Research Article - Journal of Nutrition and Human Health (2020) Volume 4, Issue 1
Performance of MUAC and associated factors in the prediction of acute malnutrition among children 6-59 months at Mulago hospital, Kampala
Sendaula E1*, Joan Kalyango1, Gloria Adobea Odei Obeng1, Nicolette Nabukeera-Barungi2, Denis Opio1, Elizabeth Katana Babirye1, Paul Okimat1, Brenda Nakafeero1, Tobius Mutabazi1, Peterson Kato Kikomeko3, Charles A.S. Karamagi1,2
1Clinical Epidemiology Unit, Makerere University, P.O. Box-7072, Kampala, Uganda
2Department of Paediatrics and Child Health, Makerere University, P.O. Box-7072, Kampala, Uganda
3Department of Human Nutrition and Home Economics, Kyambogo University Emmanuel. P.O. Box 1, Kyambogo, Kampala Uganda
- *Corresponding Author:
- Sendaula Emmanuel
College of Health Sciences
Clinical Epidemiology Unit
Makerere University, P.O. Box 7072, Kampala, Uganda
Tel: +256775806146, +256701806146
E-mail: emmasendaula@gmail.com
Accepted date: May 26, 2020
Citation: Sendaula E, Kalyango J, Obeng GAO, Nabukeera-Barungi N, Opio D, et al. Performance of MUAC and associated factors in the prediction of acute malnutrition among children 6-59 months at Mulago Hospital, Kampala. 2020;4(1):1-7
Abstract
Background: Malnutrition remains a worldwide challenge and accounts for about 35% of all deaths among children under 5 years in the world. To address the burden of acute malnutrition, weight-for-height (WHZ) and Mid-Upper Arm Circumference (MUAC) have been used for acute malnutrition case definition in children. However, these anthropometric indices/indicators correlate poorly and, in some cases, differ in application. We determined the performance of MUAC and its associated factors in the prediction of acute malnutrition among children aged 6-59 months admitted to the pediatric assessment center in Mulago Referral Hospital, Uganda.
Methods: We conducted a cross-sectional study between January and March 2018 among children admitted to the Pediatric Assessment Center of Mulago National Referral Hospital. The study involved 389 children aged 6-59 months from whom demographics and health information were obtained. All eligible participants were selected using systematic random sampling. We conducted descriptive ROC and sensitivity analysis. STATA version 13.0 was used to execute statistical tests for association using the modified poison model.
Conclusion: MUAC had poor performance characteristics at a cutoff of 12.5 cm. MUAC had excellent and similar intra/ inter-observer variability making it a suitable tool for a single user. The optimal cut off-of 13.6 improved the sensitivity. This might be a better cut-off as it has a higher sensitivity and will, therefore, detect a majority of those with malnutrition and yield better results. Age greater than 24 months is associated with a decrease in MUAC performance whilst Anemia, Down syndrome and hair changes are associated with an increase in MUAC performance.
Keywords
Malnutrition; Wasting; Sensitivity; Specificity; Predictive Value; Reliability; Mid-Upper Arm Circumference
Abbreviations
CCTC: Community Therapeutic Care, BMI: Body Mass Index, FANTA: Food and Nutrition Technical, Assistance III Project, H/A: Height-for-Age, HSDP: Health, Sector Development Plan, IMAM: Integrated Management of Acute Malnutrition, MAM: Moderate Acute Malnutrition
MoH: Ministry of Health, MUAC: Mid-Upper Arm, Circumference, NPV: Negative Predictive Value, PPV: Positive Predictive Value, SAM: Severe Acute Malnutrition, UDHS: Uganda Demographic Health Survey, UNICEF: United Nations Children’s Fund, USAID: U.S. Agency for International Development, W/A: Weight-for-Age, WFL: Weight for Length, WFL/H: Weight for Length/ Height, W/H: Weight-for-Height, WHO: World Health Organization, WHZ: Weight for Height Z
Introduction
Children are most vulnerable to malnutrition in developing countries because of low dietary intake, lack of appropriate care, and inequitable distribution of food within the household. In 2016 globally, 52 million children under 5 were wasted and 17 million were severely wasted. This translates into a prevalence of 7.7% and 2.5%, respectively. In 2016, more than half of all wasted children lived in South Asia and about one quarter in sub-Saharan Africa, with similar proportions for severely wasted children [1]. Overall, in Uganda, 4% of children are wasted and 1 percent is severely wasted with Karamoja and West Nile sub-regions having the highest percentages of children who are wasted at 10% [2].
