weeks after operation the patient fell again due to hypoglycemia. Radiologically, there is a bending of the LC plate of about 40° (Figure 8). The LC plate was removed and replaced by a 16 hole LISS plate together with a 12 hole 4.5 mm LC plate ventrally (Figure 9).
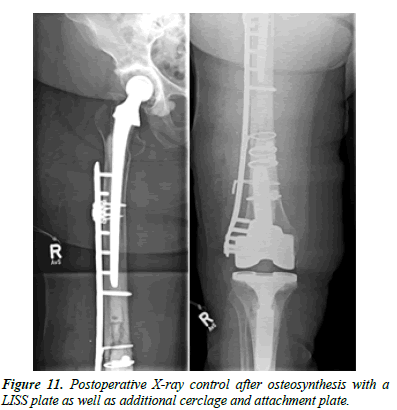
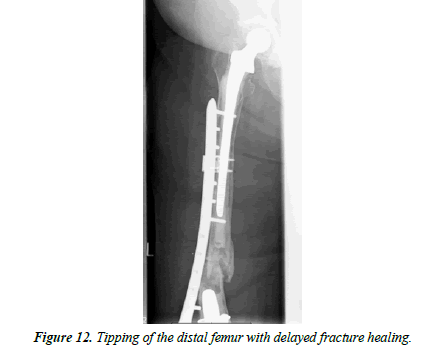
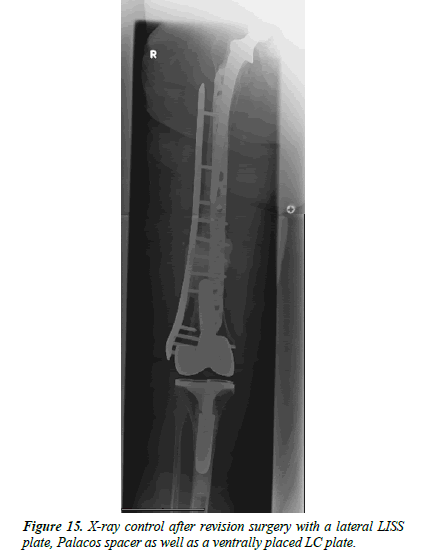
Case four
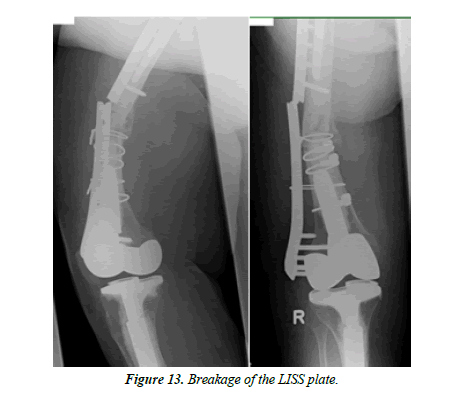
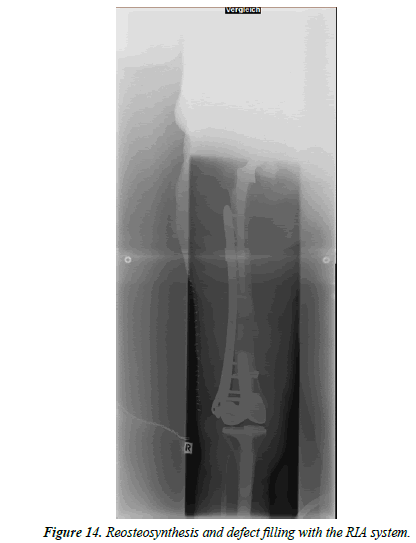
An 86-year-old female patient fell at home. X-rays showed an interprosthetic femoral femur fracture with a TKA as well as revision THA (Figure 10). During primary and revision surgery of the knee, a periprosthetic fracture occurred so cerclages were necessary. The patient was operated with a 13-hole LISS plate as well as 2 × cerclages (1.5 mm steel) and a proximally placed attachment (Figure 11). A proposed partial loadbearing could not be maintained due to incompliance so that we mobilized the patient with full load. The follow up x-rays showed a tipping of the distal femur with delayed fracture healing. Overall, there was extremely poor fracture healing with poor bone quality. (Figure 12) 8 weeks later the patient fell on more time with breakage of the LISS plate (Figure 13) The broken LISS plate as well as the bone cement was removed. We treated the patient with a surgical debridement, together with a reosteosynthesis with a 13 hole LISS plate as well as filling of the defect with cancellous bone graft which was taken from the not affected femur with a Bone Graft Harvesting Set [RIA Reamer-Irrigator- Aspirator] (Figure 14). Partial loadbearing was again not possible. The patient was discharged after completion of wound healing. X-ray controls showed a nonunion. This time the LISS plate was removed and replaced by another angular stable plate together with an additional ventrally placed 4.5 mm LC plate. The central defect was filled with 40 ml of Refobacin Palacos (Figure 15).
