Case Report - Journal of Clinical Ophthalmology (2020) Therapeutic Advances in Vision Research
PEDI (Pullout Exteriorized Drainage Implant) suture: Case report of an improved ripcord technique in glaucoma drainage implant devices
Khin P Kilgore1, Khaled Moumneh2, Oluwatosin U Smith3, Ronald L Fellman3, Arsham Sheybani1, Davinder S Grover3*
1 Washington University, School of Medicine, St. Louis, Missouri, USA
2 Touro College of Osteopathic Medicine, New York, USA
3 Glaucoma Associates of Texas, Dallas, Texas, USA
- Corresponding Author:
- Dr. Davinder S. Grover
Attending Surgeon and Clinician 10740 N. Central Expressway, Suite 300 Dallas, Texas, 75231
E-mail: dgrover@glaucomaassociates.com
Accepted date: 14 December, 2020
Citation: Kilgore KP, Moumneh K,Smith OU, et al. PEDI (Pullout Exteriorized Drainage Implant) suture: Case report of an improved ripcord technique in glaucoma drainage implant devices. J Clin Ophthalmol 2020;4(S1):13-15.
Abstract
Background: To describe the PEDI (Pullout Exteriorized Drainage Implant) suture technique, an improvement on the ripcord technique that can be removed in the office setting under topical anesthesia.
Case presentation: A 5-year-old girl with congenital ectropion uvea and bilateral glaucoma had poor intraocular pressure (IOP) control on maximal medical therapy. She received a Baerveldt 350 glaucoma drainage device in each eye using the PEDI suture technique and tube fenestrations. The PEDI suture technique involves the classic ripcord technique of inserting a 4-0 nylon suture into the proximal end of the tube and burying the distal tip under the conjunctiva. However, as the distal nylon ripcord is tunneled towards the adjacent inferior quadrant, the needle is exteriorized near the fornix for a very short course then brought back under the conjunctiva. Patient’s IOPs improved post-operatively from low-30s to mid-teens until the fenestrations closed. IOP then increased to low-30s in the right eye and low-20s in the left eye 4-5 months postoperatively, so the PEDI suture ripcord was removed from the right eye in clinic under topical anesthesia. The ripcord in left eye was similarly removed 9 months post-operatively, and the IOPs have remained controlled in the mid-teens with 3 IOP-lowering medications in both eyes.
Conclusion: The PEDI suture technique is a practical modification to the standard ripcord technique that allows for easier and safer removal in clinic without requiring sedation, conjunctival incision or a return to the operating room with its attendant anesthesia exposure for pediatric patients.
Keywords
Glaucoma drainage device, Ripcord removal, Pediatric glaucoma
Abbreviations
GATT: Gonioscopy-Assisted Transluminal Trabeculotomy; GDD: Glaucoma Drainage Device; IOP: Intraocular Pressure; OD: Right eye; OS: Left eye; OU: Both eyes; PEDI: Pullout Exteriorized Drainage Implant; POD: Post-Operative Day.
Background
Glaucoma Drainage Devices (GDDs) have traditionally been used in cases of refractory glaucoma with uncontrolled intraocular pressure (IOP) since their conception in 1969 [1,2]. The results from the landmark studies on GDD’s (Tube versus Trabeculectomy study, Primary Tube versus Trabeculectomy Study, Ahmed versus Baerveldt Study, and Ahmed Baerveldt Comparison Study) have allowed surgeons to be more comfortable with the safety and efficacy of these implants. Consequently, GDDs are being used more often in children and adults in a broad range of refractory glaucoma types [2].
Children that require non-valved GDD’s represent a unique challenge. If one uses a dissolvable suture to ligate the tube, flow will be established after approximately 4-6 weeks, requiring activity restrictions during that 2 week period, and a week after tube opening. It is often difficult to limit young children’s activities for that long, however, especially if they are without continual supervision while they are in daycare or school. Alternatively, one can stage a GDD placement, by either tucking the tube in the subconjunctival space and then returning to the operating room to insert it in the anterior chamber/ sulcus, or inserting the tube into the eye, but ligating it with a non-dissolvable suture (thus allowing for fenestrations), with subsequent surgical or laser lysis of the suture when appropriate. Using a laser at the slit lamp is often not possible in children, however, and having an additional suture in the anterior chamber puts the patient at risk of trauma to the lens or iris, especially if the anterior chamber shallows when the tube opens. Some of these techniques prevent functional fenestrations of the tube and, more importantly, involve additional trips back to the operating room with repeated anesthetic exposure for the child.
In this report, we describe an alternate approach with a ripcord that is tucked in the inferior fornix with an exteriorized nylon suture. This technique allows for functional fenestrations and complete control over when the tube opens. The tube can be opened at the slit lamp even in a young patient without much difficulty, which has the additional benefit of reducing the patients’ exposure to general anesthesia or sedation, and their possible neurotoxic effects [3]. The study was reviewed and approved by a central Institutional Review Board (IRB) committee, and adhered to the tenets of the Declaration of Helsinki.
