Research Article - Journal of Dermatology Research and Skin Care (2019) Volume 3, Issue 1
Pediatric syphilis: A five-year experience in a single centre
- *Corresponding Author:
- Rolotti MF
Department of Dermatology, Pediatric Tertiary Care Hospital, Argentina
Tel: 0054-0221-4535901 (1504)
E-mail: mariafernandarolotti@hotmail.com
Accepted date: December 13, 2018
Citation: Rolotti MF, Molina LT, Garone A, et al. Pediatric syphilis: A five-year experience in a single centre. Dermatol Res Skin Care. 2018;2(1):12-17.
Keywords
Pediatric syphilis, Syphilis lesions, Plane condylomas, Sexually transmitted diseases.
Introduction
Acquired syphilis
Primary syphilis starts at the Treponema inoculation site after an incubation period of 10-90 days. It is characterised by a deep red macule growing into an ulcerative papule. A chancre is produced [1-6] affecting regional lymph nodes within the first week. Oral chancres are very frequent but are underestimated [7].
Secondary syphilis first symptoms appear within the 6 first postinfection weeks [7]. The secondary stage generally develops after 2-12 weeks [6]. About 80-95% of cases presents with mucocutaneous manifestations [7]. However, any organ or system can be affected since syphilis is a systemic disease [7]. Patients may show loss of appetite, fever, headache, stiff neck, lachrymation, myalgias and arthralgias [6].
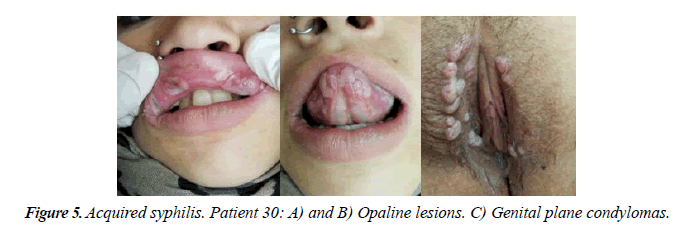
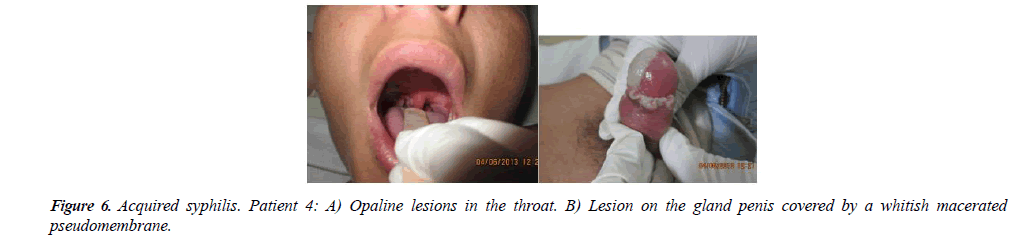
Diagnosis can be generally made through identifying follicular urticarial and infiltrated papules or psoriasis and eczema-like plaques [1]. Nodules and pustules are infrequent [6]. Lesions are widely located but they mostly appear on palms and soles. Moist vegetant lesions called plane condylomas are also found on genitals and rubbing areas [1]. Oral mucosal plaques consist of painless round surface eroded lesions showing grayish scales covered with a whitish pseudo-membrane (opaline lesions) [8]. Moist mucocutaneous lesions are contagious since they contain treponemes. Generalized lymphadenopathies can also be seen [7]. Due to this varied presentation, syphilis is called The Great Pretender [1].
Alopecia can be the only sign of secondary syphilis and has been reported as patchy, diffuse or both in 3-7% of patients. It most often manifests as small irregular patches of non-scarring hair loss around the cranial vault mainly in the occipital and parietal regions. Eyebrows, bear and other hairy areas may also be involved [6,9].
In about 5% of the patients, there may be neurological (early neurosyphilis), ophthalmological (uveitis, retinitis and optic neuritis) and vestibular involvement.
Asymptomatic infection is referred to as early latent syphilis (when detected within the first year after infection) or late latent syphilis (when found after the first post-infection year or its duration is unknown) [7].