Different methods of nutritional assessment have been used and varied by the type of health facility or service contact points in Uganda. A comprehensive nutritional assessment encompasses dietary, clinical, anthropometric, and biochemical measurements. The World Health Organization recommends WHZ anthropometry for diagnosis of acute malnutrition among children aged 0 to 60 months however many patients are missed by WHZ scores in developing countries because of its practical application [3]. In children aged 6 to 60 months, unadjusted MUAC is also recommended [4].
The prevalence of acute malnutrition in children is used internationally to define the risk of mortality and level of nutritional burden in a population. However, in practice, there is an inconsistency between the prevalence of children identified as malnourished by WHZ and by MUAC. Such ambiguity will result in divergent perceptions of the severity of a population’s nutritional status and the interventions required would depend upon which indicator is chosen to estimate the prevalence of malnutrition, thus causing confusion amongst policymakers about the appropriate criterion and intervention. On one hand, a strategy where the diagnosis can be based on either indicator, as recommended by some may unduly inflate the cost and workload of nutritional programmes whilst preventing few additional deaths and morbidity [4-6].
Early identification of malnutrition is critical and requires urgent medical and nutritional support. There is a need to use simpler methods with acceptable known performance even in hospital settings. MUAC is often preferred as a quick and easy measuring tool in many settings, therefore information about the performance of MUAC is vital especially in referral and emergency settings to adequately estimate, plan, monitor and evaluate nutritional data in regards to children.
For reliable performance, it is also crucial to understand the factors that affect the performance of MUAC. Furthermore, most interventions are aimed at mediating causal factors, it is therefore important to understand the early prediction of malnutrition by the use of MUAC to reduce the risk of morbidity and mortality. The widespread use of MUAC has brought enormous benefits in terms of coverage and efficiency of programs. However, using MUAC because of its assumed simplicity and convenience raises some concerns of validity. A convenient tool must have a fair level of precision and accuracy.
Methods
The study was carried at the Pediatric Assessment Centre of Mulago national referral hospital. A total of 389 participants were eligible and had consented to be included in the study using systematic random sampling. Modified Kish Leslie for diagnostic tests was used to determine the sample size (1965). The outcome variable was the performance of MUAC at a cutoff of 12.5 cm which was quantified using sensitivity, specificity, predictive values, and percentage agreement. The WHZ indicator has become the accepted ‘gold-standard’ anthropometric indicator for acute malnutrition and therefore was the gold standard in this study [7]. Detailed questionnaires were developed, tested, standardized and modified to gather socio-demographic, anthropometric and clinical information.
Basic anthropometry was performed on children aged 6–59 months by measuring weight, height/length, and MUAC. Presence of edema was determined as it interferes with the accuracy of anthropometric measurements. Social-demographic characteristics were reported by the caregiver.
Data was analyzed using STATA version 13.0. Normally distributed data was summarized using mean and median while skewed data was summarized using medians and ranges. Anthropometric z-scores for weight and height data were calculated against the 2006 newer standards World Health Organization (WHO) growth standards for children using the "z-score 06" and "zanthro" anthropometric add-on modules available for Stata. Sensitivity, specificity, predictive values, and likelihood estimates were also calculated. Differences in mean anthropometric z-score by gender were analyzed using the two-sample independent t-test. Comparison of mean W/H versus MUAC z-score within each gender was analyzed using the paired t-test. The overall prevalence of malnutrition was estimated for each index and compared using a Kappa statistic. The modified poison model with robust standard errors was used to determine factors affecting the performance of MUAC in predicting Acute Malnutrition where the outcome (diagnosis) was coded as “1” for misclassification and “0” for correct classification. The questionnaires were translated to Luganda which is widely spoken and commonly understood by the study population and pretested Standard Operating Procedures were adopted and followed to minimize errors in the measurements and all equipment were calibrated before use.