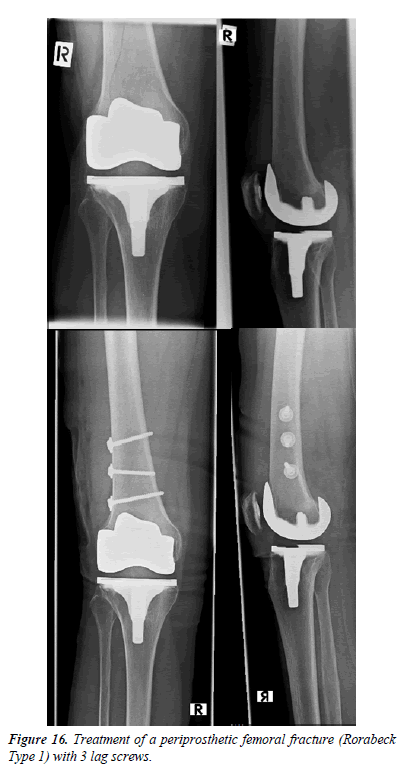
Treatment Options
Patients with peri- and interprosthetic fractures have a high rate of secondary diseases and limited compliance in the overwhelming number of cases. The treatment of these fractures are due to potential poor bone stock, advanced age, potential prosthetic instability/loosening, and limited fracture fixation options both proximally and distally a major challenge. The general complication rate is high. A one-time surgery and definitive procedure should be chosen [14]. The operative strategies for periprosthetic femoral fractures range from minimally invasive procedures to angle stable plate fixation to revision prosthetics. In addition, there are numerous additive processes such as cerclage, attachment plates, bone grafting. In essence, the type of operative treatment depends on whether the prosthesis is still well fixed or has loosened or broken through the fracture. Surgeons have to consider that the bone might be weakened due to minor perfusion by cerclage. Screw holes can act as predetermined breaking points. Periprosthetic femur fractures Type Vancouver A can be treated conservatively up to a dehiscence <2 cm. From 2 cm dehiscence, an osteosynthesis is useful to improve the mobility [15]. Vancouver B 1 fractures are treated with angular stable plate fixation with or without cerclage. Vancouver B 2 fractures always have a loosened prosthesis, which require a change of the prosthesis. In case of poor bone quality and loosened prosthesis [Vancouver B 3], the prosthesis must also be removed [16,17]. Depending on the size of the bone defect, the augmentation of the femur by allogeneic or autologous bone graft appears to be useful [18]. For the therapy of periprosthetic fractures after TKA, various treatment options are available. The conservative therapy of periprosthetic femur fractures after TKA is possible in cases of Rorabeck type I fractures as well as nondislocated fractures without component loosening. The indication for a conservative treatment is in regard of possible accompanying complications like long phase of convalescence muscular atrophy, thrombosis and pneumonia strict. [19,20]. Rorabeck type 2 and 3 are always treated surgically. Similarly to the treatment of periprosthetic fractures of the femur, treatment depends of whether the prosthesis is firm or loose. In the case of a loosened prosthesis, the prosthesis should be changed. In the case of a fixed prosthesis, the fracture can be treated with an osteosynthesis. Additive methods such as cerclage or attachment plates are also available. Intramedullary systems have a higher risk of rotational misconduct and appear to have an increased risk of infection. Further disadvantages of intramedullary systems are that they cannot be used in very distal fractures [21]. The trend is therefore toward angular stable plate fixation. But there are also minimal invasive osteosynthesis possible (Figure 16). Interprosthetic fractures are rare fractures, refractures after angular stable plate fixation of an interprosthetic femoral fracture even more rare. Interprosthetic fractures may occur between two well-fixed implants or between loose implants. It is also conceivable that a previously fixed prosthesis can be loosened by a refracture [22]. In our own patients, we have seen a refracture of an interprosthetic femoral fracture 2 times with well-fixed prostheses in both cases. Treatment of patients with an interprosthetic femoral refracture is more complex and surgically more demanding than of patients with isolated periprosthetic fractures. The therapy of interprosthetic femoral fractures follows similar principles as for periprosthetic femur fractures. In the case of prosthesis loosening, the change of the prosthesis is indicated along with an additional osteosynthesis. Most surgeons prefer a lateral angle stable plate like the LISS System. However, there are also case reports about treatment of periprosthetic femoral fractures with femoral nails. Citak et al. described a series of 4 cases of interprosthetic femoral fractures treated with a custom-made interposition device [23-28]. In the treatment of refractures of interprosthetic femoral fractures we prefer in our own patients the reosteosynthesis with an angular stable plate