Tertiary syphilis is the most destructive stage but is rare nowadays [7]. It presents with two types of lesions. Tubercles are solid elevated brown-copper lesions on the face, the trunk, the buttocks and limb extension areas. They develop in weeks or months and produce a leuco pigmented scar. Gummas are 2-10 cm hypodermic lesions involving the skin, mucosa membranes, bones and internal organs. They take approximately four months to undergo the infiltration, softening, ulceration and scarring stages. They are commonly found on the limbs, the head and the sternal area. Cardiovascular involvement is found in 25% of the patients with gummas [10] (Figures 1-6).
Congenital syphilis
It is transmitted from the mother to the baby through the placenta. The more recent the disease is in pregnancy, the higher the transmission risks.
Congenital syphilis is referred to as early congenital syphilis when an infected baby is born or when the infection develops before the age of 2. Like in the secondary stage of acquired syphilis, the infection spreads by treponemal dissemination.
Symptoms can be apparent at birth or develop during the 6th-8th weeks of life. Dermatologically, several types of lesions can be seen. Some of them are specific of the congenital form, such as pemphigus on the palms and soles, onychosis, perionychosis and moist papules clustering round body orifices (mouth, nose, anus, vulva) and leading to very deep painful radiating fissures.
Mucocutaneous involvement includes very early secreting rhinitis, laryngitis producing a dysphonic cry (Genaro Sisto’s sign) and oral lesions similar to the ones in adults. Plane condylomas appear as eroded plane papules in the diaper area. Bones are frequently involved. Long-bone osteochondritis and periostitis are very painful conditions leading to Parrot’s pseudo paralysis, an antalgic posture of the affected limb. Systemic manifestations involve different organs and it may be critical in newborns.
Late congenital syphilis occurs in children older than two and is later detected only using lab tests. It does not represent an infectious stage, but it is characterised by the scarring stigmas of undiagnosed early lesions. Central nervous system, bones, teeth and skin are affected causing chorioretinitis, corneal vascularization, frontal lumps, saddle nose, saber shin, mulberry molars, Hutchinson’s teeth, perioral grooves [1] (Figure 1).
Diagnosis
Treponema pallidum
Treponema pallidum is a bacterium that cannot be cultured on artificial media. There are two diagnostic tests:
• T pallidum detection: dark field microscopy, PCR amplification and direct immunofluorescence.
• Serological tests.
Non-treponemal tests
They are used to detect unspecific antibodies known as reagins produced as a response against lipoidal antigens that are probably released by the treponemes themselves due to cellular damage. These tests are called Venereal Disease Research Laboratory (VDRL) and Rapid Plasma Reagin (RPR) with carbon aggregates and macroscopic reading. The results can be false-positive and so may not be indicative of syphilis. Therefore, they should be confirmed with a treponemal test.
Treponemal tests
They are carried out to detect specific antibodies reacting against treponemal proteins. They include the Treponema pallidum particle agglutination test (TP-PA), the treponemal microhemo- agglutination test (MHA-TP), the hemagglutination test (HA-TP), the fluorescent treponemal antibody absorption test (TFA-ABS) and enzyme immunoassay (EIA)/enzyme-linked immunosorbent assay (ELISA) [7].
Treatment
Penicillin is the drug of choice in every syphilis stage. Benzathine and crystalline forms are generally used. Treatment dosage and duration vary according to both the stage and the clinical presentation of the disease. Ophthalmic and neurological involvement is another important variable. Penicillin shows maximun efficacy and non-resistance. The number of benzathine penicillin doses has not been determined yet.
Two or three doses of benzathine penicillin G (2.400.000 U, IM) are recommended for the treatment of primary, secondary and early latent syphilis. For patients allergic to beta-Lactam derivatives and older than 8 years, the therapeutic alternatives are doxycycline (100 mg orally every 12 hours for 14 days) or tetracycline (500 mg orally every 6 hours for 14 days). Patients with late latent syphilis should be treated with more than three doses of benzathine penicillin G (2.400.000 U, IM, weekly). Doxycycline (100 mg every 12 hours for 28 days) or tetracycline (500 mg every 6 hours for 28 days) should be administered when penicillin allergy is proved.