Results
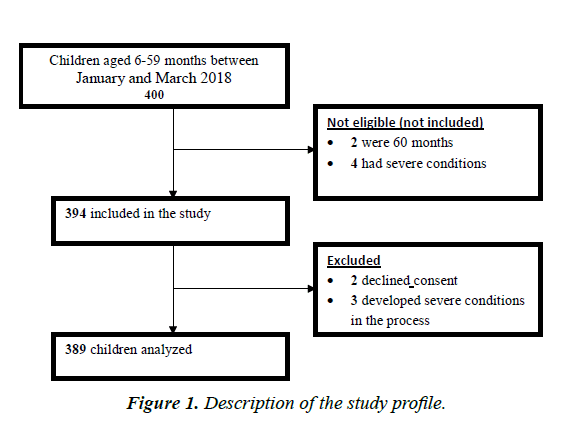
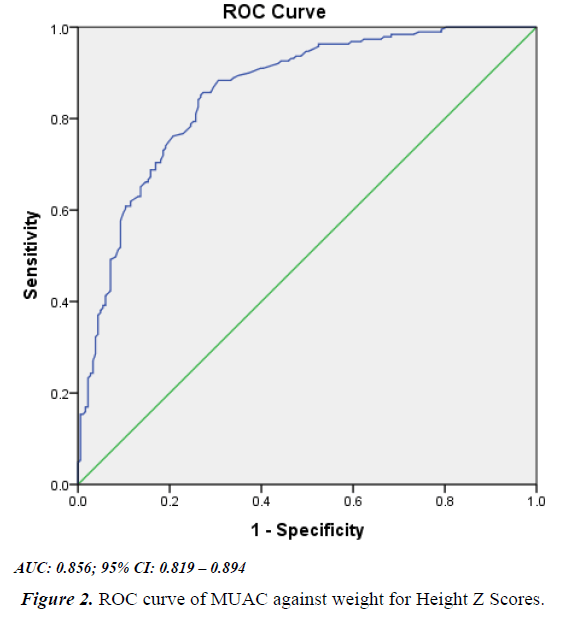
Majority of the study participants were males (60.7%) and the median age was 15, (IQR 9–26) months, Acute malnutrition was assessed using both MUAC (25.27%) and WHZ (49.2%) scores, MUAC sensitivity was 47.5%, specificity was 96.3% at 12.5 cm, optimal cutoff was 13.6 cm (Sensitivity 74% Specificity 81%) ROC AUC 0.856; 95% CI: 0.819 – 0.894. The gold standard in this study was WHZ. The PPV obtained was 92.6% and the NPV was 65.47%. MUAC kappa for intra-observer variability was 0.898 and 0.945 with an inter-observer variability of 0.9323. Similarly, WHZ kappa for intraobserver variability was 0.9788 and 0.9626 with an Inter-observer variability of 0.9516. At multivariate analysis, Age (P=0.019), Anemia (P=0.037), Down syndrome (P=0.004) and hair changes (P=0.023) were found to be significant. A total of 389 children aged 6-59 months were screened as showed in Figure 1.