fixation like the LISS System or lateral LC Plates that span the entire interprosthetic fracture zone to eliminate additional stress risers where the plate is either placed further proximally or distally in order not to occupy the old drill holes [23,24]. Additional procedures such as cerclage wire or a ventral LC plate can be used. In summary we archived satisfactory outcome in our 2 patients. Positioning of the new plate is due to limitations of the proximal and distal prosthesis or osteosynthesis, comorbidities as well as weakened bone stock due to the former femoral drill holes challenging. Platzer et al. described a case of a plate breakage after lateral plate fixation of an interprosthetic femoral fracture 10 months after primary stabilization. The patient finally underwent revision surgery by plate fixation and supplementary bone grafting, and the interprosthetic fracture had healed uneventfully. In our patient collective we perform a reosteosynthesis. In the first operation step, the broken angular stable plate is removed and the fracture area is debrided. The reosteosynthesis is also performed with an angular stable plate from the lateral side. The plate is placed more distally or proximally in order not to use the same screw holes. In addition, a ventral 4.5 mm LCP plate is placed to overbridge the fracture. Nevertheless, in addition to the fracture morphology, the expected patient compliance and secondary diseases must be taken into account, so that the type of care remains an individual decision. Since the total number of total hip and total knee replacement will increase over time, the number of revision prostheses will also increase, so in the future we will more and more see those types of fractures.
Limitations
The central weak point of the extension of the classifications is that no therapeutic recommendation result from this. While the Vancouver and the Rorabeck classification always provide conclusions about the treatment options, for example whether the prosthesis should be changed or an osteosynthesis is sufficient, this is not the case with the new types.
Discussion and Conclusion
Complications after joint replacement are getting more and more frequent. With the current classifications certain periprosthetic femoral fractures as well as interprosthetic femoral refractures cannot be classified so we suggested updating those classifications. Overall, these are rare injuries. There is considerable data concerning epidemiology and treatment of TKA and THA periprosthetic fractures but there are less information regarding interprosthetic fracture management. The large increase in primary implantations of THA and TKA as well as revision procedures, will unavoidable lead to an increasing number of those fractures [25-28]. According to Platzer et al. interprosthetic femoral fractures are more susceptible for delayed union or nonunion than other fractures, so we presume that we will see similar observing after refracture of interprosthetic femoral fractures. As mentioned before the therapy is an individual decision of the surgeon with a limited number of options. A standardized procedure in the treatment of those fractures is so far not known. The extension of the classification is intended to give the surgeon a clue about the injury. More cases have to be analyzed in the future in order to classify the periprosthetic femoral fractures in their totality.
We are convinced that in future we will see even more types of periprosthetic femoral fractures.
Declaration of Conflicting Interests
The author’s declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
Our institutions do not require ethical approval for reporting individual cases or case series.
Funding
The author[s] received no financial support for the research, authorship, and/or publication of this article.
References
- Wengler A, Nimptsch U, Mansky T. Hip and knee replacement in Germany and the USA: Analysis of individual inpatient data from German and US Hospitals for the Years 2005 to 2011. Deutsches Ärzteblatt International. 2014;111:407-6.
- Soenen M, Migaud H, Bonnomet F, et al. Interprosthetic femoral fractures: analysis of 14 cases. Proposal for an additional grade in the Vancouver and SoFCOT classifications. Orthop Traumatol Surg Res. 2011; 97: 693-698.