Case Presentation
A 5-year-old girl with congenital ectropion uvea and glaucoma in both eyes (OU) presented in June 2016 with elevated intraocular pressures (IOP) OU. The patient had initially undergone gonioscopy-assisted transluminal trabeculotomy (GATT) bilaterally, in October 2013 for the left eye (OS) and March 2014 for the right eye (OD). On her visit in June 2016, IOP’s were 31 mmHg OD and 32 mmHg OS.
The patient was already on maximally-tolerated medical therapy with latanoprost OU, pilocarpine (2%) OS, and dorzolamide/ timolol OU. After discussion with the family, a Baerveldt 350 was implanted in the left eye in July 2016 using the PEDI suture method. In this patient, we used a Baerveldt 350 glaucoma implant (Johnson and Johnson Vision, Santa, CA), but the technique can be utilized with any non-valved implant (see Video S1). The GDD surgery is started traditionally with a 5-clock hour peritomy and sub-Tenon’s dissection in the supratemporal quadrant, and isolation of the superior and lateral rectus muscles. The GDD plate is then tucked under the bellies of the rectus muscles.
Video S1
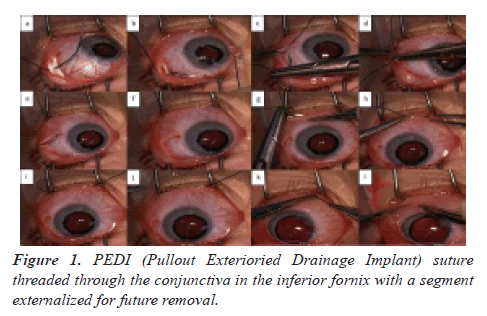
The next step involves the PEDI suture ripcord: the free end of a 4-0 nylon suture with a needle on the other end is inserted into the tube opening in the plate (Figure 1a). The tube is completely ligated near the plate with a 7-0 polypropylene suture over the ripcord. After securing the GDD plate with interrupted 9-0 polypropylene sutures, the tube is inserted into the anterior chamber, and secured to the sclera with a 7-0 polyglactin 910 Figure 8 suture (Figure 1b). Multiple fenestrations are created in the tube anterior to the ligation. The end of the ripcord with the needle is then tunneled in the subconjunctival space towards the inferior-temporal fornix. The needle is then brought anteriorly and externalized through the conjunctiva a few millimeters nasally, tucked back under the conjunctiva and externalized again. The distal end of the suture is trimmed at the level of the conjunctiva, leaving only a small forniceal section of the nylon externalized (Figure 1c-1l) in the inferior fornix. The tube overlying the sclera is then covered with a corneal graft, and the conjunctiva is re-approximated using 8-0 Vicryl sutures. When desired, the ripcord can be removed by pulling on the externalized nylon section at the slit lamp (or with loupes) under local anesthesia with blunt epilation forceps. This technique causes minimal pain and can be done even in a minimally cooperative child/infant from several months old to several years old.
In August 2016, the IOP’s were 30 mmHg OD (on maximal medical treatment) and 23 mm Hg OS (post-operative day [POD] #41). Therefore, the same procedure was performed in the right eye. The child was scheduled to start kindergarten in September 2016. By utilizing the PEDI suture technique, the surgeon felt comfortable with the child attending her first day of kindergarten (an important milestone for both the parents and child to enjoy).
During the following post-operatively months, the IOP was well-controlled in the mid-teens as the fenestrations worked. The IOP began to increase despite treatment with dorzolamide/ timolol OU daily and prednisolone acetate OU twice daily, and in November 2016 (POD #67) the IOP’s were up to 31 mmHg OD and 20 mmHg OS. The parents are both working professionals and wanted to be able to schedule the tube opening around their work schedule and the patient’s school schedule, so it was scheduled for the next month.
On December 27, 2016, the IOP’s were 29 mmHg OD and 20 mmHg OS on maximal medical treatment. The ripcord suture was safely removed in the exam lane with epilation forceps after instilling topical proparacaine, without the need of a slit lamp. The IOP OD dropped to 10 mmHg. All glaucoma drops were stopped in the right eye, and the patient was put on strict activity limitations for just one week. She did not miss any school during this time for it was during a holiday break. For the fellow eye, the rip cord opening was scheduled for April 2017, during the patient’s spring break. At the most recent visit in August 2019, IOP was controlled in the mid-teens on dorzolamide/timolol OU daily and latanoprost OU at bedtime.
Discussion
In this technique report, we describe a modification of the widely-used ripcord technique in non-valved GDIs, which reliably restricts flow to the implant until the necessary resistance is formed via capsule formation. By threading the ripcord suture through the conjunctiva twice, a part of the suture remains externalized in the inferior temporal fornix, allowing for removal with the use of topical anesthetic alone, in the clinic without a conjunctival incision. This is in contrast to the traditional method in children, in which the ripcord is buried completely under the conjunctiva and its removal requires a return to the operating room with additional general anesthesia or sedation, conjunctival incision and sometimes closure, resulting in a longer post-operative course.