MUAC at a cutoff of 12.5 cm had poor performance characteristics; we recommend a cutoff of 13.6 cm in screening, referral and admission for acute malnutrition in children 6-59 months in referral hospitals and similar settings. Age greater than 24 months was associated with a decrease in the performance MUAC whilst Anemia, Down syndrome and hair changes were associated with an increase in the performance of MUAC (Figure 1). Majority of the study participants were males 236 (60.7%) and the median age of study participant was 15 months with 194 (49.87%) of them belonging to the age group 6-14 years. The average birth weight was 3 kilograms (IQR 2.7- 3.5) as shown in Table 1.
| Characteristics | Frequency (n) | Percentage (%) |
|---|---|---|
| Age category (months) | ||
| 6-23 | 282 | 72.5 |
| 24-59 | 107 | 27.5 |
| Sex | ||
| Male | 236 | 60.7 |
| Female | 153 | 39.3 |
| Birth weight (kg)* | ||
| ≤ 2.5 | 77 | 19.8 |
| 2.6 – 6 | 287 | 73.8 |
| Caretaker’s education level | ||
| No formal education | 83 | 21.3 |
| Primary | 67 | 17.2 |
| Secondary | 202 | 51.9 |
| Tertiary | 37 | 9.5 |
Table 1. Social-demographic characteristics of the 389 study participants included in the study.
Health status of the participants
Approximately 2% of the participants had birth defects, most of the children were diagnosed or had signs of malaria 44 (11.3%). majority of the study participants 180 (52.8%) were still breastfeeding as shown in Table 2.
| Variables | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Down syndrome | No | 378 | 97.2 |
| Yes | 11 | 2.83 | |
| Heart Defect | No | 380 | 97.7 |
| Yes | 9 | 2.31 | |
| Hair changes | No | 347 | 89.2 |
| Yes | 42 | 10.8 | |
| Mother’s HIV Status* | Negative | 326 | 86.7 |
| Positive | 50 | 13.3 | |
| Child PCR status | Negative | 122 | 31.4 |
| Positive | 6 | 1.5 | |
| Not specified | 261 | 67.1 | |
| Malaria | No | 345 | 88.7 |
| Yes | 44 | 11.3 | |
| Sickle cell Anaemia | No | 354 | 91.0 |
| Yes | 35 | 9.0 | |
| Diarrhoea | No | 370 | 95.1 |
| Yes | 19 | 4.9 | |
| Anaemia | No | 379 | 97.4 |
| Yes | 10 | 2.6 | |
| Breastfeeding* | No | 161 | 47.2 |
| Yes | 180 | 52.8 |
Table 2. Heath status of the study participants included in the study.
Performance of MUAC
Validity performance
The prevalence obtained by WHZ was 49.2%, MUAC sensitivity and specificity was 47.5% and 96.3% respectively as shown in Table 3. From Figure 2, the optimal cut off obtained from the plotted ROC curve was 13.6 cm with a sensitivity of 74% and specificity of 81%.
| Performance | Percentage | CI | |
|---|---|---|---|
| Sensitivity | Pr (+| D) | 47.5% | 40.1% 55.0% |
| Specificity | Pr (-|~D) | 96.3% | 92.5% 98.5% |
| PPV | Pr (D| +) | 92.6% | 85.3% 97.0% |
| NPV | Pr (~D| -) | 65.5% | 59.6% 71.1% |
| Prevalence | Pr (D) | 49.2% | 44.0% 54.4% |
Table 3. Results on the performance of MUAC.