- Ochs BG, Stöckle U, Gebhard F. Interprosthetic fractures-A challenge of treatment. Eur Orthop Traumatol. 2013; 4: 103-109.
- Von Matthey F, Ruchholtz S, Biberthaler P, et al. Unfallchirurg. 2016;119: 288.
- Ruchholtz S, Tomás J, Gebhard F, et al. Periprosthetic fractures around the knee-the best way of treatment. European Orthopaedics and Traumatology. 2013;4:93-102.
- Hanschen M, Biberthaler P. Risk factors for failure of osteosynthesis after periprosthetic fractures of the knee joint. Orthopade. 2014;43:541-48.
- Chandler HP, Tigges RG. The role of allografts in the treatment of periprosthetic femoral fractures. Instr Course Lect. 1998;47:257-64.
- Ochs B, Stöckle U. Periprothetische Frakturen bei einliegender Hüfttotalendoprothese Trauma Berufskrankh. 2012;14:162.
- Pritchett JW. Fracture of the greater trochanter after hip replacement. Clin Orthop Relat Res. 2001;390:221-226.
- Gruner A, Hockertz T, Reilmann H. Die periprothetische Fraktur – Klassifikation, Management, Therapie. Unfallchirurg. 2004; 107: 35-49.
- Platzer P, Schuster R, Luxl M, et al. Management and outcome of interprosthetic femoral fractures. Injury. 2011;42:1219-25.
- Soenen M, Migaud H, Bonnomet F. Interprosthetic femoral fractures: Analysis of 14 cases. Proposal for an additional grade in the Vancouver and SoFCOT classifications Orthop Traumatol Surg Res. 2011;97:693-698.
- Lehmann W, Rupprecht M, Rücker A, et al. Interprothetische Frakturen am Femur Trauma Berufskrankh. 2012; 14:190.
- Duncan CP, Masri BA. Fractures of the femur after hip replacement. AAOS Instr Course Lect. 1995;44: 293-304.
- Cook RE, Jenkins PJ, Walmsley PJ, et al. Risk factors for periprosthetic fractures of the hip: A survivorship analysis. Clin Orthop Relat Res. 2008;466:1652-56.
- Iesaka K, Kummer FJ, Di Cesare PE. Stress risers between two ipsilateral intramedullary stems: a finite-element and biomechanical analysis. J Arthroplasty. 2005;20:386-91.
- Lindahl H, Malchau H, Herberts P, et al. Peri-prosthetic femoral fractures classification and de-mographics of 1049 periprosthetic femoral fractu-res from the Swedish national hip arthroplasty re-gister. J Arthroplasty. 2005;20:857-65.
- Berry DJ. Epidemiology: Hip and knee. Ort-hop Clin North Am. 1999;30:183-190.
- Tsiridis E, Haddad FS, Gie GA. The management of peri-prosthetic femoral fractures around hip replacements. Injury. 2003;34:95-105.
- Ochs B, Stöckle U. Periprothetische Frakturen bei einliegender Hüfttotalendoprothese.Trauma Berufskrankh. 2012;14:162-170.
- Berend KR, Lombardi AV Jr, Mallory TH, et al. Cerclage wires or cables for the management of intraoperative fracture associated with a cement-less, tapered femoral prosthesis: results at 2-16ye-ars. J Arthroplasty. 2004; 19:17-21.
- Singh JA, Jensen M, Lewallen D. Predictors of periprosthetic fracture after total knee replacement: an analysis of 21,723 cases Acta Orthop. 2013;84:170-177.
- Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007;38:651-54.
- Kenny P, Tice J, Quinlan W. Interprosthetic fracture of femoral shaft. J Arthroplasty. 998;13:361-4.
- Bégué T, Thomazeau H, Adam P, et al. Fractures périprothétiques autour des prothèses du genou et de la hanche. Rev Chir Orthop. 2006;92:S29-96.
- Mamczak CN, Gardner MJ, Bolhofner B, et al. Interprosthetic femoral fractures J Orthop Trauma. 2010;24:740-4.
- Sah AP, Marshall A, Virkus WV, et al. Interprosthetic fractures of the femur: Treatment with a single-locked plate. J Arthroplasty. 2010;25:280-6.
- Citak M, Klatte TO, Kendoff D, et al. Treatment of interprosthetic femoral fractures with interposition prosthesis: A technical note. Acta Orthop. 2013;84: 326-27.