Research Article - Current Pediatric Research (2024) Volume 28, Issue 1
Pediatric neurotuberculosis: Clinico-radiological profile in a tertiary care centre in India.
Vedavathi Kunnanayaka1, Ashwini Hiremath2*, Milind Kulkarni3
1Department of Pediatrician, Aster Clinics, Dubai, UAE
2Department of Neurology, BLDE University’s Shri BM Patil Medical College and Research Centre, Vijayapur, India
3Department of Cardiology, BLDE University’s Shri BM Patil Medical College and Research Centre, Vijayapur, India
- Corresponding Author:
- Ashwini Hiremath,
Department of Neurology, BLDE University’s Shri BM Patil Medical College and Research Centre, Vijayapur, India
E-mail: ashwinihiremath2013@gmail.com
Received: 25 December, 2023, Manuscript No. AAJCP-24-127370; Editor assigned: 27 December, 2023, Pre QC No. AAJCP-24-127370(PQ); Reviewed: 10 January, 2024, QC No. AAJCP-24-127370; Revised: 17 January, 2024, Manuscript No. AAJCP-24-127370 (R); Published: 24 January, 2024, DOI:10.35841/0971-9032.28.01.1185-1189.
Abstract
Introduction: Untreated primary tuberculosis cases in children are known to have a higher chance of developing neurotuberculosis than cases in adults. The study aims to assess the clinical profile of pediatric neurotuberculosis.
Methods: This is a retrospective study which was done at a tertiary care hospital for duration of 2 years among 50 pediatric patients diagnosed with neurotuberculosis. Patients were selected on the basis of inclusion and exclusion criteria. Patient’s clinical and laboratory features were noted and analyzed using SPSS version 25.0.
Results: There was predominance of male patients (64%) and rest 36% was female. The age group of 1 to 5 years had maximum number of cases (70%). The most common clinical features were fever (90%) followed by headache (88%), vomiting (70%), seizures (54%). The neuroimaging findings reveal basal enhancement (60%), basal exudates (54%), hydrocephalus (43%), vasculitic infarcts (38%), periventricular ooze (36%) and tuberculomas (26%). 32% patients with neurotuberculosis died and only 68% survived.
Conclusion: There is a higher incidence of neurotuberculosis in children aged 1-5 years. Contrary to recent medical literature, fevers may only last a short while when they first manifest. Neuroimaging and CSF studies are essential for establishing a diagnosis and initiation of early treatment.
Keywords
Children, CSF, Meningitis, Neurotuberculosis, Neuroimaging, Paediatric.
Introduction
One of the most common and ancient infectious diseases, tuberculosis is highly prevalent, especially in India. The WHO global tuberculosis report 2023 states that there were total cases of 10 million cases globally out of which reported cases in India were 2.8 million. The total number of deaths till 2022 in India was 342000. HIV cases account for 48000 of all new incident TB cases [1,2].
11% of tuberculosis cases worldwide were reported in children under the age of 15 [3]. Tubercular Meningitis (TBM), the most severe form of extra pulmonary tuberculosis, affects nearly one-fourth of children with tuberculosis [4]. TBM primarily affects younger children, peaking between the ages of 23 and 49 months [5-7]. Despite making up a small percentage of all tuberculosis cases, TBM produces a disproportionately high rate of morbidity and mortality [8]. Only 16%-20% of infants with TBM are said to have lived without experiencing any sequalae and the death rate among these patients ranges from 13%-70% [9]. A persistent neurological, cognitive, behavioral, or developmental disability affects significant TBM survivors [10].
Early diagnosis of neurotuberculosis is challenging due to various factors such as the wide range of tuberculosis symptoms, prolonged asymptomatic course of the disease, delayed diagnosis, decreased efficacy of anti-TB treatment in advanced cases, high rate of false-negative chest radiographs, and tuberculin tests [11,12]. Primary bacillemia follows mycobacterium tuberculosis infection or the reactivation of prior tuberculosis, and this causes tuberculosis foci to form in a variety of organs, including the meninges, the brain, and the spinal column. This usually happens as a result of a primary infection in children [13].