Performance of MUAC adjusted for age
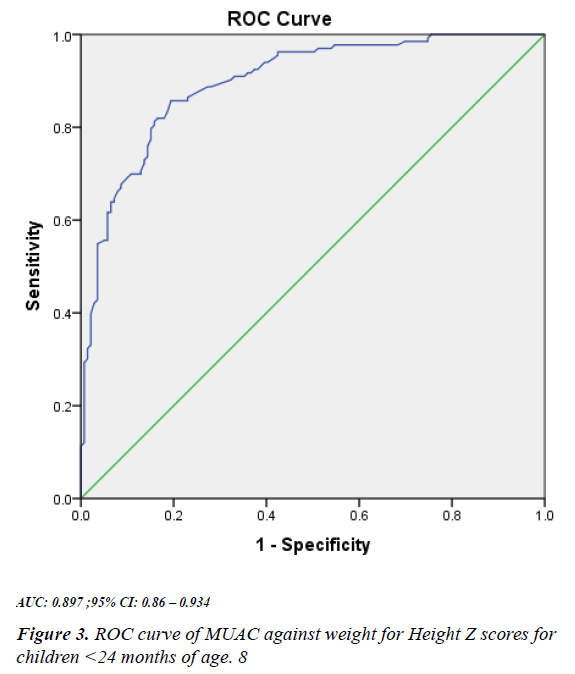
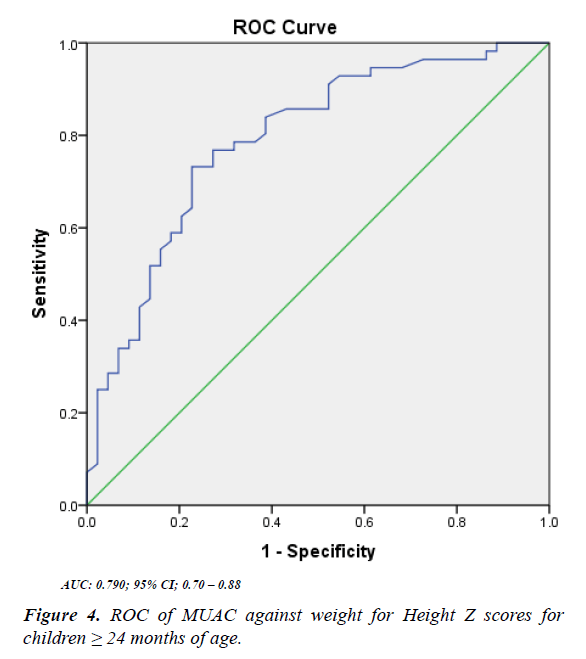
When we adjusted for age, the sensitivity increased to 62% in the age category 6-23 months and decreased to 25% in the age category 24-59 months. The specificity increased from 94% in the age category 6-23 months and 98% in the age category 24 -59 months (Figure 3). The optimal cut off obtained from the plotted ROC curve as shown in Figure 3 was 13.9 cm w ith a sensitivity of 62% and specificity of 94% (Figure 4). Similarly, the optimal cut off obtained from the plotted ROC curve as shown in Figure 4 was 15.6 cm with sensitivity s of 25% and specificity of 98%.
Reliability performance
The observers for the inter and intra-observer assessment were two trained nurses. Double measurements were taken for each participant. The MUAC kappa for intraobserver variability for observer one and two was 0.898 and 0.9451 respectively with an Inter-observer variability of 0.9323 The MUAC kappas for intraobserver variability for observer one and two was 0.898 and 0.9451 respectively with an Inter-observer variability of 0.9323. Similarly, the WHZ scores kappa for intraobserver variability for observer one and two was 0.9788and 0.9626 respectively with an Inter-observer variability of 0.9516.
Factors associated with the performance of MUAC
Multivariate analysis
At multivariate analysis, age, anemia, Down syndrome and hair changes were found to be significantly associated with the performance of MUAC as shown in Tables 4-7. Interaction and confounding assessments were done, in which no interaction was significant and there was no confounding.
| Variables | Frequency | PR* | 95% CI | P-value |
|---|---|---|---|---|
| Age category (months) | ||||
| 6-23 | 282 | 1.00 | 0.65- 0.93 | 0.011 |
| 24-59 | 107 | 0.80 | ||
| Sex | ||||
| Male | 236 | 1.00 | ||
| Female | 153 | 1.08 | 0.96 -1.23 | 0.196 |
| Birth weight | ||||
| ≤ 2.5 | 77 | 1.00 | ||
| 2.6-6 | 287 | 1.10 | 0.92 -1.32 | 0.291 |
| Caretaker’s Education Level | ||||
| No formal education | 83 | 1.00 | -- | -- |
| Primary | 67 | 0.89 | 0.73 -1.11 | 0.318 |
| Ordinary | 202 | 0.91 | 0.78 -1.06 | 0.211 |
| Tertiary | 37 | 1.05 | 0.86 -1.29 | 0.567 |
Table 4. Unadjusted analysis the Social-demographic factors associated with the performance of MUAC.