Penicillin is the only drug that has been demonstrated to be effective in treating syphilis during pregnancy. Standard doses should be administered. There is international agreement on desensitization when patients are allergic to penicillin [11]. Crystalline penicillin G IV (100000-300000 U/kg/d for 10 days) is recommend for treating congenital syphillis. When congenital syphilis is unduly diagnosed or retreated, aqueous penicillin G should be used (200000-300000 U/kg/d for 10-14 days) [1].
Materials and Methods
An observational retrospective descriptive study was performed from 1st January 2013 to 31st December 2017 at Sor María Ludovica children’s hospital by analysing clinical, hospitalization and referral reports of 50 patients with suspected syphilis, 36 of which had been confirmed with serological tests.
At the study hospital there is a neonatal intensive care unit without maternity care. The Dermatology Department receives an average of 6500 outpatients and 300 interdepartmental consultations every year.
The following variables were assessed: length of hospital stay (months), sex (female/male), syphilis types (congenital/ acquired), infection stages (early and late congenital syphilis/ primary, secondary and tertiary acquired syphilis), transmission mode (horizontal, sexual, unknown) and clinical presentation. Tables 1 and 2 shows the collected information.
| Patient | Age Months |
Sex | Infection stage | Clinical presentation |
|---|---|---|---|---|
| 1 | 1 | M | Early | Pretibial aplasia cutis, hepatosplenomegaly |
| 2 | 3 | M | Early | Syphilic pemphigus, orifice bloody secretions, Genaro Sisto’s cry |
| 3 | 24 | F | Early | Tibial periostitis, Parrot’s pseudo-paralysis |
| 4 | 1 | M | Early | Serological diagnosis of syphilis without clinical presentation |
Table 1: Congenital syphilis (11%).
| N | Age Months |
Sex | Infection stage | Transmission mode | Clinical presentation |
|---|---|---|---|---|---|
| 1 | 156 | F | Secondary | Unknown | PC on palms and soles |
| 2 | 171 | M | Secondary | Sexual | Moth-eaten alopecia Genital PC |
| 3 | 175 | F | Secondary | Sexual | Moth-eaten alopecia in the frontotemporal region |
| 4 | 173 | M | Secondary | Sexual | OL Foreskin PC |
| 5 | 28 | F | Secondary | Unknown | Diffuse alopecia |
| 6 | 180 | F | Secondary | Sexual | OL on the mucous membrane |
| 7 | 85 | F | Secondary | Unknown | Generalised PL |
| 8 | 159 | F | Secondary | Sexual | Genital PC |
| 9 | 14 | M | Secondary | Unknown | Diffuse alopecia PL in the diaper area |
| 10 | 84 | F | Secondary | CSA | Perianal PC |
| 11 | 186 | F | Primary | Sexual | Genital chancre |
| 12 | 217 | M | Secondary | Sexual | Genital PC |
| 13 | 216 | M | Secondary | Sexual | Balanitis Inguinal lymphadenopathy |
| 14 | 24 | M | Secondary | Unknown | Erosive lesions of the penis Inguinal PC |
| 15 | 60 | F | Secondary | Unknown | Neck PL Polyadenopathies |
| 16 | 26 | M | Primary | Unknown | Oral mucosa chancre |
| 17 | 36 | M | Secondary | Unknown | PL on the trunk, palms and soles |
| 18 | 72 | M | Secondary | Unknown | Diffuse alopecia |
| 19 | 182 | F | Secondary | Sexual | Genital PC |
| 20 | 15 | F | Secondary | Unknown | Genital PC |
| 21 | 128 | F | Secondary | CSA | Perianal PC |
| 22 | 11 | M | Secondary | Unknown | Generalised PL |
| 23 | 27 | M | Secondary | Unknown | Bilateral angular cheilitis Oral OL |
| 24 | 74 | F | Secondary | CSA | Perianal PC |
| 25 | 169 | F | Secondary | Sexual | Genital PC |
| 26 | 25 | F | Secondary | CSA | Perianal PC |
| 27 | 27 | F | Secondary | CSA | Genital PC |
| 28 | 36 | F | Secondary | CSA | Genital PC |
| 29 | 12 | M | Secondary | Unknown | Diffuse alopecia |
| 30 | 170 | F | Secondary | Sexual | Oral OL Genital PC |
| 31 | 109 | F | Secondary | CSA | Perianal PC |
| 32 | 148 | F | Secondary | Sexual | Palatal erosion Neck PL |
Table 2: Acquired syphilis (89%).