For neurotuberculosis to be caused there must be a subependymal tubercle that develops, grows, and bursts into the subarachnoid area. This causes the tubercular protein to leak into the subarachnoid area, which triggers an allergic response. Typically, this causes gelatinous basal exudates to develop [14]. The exudate causes vasculitis in the cortico-meningeal arteries, which in turn causes border zone encephalitis. An infarction may occur when there is further involvement of major vessels, such as the middle meningeal artery, either as a result of arteritis or subsequent to cerebral edema entrapment [15]. Communicating hydrocephalus is caused when basal exudates obstruct the basal subarachnoid cisterns, obstructing the regular flow of Cerebrospinal Fluid (CSF) out of the ventricular system [16].
For individuals with neurotuberculosis, the age of onset and the stage of presentation are critical determinants that determine their clinical prognosis, morbidity, and mortality. The surviving also exhibits a broad range of neurological consequences. Hence the present study was done to study the clinical profile of pediatric neurotuberculosis.
Material and Methods
The retrospective study was done at a tertiary care centre for a period of 2 years among pediatric population diagnosed with neurotuberculosis. Ethical permission was taken from institutional ethical committee before the commencement of study.
Total 50 cases of pediatric neurotuberculosis were selected through convenience sampling. Cases with CSF analysis confirming neurotuberculosis and pathognomonic radiological (Computed Tomography (CT) scan or Magnetic Resonance Imaging (MRI) brain with contrast) features and within the age group of 6 months to 12 years were included for the study. Patients with coexisting central nervous system abnormalities such as anatomical malformations, epilepsy, and other isolated or coexisting infections (pyogenic meningitis, viral meningoencephalitis) were excluded from the study.
Recorded were the patient's demographics, symptoms at presentation, history of contact with a tuberculosis case and vaccination history. A physical examination was conducted, with particular attention paid to fever, hepatosplenomegaly, the scar from the Bacillus Calmette-Guerin (BCG) vaccine, examinations of the chest, Central Nervous System (CNS), and fundus examination.
A complete blood count, chest X-ray, and Gastric Aspirate (GA) CBNAAT were performed on each patient in order to search for signs of pulmonary tuberculosis; contrast-enhanced computed tomography and magnetic resonance imaging were used to confirm the diagnosis; CSF analyses, including microscopic, biochemical, and microbiological analyses; CSF CBNAAT was performed in all cases. A baseline liver function test was performed to identify abnormal liver function; a tuberculin test and an HIV test were performed on each patient. Throughout their hospital stay, the patients were observed, and we documented any cases of death, the duration from admission to death, the necessity for neurosurgical procedures (such as a ventriculoperitoneal shunt, external ventricular drainage, and ventricular tap), the requirement for ventilation, and the emergence of ATT-induced hepatitis.
Statistical analysis
A Microsoft Excel spreadsheet was used to record the data, which were then analyzed using SPSS for Windows version 25.0 (IBM Corp., Armonk, NY, USA) and the relevant statistical tests.
Results
Out of 50 patients of pediatric neurotuberculosis there was predominance of male patients (64%) and rest 36% were female. Maximum number of cases was in the age group of 1 to 5 years (70%). Out of 50 cases 13 were in the age group of 6 to 12 years and 2 were in the group of less than one year as shown in Table 1.
| Variable | Frequency (%) | |
|---|---|---|
| Gender | Male | 32 (64) |
| Female | 18 (36) | |
| Age | Less than 1 year | 2 (5) |
| 1 to 5 years | 35 (70) | |
| 6 to 12 years | 13 (25) | |
Table 1. Demographic detail of patients.
The most common clinical features were fever (90%) followed by headache (88%), vomiting (70%), altered sensorium (82%), seizures (54%), focal deficit (12%), papilloedema (28%), neck stiffness (80%). BCG scar was noted in almost 56% of cases. Some of the uncommon symptoms were weight loss (40%), anemia (38%) as shown in Table 2.
| Clinical features | Frequency (%) |
|---|---|
| Fever | 45 (90) |
| Headache | 44 (88) |
| Vomiting | 35 (70) |
| Altered sensorium | 41 (82) |
| Seizures | 27 (54) |
| Focal deficit | 6 (12) |
| Papilloedema | 14 (28) |
| Weight loss | 20 (40) |
| BCG scar | 28 (56) |
| Anemia | 19 (38) |
| Neck stiffness | 40 (80) |
Table 2. Clinical features of patients.