| Variables | Frequency | PR* | 95% CI | P-value |
|---|---|---|---|---|
| Child PCR status | ||||
| Negative | 122 | 1.00 | 1.24-1.56 | 0.000 |
| Positive | 6 | 1.40 | ||
| Not specified | 261 | 0.99 | 0.87-1.15 | 0.987 |
| Malaria | ||||
| No | 345 | 1.00 | 0.78-1.19 | 0.733 |
| Yes | 44 | 0.96 | ||
| Mother’s HIV status | ||||
| Negative | 326 | 1.00 | 0.95 -1.31 | 0.187 |
| Positive | 50 | 1.12 | ||
| Sickle cells | ||||
| No | 354 | 1.00 | 0.56 -1.03 | 0.077 |
| Yes | 35 | 0.76 | ||
| Anaemia | ||||
| No | 379 | 1.00 | 1.01 -1.56 | 0.038 |
| Yes | 10 | 1.26 | ||
| Down syndrome | ||||
| No | 378 | 1.00 | 1.04 -1.55 | 0.017 |
| Yes | 11 | 1.27 | ||
| Hair changes | ||||
| No | 380 | 1.00 | 1.04 -1.40 | 0.013 |
| Yes | 9 | 1.21 | ||
| Heart Defect | ||||
| No | 380 | 1.00 | 0.43-1.38 | 0.377 |
| Yes | 9 | 0.78 | ||
| Breastfeeding | ||||
| No | 161 | 1.00 | 0.92-1.21 | 0.389 |
| Yes | 180 | 1.06 | ||
Table 5. Unadjusted analysis for the health factors associated with the performance of MUAC.
| Variables | frequency | PR* | 95% CI | P-value |
|---|---|---|---|---|
| Age | ||||
| 6-23 | 282 | 1.00 | 0.69 - 0.97 | 0.019 |
| 24-59 | 107 | 0.82 | ||
| Anaemia | ||||
| No | 379 | 1.00 | 1.02 - 1.62 | 0.037 |
| Yes | 10 | 1.28 | ||
| Down syndrome | ||||
| No | 378 | 1.00 | 1.09 - 1.57 | 0.004 |
| Yes | 11 | 1.31 | ||
| Hair changes | ||||
| No | 347 | 1.00 | 1.02 - 1.39 | 0.023 |
| Yes | 42 | 1.19 | ||
Table 6. Multivariate analysis for the factors associated with the performance of MUAC.
Discussion
Performance of MUAC
Generally, the prevalence of malnutrition was high, it was found to be higher with WHZ (49.2%) compared to that measured by MUAC (25.27%). This is because Mulago hospital is a referral setting with a high possibility of capturing the very sick population who are likely to be malnourished. Furthermore, malnutrition has been found to predispose children to sickness but also those who are sick are likely to get acute malnutrition. The difference in the prevalence between MUAC and WHZ results from the nature of each parameter. WHZ does not account for nutrient stores and body composition but rather determines malnutrition through comparison of weight for height with a reference population. MUAC is directly related to muscle mass and therefore gives us some idea about body composition thus a better predictor of Mortality.
At a MUAC cut-off of 12.5 cm, the prevalence of acute malnutrition was higher in children less than 24 months (32.3%) and low in children ≥ 24 months (9.4%) this is because of a single MUAC cut-off used for the two groups which does not entirely account for older children. this further translated into a lower overall sensitivity for MUAC with increasing age. Mulago hospital has been using two-stage criteria for assessment of acute malnutrition, MUAC has been used for referrals whilst WHZ for admission purposes. The use of an adequate sensitive MUAC (i.e., a MUAC threshold likely to identify all or almost all persons meeting the W/H-based referral criteria) results in many patients being referred for care who are then refused treatment because they do not meet the W/H-based admission criteria as reported by Myatt et al. this raises a concern of rejected referrals. In some programs, the problem of rejected referrals was solved by moving toward a unified MUAC-based referral and admission criterion [8]. Sackett and Holland recommended that an appropriate screening tool in referral clinical settings must be, high predictive value, high objectivity, a high degree of accuracy, reliability and highly specific to prevent referral rejections [9].