One possible limitation to the PEDI suture technique is the risk of endophthalmitis as the externalized ripcord may act as a wick for infectious agents. However, this complication can be mitigated with intracameral antibiotics, post-operative topical antibiotics, close monitoring and, most importantly, with proper placement of the exteriorized segment in the fornix, where it is protected from exposure. The authors would not recommend leaving the externalized segment in place for a long period of time, given this theoretical increased risk of infection. Additionally, we ask the patient to avoid swimming and any other activities that may expose them an increased risk of infection. However, leaving the ripcord in place for several months to allow for scheduling around the patient’s school schedule and the parents work schedule allows for minimal disruption to their lives, which are already plagued by the stressors of multiple clinic and operating room visits. This is done in conjunction with patient and parental education about conjunctivitis, or symptoms of ocular irritation or infection upon which they would notify the surgeon in a timely fashion.
Appropriate patient selection guidelines for the PEDI suture technique include ensuring that the patients and their guardians understand its unique risks and benefits, and that the patient is cooperative in the office without any sedation and has normal eyelid anatomy that can be expected to hide the externalized ripcord segment. Patients who have been selected for the PEDI suture technique have tolerated the ripcord removal well in the office without sedation, and without any vasovagal episodes as no ocular muscle manipulation was required. There have also been no instances of the PEDI suture ripcord failing to release in the office setting, but should it occur, the removal may be reattempted under mild oral or inhalational sedation.
Since the IOPs in children rarely stay controlled once the fenestrations close, it is unlikely that ripcord would not need to be removed. However, if ripcord removal is not necessitated or if the externalized segment of the suture is causing ocular irritation, the suture can be trimmed in the office at the proximal end of the externalized segment, converting it to a traditional ripcord.
The main strength of the PEDI suture technique is the elimination of the need for additional general anesthesia or sedation to open the tube. Since anesthesia-induced neurotoxicity in rats was first described in 2001 [4], numerous studies in pediatric populations have shown that multiple or prolonged exposures to anesthesia at a young age may contribute to neurotoxicity, potentially leading to long-term cognitive consequences [3,5,6]. In 2017, the United States Food and Drug Administration thus issued a statement warning that multiple or lengthy exposures to general anesthetic and sedation medications may affect brain development [7]. Newer studies agree that while single exposures to general anesthesia are not associated with neurotoxicity, repeated or prolonged exposure should be avoided when possible [3,8,9].
Decreased time in the operating room is not only beneficial to the patient’s health, but also to their personal and family lives. To have a young child go through a second ocular surgery, significant time must be taken off of work and school. This is where the PEDI suture technique shines, as it avoids the variability and attendant risk of uncontrolled ligature dissolution, the prolonged activity restriction and close supervision during the weeks when the ligature may open, and does not require an invasive procedure to remove. As described in the case, both nylon suture removals were scheduled during holiday breaks and the postoperative courses were so short, the child did not have to take any time off school, thus minimizing the impact to their education and their parents’ jobs.
Conclusion
Overall, we believe that the PEDI suture technique is superior to the traditional ripcord technique used with GDDs, especially in pediatric patients, in whom it is better to avoid the risk of returning to the operating room just to stage their drainage implant surgery. This controlled opening of the tube also applies to certain adults who are not good candidates for uncontrolled opening of their ligatures with the attendant risk of hypotony.
References
- Molteno AC. New implant for drainage in glaucoma. Clinical trial. Br J Ophthalmol. 1969;53:606-15.
- Tan YL, Chua J, Ho CL. Updates on the Surgical Management of Pediatric Glaucoma. Asia Pac J Ophthalmol. 2016;5:85-92.
- Grover LA, Mitchell RB, Szmuk P. Anesthesia Exposure and Neurotoxicity in Children-Understanding the FDA Warning and Implications for the Otolaryngologist. JAMA Otolaryngol Head Neck Surg. 2017;143:1071-2.
- Jevtovic-Todorovic V, Wozniak DW, Benshoff N, et al. Commonly used anesthesia protocol causes neuronal suicide in the immature rat brain. eNeuro. 2001;27:2050.
- Flick RP, Katusic SK, Colligan RC, et al. Cognitive and behavioral outcomes after early exposure to anesthesia and surgery. Pediatrics. 2011;128:e1053-1061.
- Andropoulos DB, Ahmad HB, Haq T, et al. The association between brain injury, perioperative anesthetic exposure, and 12-month neurodevelopmental outcomes after neonatal cardiac surgery: a retrospective cohort study. Paediatr Anaesth. 2014;24:266-74.
- FDA Drug Safety Communications. FDA approves label changes for use of general anesthetic and sedation drugs in young children 2016.
- Warner DO, Zaccariello MJ, Katusic SK, et al. Neuropsychological and Behavioral Outcomes after Exposure of Young Children to Procedures Requiring General Anesthesia: The Mayo Anesthesia Safety in Kids (MASK) Study. Anesthesiology. 2018;129:89-105.
- Davidson AJ, Disma N, de Graaff JC, et al. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet. 2016;387:239-250.