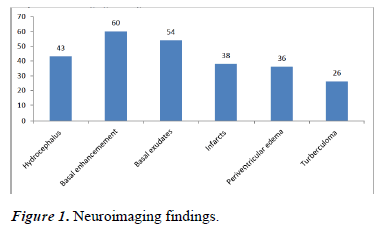
Laboratory findings showed CSF lymphocytosis (42%), elevated CSF protein in 76% and, raised CSF ADA levels in 40% cases. Mantoux positivity was seen in 43% and hyponatremia in almost 58% cases along with abnormal chest X-ray (28%), miliary TB (6%), lymphadenopathy (10%) and associated bronchopneumonia (14%). The neuroimaging findings revealed basal enhancement (60%), basal exudates (54%), infarcts (38%), hydrocephalus (43%) periventricular ooze (36%) and turberculomas (26%) as shown in Table 3 and Figure 1.
| Findings | Frequency (%) |
|---|---|
| CSF lymphocytosis | 21 (42) |
| Elevated CSF protein | 38 (76) |
| Rise CSF ada levels | 20 (40) |
| Abnormal chest X-ray | 14 (28) |
| Miliary TB | 3 (6) |
| Lymphadenopathy | 5 (10) |
| Bronchopneumonia | 7 (14) |
| Neuroimaging | |
| Hydrocephalus | 21 (43) |
| Basal enhancemement | 30 (60) |
| Basal exudates | 27 (54) |
| Infarcts | 19 (38) |
| Periventricular edema | 18 (36) |
| Turberculoma | 13 (26) |
Table 3. Laboratory findings.
The outcomes of the patients were very poor. 32% patients with neurotuberculosis died and only 68% survived as shown in Table 4. 7 cases required neurosurgical intervention. During the duration of stay, raised liver function tests were noted in 6 patients. The patients who presented late and with stage 3 of TBM died within four-five days of admission into ICU.
| Outcome | Frequency (%) |
|---|---|
| Died | 16 (32) |
| Survived | 34 (68) |
Table 4. Outcome of patients.
Discussion
Neurotuberculosis poses a significant challenge to the Indian healthcare system. Although the condition has been shown to affect people of all ages, the majority of cases occur during the first five years of life, according to recent medical research [17-19]. 70% of the total cases in this study occurred in the 1-5 year age range. Number of male patients was more as compared to females similar to other studies [20,21].
The most common clinical features were fever (90%) followed by headache (88%), vomiting (70%), altered sensorium (82%), seizures (54%). Some of the uncommon symptoms were weight loss, anemia and focal deficits due to vasculitic infarcts. Bhargava et al., and Farinha et al., reported to a typical presentation of fever for >15 days at hospitalization [19,22]. Most of the other symptoms noted were due to raised intracranial tension. It has been noted that focal deficits and seizures occur as a result of the involvement of the brain parenchyma as these signs are not seen in patients with isolated meningeal involvement. In a study by Alarcon et al., [23], 30 patients had movement disorders out of 130 TBM cases studied over 7 years. Twenty patients had tremors, seven had chorea, and three had dystonia. Out of seven patients, five were less than 5 years old and one was less than 12 years of age. However none of our patients had abnormal movements.
The neuroimaging findings of our study revealed basal enhancement (60%), basal exudate (54%), infarcts (38%), hydrocephalus (43%), periventricular ooze (36%) and tuberculomas (26%). These results are in contrast to a research by Lee et al., that revealed hydrocephalus in 78% of cases and basal exudates in 100% of cases. Any patient who has a clinical suspicion of neurotuberculosis should have neuroimaging performed as soon as they are admitted because it is a very effective method of diagnosing the illness [24]. Based on a chest X-ray, 26% of patients showed a predominant focus of lung infection, which is consistent with recent research.
The outcome of patients were poor, 32% of patients died and these deaths may be due to late presentation of cases in hospital and therefore results into late management and mortality. There is a dearth of recent information on the clinical spectrum and prognosis of extrapulmonary tuberculosis in children. Paediatric neurotuberculosis frequently has clinical characteristics similar to CNS illnesses caused by bacterial, fungal, and viral diseases. A child frequently arrives at the disease's advanced stage, which is linked to increased morbidity and mortality. A significant determinant of death is the clinical staging at presentation. For an early diagnosis and course of treatment, a high degree of suspicion is therefore necessary. Children who are diagnosed later in life are particularly vulnerable to behavioural and neurocognitive disorders [25].
Limitation of study includes small sample size and as it was a retrospective study data available in hospital records was the only source to interpret results and long follow ups of patients could not be taken.
Conclusion
Clinical signs are still not conclusive in identifying neurotuberculosis in children. It seems that neuroimaging is the most sensitive method for prognosis as well as diagnosis. In this study, it was discovered that having basal exudates, hydrocephalus, and being young were all linked to poor outcomes. Therefore, it's imperative to keep a close eye out for neurotuberculosis in children in order to avoid neurological morbidity, impairment, and death.