MUAC performed poorly with a sensitivity of 47.5% and a specificity of 96.3% PPV (92.6%) NPV (65.5%) at a cutoff <12.5 similar to study carried out in Urban Nigeria 2012 on Reliability of the MUAC among Children Aged 12-59 months with a sensitivity of 20% and specificity of 95.3%. The optimal cut off of 13.6 cm obtained from our study yielded a better sensitivity of 74% and specificity of 81%.
The validity of the MUAC
Both MUAC and WHZ had an excellent agreement beyond chance for inter and intraobserver agreement. The Cohen’s kappa coefficients for WHZ were slightly higher than those of MUAC. Therefore, the reproducibility of the study findings is reliable. The MUAC intra and Intraobserver variability were excellent.
Factors associated with the performance of MUAC
This study further identified MUAC performance anthropometric predictors in children. Age was one the factors found to be significantly associated with the performance of MUAC at 12.5 cm where children aged between 6-23 months were 0.79 times less likely to predict a correct diagnosis by MUAC compared to those aged 24-59 months. A cross-sectional study on MUAC-forage usefulness among children 6–59 months of age in Somalia 2016 showed similar results that the age of the child affected the likelihood of the right diagnosis for acute malnutrition. Children aged 24 months and above had an OR = 0.14 95% (CI; 0.13–0.1, n =858) compared to children less than 24 month [10].
Children with Down syndrome were 1.31 times more likely to predict a correct diagnosis by MUAC compared to those without. A study carried out in the USA in 2015 to evaluate the predictive performance of various methods for weight estimation strategies concluded that MUAC was the best option for weight estimation in children with Down syndrome [11]. However further studies are required to further understand the relationship between Down syndrome and MUAC performance.
According to a study by Myatt et al. WHZ-based indicators are poor at detecting cases of kwashiorkor because the retained fluid weight that tends to mask what would otherwise be low WHZ values. Berkley et al. reported that MUAC used alone performed better than WHZ used alone in identifying children with bipedal edema, skin and hair changes associated with kwashiorkor in Kenya. In our study children with hair changes were found to be 1.18 times more likely to predict a correct diagnosis by MUAC compared to those without hair changes. Acute malnutrition distorts protein synthesis in the hair, therefore hair changes are used by health workers for early diagnosis of childhood malnutrition.
In severe malnutrition, the cause of congestive heart failure is due to an inability to adapt to fluid and electrolyte imbalances which may be due to diarrhoea, severe anaemia, and dehydration. This is usually accompanied by loss of tissue which is directly captured by MUAC increasing the possibility for a correct diagnosis. In our study children with Anemia were found to be 1.25 times more likely to predict a correct diagnosis by MUAC compared to those without anemia.
Conclusion
MUAC had poor performance characteristics at a cutoff of 12.5 cm. MUAC had excellent and similar intra/ inter-observer variability making it a suitable tool for a single user. The optimal cut off-of 13.6 improved the sensitivity. This might be a better cut-off as it has a higher sensitivity and will, therefore, detect a majority of those with malnutrition and yield better results. Age greater than 24 months is associated with a decrease in MUAC performance whilst Anemia, Down syndrome and hair changes are associated with an increase in MUAC performance.
Recommendations
MUAC at a cut-off of 12.5 cm has a low sensitivity, a cut-off of 13.6 cm is recommended for adoption in screening, referral, and admission for acute malnutrition in children 6-59 months in referral hospital settings and similar areas. We recommend the use of two or more assessors (health workers) in the assessment of malnutrition using WHZ.
Acknowledgments
We wish to acknowledge Makerere University Clinical Epidemiology Unit and Mulago Hospital for their supportive role. The authors acknowledge Dr. Sabrina Kitaka for her input into the area of Child Health.