A multidisciplinary committee on child sexual abuse formed by gynecologists, dermatologists, psychiatrists, psychologists and social workers assessed all patients with acquired syphilis without reported sexual activity (Tables 1 and 2).
Results and Discussion
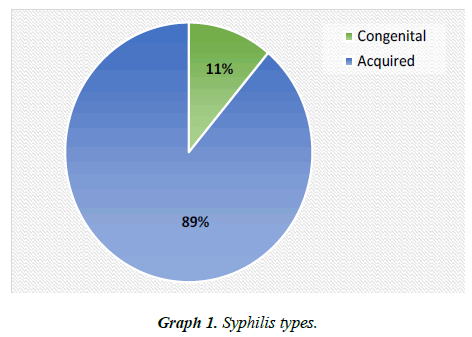
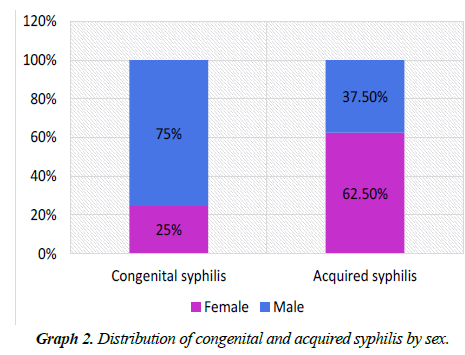
A total of 36 patients were serologically diagnosed with syphilis. The mean age was 72 months (age range: 0-217 months). Eleven percent had congenital syphilis while the remaining 89% had acquired syphilis (Graph 1). Congenital syphilis was more common in boys (75%) whereas acquired syphilis was more frequently reported in girls (62.5%) (Graph 2).
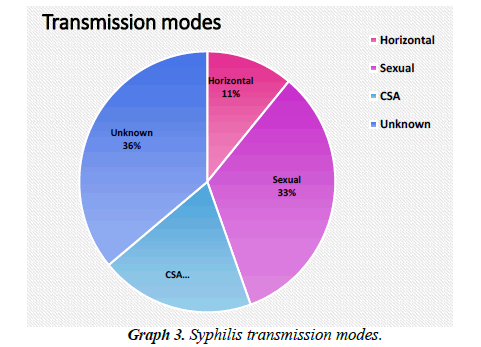
Syphilis was transmitted horizontally (11%), sexually (33.5%) and by sexual abuse (19.5%). The transmission mode was unknown in 36% of the cases (Graph 3).
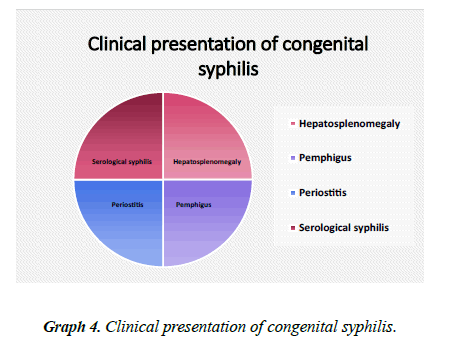
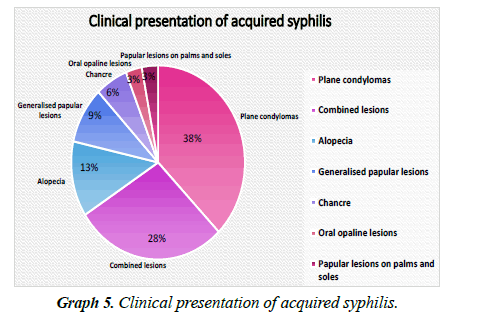
Clinical presentation was heterogeneous. The 4 patients with congenital syphilis showed different clinical manifestations (Graph 4). Acquired syphilis evolved with genital and perianal plane condylomas (12 patients), combined lesions (9 patients), alopecia as the sole symptom (4 patients), generalized papular lesions (3 patients), genital chancres (1 patient), oral chancres (1 patient), oral opaline lesions (1 patient) and papular lesions on the palms and soles (1 patient) (Graphs 4 and 5).