References
- K Floyd. Global tuberculosis report 2023. Geneva, Switzerland: WHO. 2023.
- Cherian AB, Thomas SV, Bryan R, et al. Central nervous system tuberculosis. Afr Health Sci 2011; 11: 116-27.
- Dodd PJ, Gardiner E, Coghlan R, et al. Burden of childhood tuberculosis in 22 high-burden countries: A mathematical modelling study. Lancet Glob Health 2014; 2: e453-9.
- van Well GT, Paes BF, Terwee CB, et al. Twenty years of pediatric tuberculous meningitis: A retrospective cohort study in the western cape of South Africa. Pediatrics 2009; 123: e1-8.
- Farinha NJ, Razali KA, Holzel H, et al. Tuberculosis of the central nervous system in children: A 20-year survey. J Infect 2000; 41: 61-8.
- Yaramis A, Gurkan F, Elevli M, et al. Central nervous system tuberculosis in children: A review of 214 cases. Pediatrics 1998; 102: E49.
- Thwaites GE, van Toorn R, Schoeman J. Tuberculous meningitis: More questions, still too few answers. Lancet Neurol 2013; 12: 999-1010. [Crossref]
- Mahadevan B, Mahadevan S, Serane VT. Prognostic factors in childhood tuberculous meningitis. J Trop Pediatr 2002; 48: 362-5.
- Misra UK, Kalita J, Srivastava M, et al. Prognosis of tuberculous meningitis: A multivariate analysis. J Neurol Sci 1996; 137: 57-61.
- Rohlwink UK, Donald K, Gavine B, et al. Clinical characteristics and neurodevelopmental outcomes of children with tuberculous meningitis and hydrocephalus. Dev Med Child Neurol 2016; 58: 461-8.
- Garcia-Monco JC. Central nervous system tuberculosis. Neurol Clin 1999; 17: 737-59.
- Thwaites GE, Tran TH. Tuberculous meningitis: Many questions, too few answers. Lancet Neurol 2005; 4: 160-70.
- Pavlinac PB, Naulikha JM, John-Stewart GC, et al. Mycobacterium tuberculosis bacteremia among acutely febrile children in Western Kenya. Am J Trop Med Hyg 2015; 93: 1087-91.
- Chatterjee S. Brain tuberculomas, tubercular meningitis, and post-tubercular hydrocephalus in children. J PediatrNeurosci 2011; 6: S96-100.
- Chan KH, Cheung RT, Lee R, et al. Cerebral infarcts complicating tuberculous meningitis. Cerebrovasc Dis 2005; 19: 391-5.
- NK Venkataramana. Hydrocephalus Indian scenario-A review. J PediatrNeurosci 2011; 6(2): 611-22.
- Chang KH, Han MH, Roh JK, et al. Gd-DTPA-enhanced MR imaging of the brain in patients with meningitis: Comparison with CT. AJNR Am J Neuroradiol 1990; 11: 69-76.
- Molavi A, LeFrock JL. Tuberculous meningitis. Med Clin North Am 1985; 69: 315-31.
- Bhargava S, Gupta AK, Tandon PN. Tuberculous meningitis–A CT study. Br J Radiol 1982;55:189-96.
- Dhawan SR, Gupta A, Singhi P, et al. Predictors of neurological outcome of tuberculous meningitis in childhood: A prospective cohort study from a developing country. J Child Neurol 2016; 31: 1622-7.
- Israni AV, Dave DA, Mandal A, et al. Tubercular meningitis in children: Clinical, pathological, and radiological profile and factors associated with mortality. J Neuro sci Rural Pract 2016; 7: 400-4.
- Farinha NJ, Razali KA, Holzel H, et al. Tuberculosis of the central nervous system in children: A 20-year survey. J Infect 2000; 41: 61-8.
- Alarcon F, Duenas G, Cevallos N, et al. Movement disorders in 30 patients with tuberculous meningitis. Mov Disord 2000; 15: 561-9.
- Lee LV. Neurotuberculosis among Filipino children: An 11 years’ experience at the Philippine children’s medical center. Brain Dev 2000; 22: 469-74.
- Awasthi S, Moin S. Effectiveness of BCG vaccination against tuberculous meningitis. Indian Pediatr 1999; 36: 455-60. 21.