Ethics Approval and Consent to Participate
Permission to proceed with the study was sought from the Clinical Epidemiology Unit, College of Health Sciences Makerere University and Mulago Hospital. Institutional ethical approval was sought from the Makerere University School of Medicine Research and Ethics Committee and Uganda National Council for Science and Technology. All parents or caregivers were asked to consent before allowing their children to participate in the study after explaining the purpose of the study, the duration, study procedures, benefits and risks to them. Confidentiality of participant information was ensured by using participant identification numbers. Children found with malnutrition were forwarded to Health care providers in charge of treatment and referral to the Acute Care Clinic.
Consent for Publication
Not applicable.
Availability of Data and Materials
The datasets will be available on request. Please contact the corresponding author for further information.
Competing Interests
The authors declare that they have no competing interests.
Funding
Not applicable
Authors' Contributions
Emmanuel Sendaula participated in the conception, design, and implementation of the study, statistical analysis, interpretation, and drafting of the manuscript. Charles AS Karamagiparticipated in the study conception and design of the study. Gloria Odeiplanned the study, contributed tothe analysis and reviewed the manuscript. Joan Kalyango planned the study, contributed to the analysis and reviewed the manuscript. Nicolette Barungi planned the study, contributed tothe analysis and reviewed the manuscript. Denis Opio planned the study, contributed to the analysis and reviewed the manuscript. Elizabeth Katana Babirye planned the study, contributed to the analysis and reviewed the manuscript. Paul Okimat planned the study, contributed to the analysis and reviewed the manuscript. Brenda Nakafeero planned the study, contributed tothe analysis and reviewed the manuscript. TobiusMutabazi planned the study, contributed to the analysis and reviewed the manuscript. Charles Karamagiconceptualized, planned and supervised the study, interpreted results and reviewed the manuscript. All authors read and approved the final manuscript.
References
- Berkley J, Mwangi I, Griffiths K, et al. Assessment of severe malnutrition among hospitalized children in rural Kenya: comparison of weight for height and mid-upper arm circumference. JAMA. 2005; 294(5):591–7.
- Legason ID, Dricile R. Prevalence of acute malnutrition among children ages 6-59 months: Results from a baseline nutrition survey in North-Western Uganda. J Nutr Hum Health. 2018; 2(1).
- Akugizibwe R, Kasolo J, Makubuya DB, et al. Missed opportunities in the diagnosis and management of protein-energy malnutrition among children under 5 years in Wakiso district, Uganda. J Public Health Epidemiol. 2013;5(11):463–70.
- WHO & UNICEF. WHO child growth standards and the identification of severe acute malnutrition in infants and children [Internet]. 2009 [cited 2017 Oct 20]. Available from: http://www.who.int/nutrition/publications/severemalnutrition/9789241598163_eng.pdf
- Laillou A, Prak S, De Groot R, et al. Optimal Screening of Children with Acute Malnutrition Requires a Change in Current WHO Guidelines as MUAC and WHZ Identify Different Patient Groups. PLoS One. 2014; 9(7).
- Grellety E, Golden MH. Weight-for-height and mid-upper-arm circumference should be used independently to diagnose acute malnutrition policy implications. BMC Nutr. 2016; 2(1):10.
- Marshall SK, Monárrez-Espino J, Eriksson A. Performance of mid-upper arm circumference to diagnose acute malnutrition in a cross-sectional community-based sample of children aged 6–24 months in Niger. Nutr Res Pract. 2019 ;(3):247–55.
- Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr Bull. 2006;27(3):7–23.
- Sackett DL, Holland WW. Controversy in the detection of disease. 1975; 2(7): 357-359.
- Custodio E, Martin-Cañavate R, Di Marcantonio F, et al. MUAC-for-age more useful than absolute MUAC for nutritional surveillance in Somalia: Results from nineteen cross-sectional surveys (2007–2016). BMC Nutr. 2018;4(1).
- Talib NJ, Rahm G, Abdel-Rahman SM. Estimating weight in children with Down syndrome. Glob Pediatr Health. 2015; 2: 1.