Conclusion
An annual increase of syphilis incidence was reported during 2013-2017. In the last two years, it has shown a two-fold increase correlating with the recent upsurge of sexually transmitted diseases worldwide.
Importantly, only 11.1% of the patients had congenital syphilis. This can be due to the kind of consultations made on outpatients and inpatients to the Department of Dermatology at the studied tertiary care hospital which offers neonatal but not maternity services. Moreover, neonatal serological screening is systematically performed in other hospitals with maternity care in the same city, which has contributed to diagnosing and treating congenital syphilis in their neonatology departments without referrals.
It was not possible to establish a relation between the reported higher incidence of acquired syphilis in girls and a particular condition, except for sexual abuse which was reported in 19.55% of the cases. The girls were all 25-109 months old, which can be associated with a more vulnerable population in terms of age and sex.
The percentage of patients with unknown syphilis transmission mode was high (36%). All these patients lived with at least one person who had a serological diagnosis of syphilis. These findings warn about the importance of identifying and working on unhealthy family habits facilitating bacterial transmission through fomites or non-sexual direct contact. Long-term followup is crucial for children with initially undiagnosed sexual abuse due to absent lesions, especially those who cannot express themselves or have uncooperative families.
The heterogeneous clinical presentation reported in this study reinforces the concept that syphilis is a disease with variable signs and symptoms. That is why, it is referred to as The Great Pretender by dermatologists.
Pediatric dermatologists play an important role in the early diagnosis of syphilis since they can unmask the disease through mucocutaneous lesions during outpatient hospital visits.
References
- Bermejo A, Leiro V. SÃfilis. En: Larralde M, Abad P, Luna P (eds.) DermatologÃa pediátrica, 2°edición. Buenos Aires: Editorial Journal. 2010;3:260-3.
- Leiro V, Bermejo A. SÃfilis adquirida temprana familiar. DermatologÃa Argentina: Volumen XII. 2006;1:66-8.
- Hofmann B, Schuppe HC, Ruzicka T, et al. Acquired syphilis II in early childhood: Reappearance of syphilis brephotrophica. J Am Acad Dermatol. 1998;38(4):638-9.
- Zhou P, Qian Y, Lu H, et al. Nonvenereal transmission of syphilis in infancy by mouth-to-mouth transfer of prechewed food. Sex Transm Dis. 2009;36(4):216-7.
- TellerÃa R, DumondÃn V, Cirio A, et al. SÃfilis en la infancia: Estudio retrospectivoen un hospital pediátrico. DermatologÃa Argentina. 2017:23:66-72.
- Sanchez R, Miguel A. Enfermedades de transmisión sexual. SÃfilis. EN: Fitzpatrick, Wolff K, Godlsmith L, Katz S (eds.). DermatologÃa en Medicina General. 7° edición. Buenos Aires: Editorial Panamericana. 2003;pp:1955-77.
- https://www.sadi.org.ar/recomendaciones-y-consensos/item/49-primerconsenso-dediagnostico-tratamiento-y-prevencion-de-las-enfermedades-de-transmision sexual.
- DÃaz MG, Carbó E, Guardati MV, et al. SÃfilis secundaria en cavidad oral. Reporte de dos casos. Rev Arg de Dermatol. 2008;89(4):33-55.
- Ornelas J, Agbai O, Kiuru M, et al. Alopecia as the presenting symptom of syphilis. Dermatology Online Journal. 2015;21(7):4-5.
- Garritano MV, Jaurigoity ME, Maradeo MR, et al. Presentación de un caso y revisión bibliográfica. SÃfilis terciaria cutánea: Una gran desconocida. Arch Argent Dermatol. 2008;58:97-103.
- http://www.sad.org.ar/wp-content/uploads/2016/04/Enfermedades-de-Transmision-Sexual-ETS-en-adultos.