Review Article - Insights in Nutrition and Metabolism (2017) Volume 1, Issue 1
Pain: A patient with painful diabetic neuropathy and post herpetic neuralgia: A review report
Mehboob Matteo Manuelli Haque1*, Tan GLC2
1Department of Public Health, Experimental and Forensic Medicine, Unit of Human Nutrition, University of Pavia, Italy
2Department of Neurology and Psychiatry, University of Santo Tomas, Manila, Philippines
- Corresponding Author:
- Mehboob Matteo Manuelli Haque
Department of Public Health
Experimental and Forensic Medicine
Unit of Human Nutrition, University of Pavia, Italy
Tel: +91-9007322346
E-mail: mehboobhaque906@gmail.com
Received date: January 04, 2017; Accepted date: January 28, 2017; Published date: February 04, 2017
Citation: Haque MMM, Tan GLC. Pain: A patient with painful diabetic neuropathy and post herpetic neuralgia: A review report. Insights Nutr Metabol 2017;1(1):01-09.
Copyright: © 2017 Haque MMM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
State-of-the-art information shows that the incidence of diabetes mellitus will expand via the 12 months 2030, where as much as 50% increase neuropathy and about a quarter will strengthen neuropathic pain. The purported immunocompromised diabetic state makes them additionally prone to various infections, for illustration, herpes zoster illness. Presented on this record is a case of a sixty three-12 months ancient Filipino with painful diabetic neuropathy and who due to this fact developed publish herpetic neuralgia. A pain regimen with pregabalin at the start at one hundred fifty mg/day ultimately attaining 600 mg/day decreased pains, however needed an augmentation with lidocaine patch (5%) utility, and tramadol plus paracetamol fixed dose mixture as rescue medication, for higher manipulate.
Keywords
Diabetic polyneuropathy; Post herpetic neuralgia; Neuropathic pain; Pregabalin
Introduction
Neuropathic soreness is outlined as “agony coming up as an immediate outcome of a lesion or disorder affecting the somatosensory procedure” [1]. This can be brought on by using foremost lesions in the crucial fearful system (e.g. Stroke more than one sclerosis spinal wire damage or trauma) and peripheral nervous approach (e.g. Diabetes mellitus [DM], toxins, accidents and varicella-zoster infections and HIV). The scientific confident signs would incorporate spontaneous affliction, paraesthesia’s and dysesthesia (hyperalgesia and allodynia) at the same time the negative signs would comprise hypoesthesia weak point and loss of steadiness. At the same time rough to estimate painful diabetic neuropathy (PDN) could occur in up to 25% of sufferers with DM [2] and that DM is related to an elevated risk of power submit-herpetic neuralgia (PHN) [3-25].
Neuropathic pain is a complex chronic pain state that usually is accompanied by tissue injury. With neuropathic pain the nerve fibers themselves may be damaged dysfunctional or injured. These damaged nerve fibers send incorrect signals to other pain centres. The impact of nerve fiber injury includes a change in nerve function both at the site of injury and areas around the injury [26-30].
One example of neuropathic pain is called phantom limb syndrome. This rare condition occurs when an arm or a leg has been removed because of illness or injury but the brain still gets pain messages from the nerves that originally carried impulses from the missing limb. These nerves now misfire and cause pain [31-35].
Causes of Neuropathic Pain
Neuropathic pain often seems to have no obvious cause but some common causes of neuropathic pain include:
• Alcoholism
• Amputation
• Back leg and hip problems
• Chemotherapy
• Diabetes
• Facial nerve problems
• HIV infection or AIDS
• Multiple sclerosis
• Shingles
• Spine surgery
• Symptoms of Neuropathic Pain
Neuropathic pain symptoms may include
• Shooting and burning pain
• Tingling and numbness
• Diagnosing Neuropathic Pain
To diagnose neuropathic pain, a doctor will conduct an interview and physical exam. He or she may ask questions about how you would describe your pain when the pain occurs or whether anything specific trigger the pain. The doctor may also request both blood and nerve tests.
Neuropathic Pain Treatment
Some neuropathic pain studies suggest the use of non-steroidal anti-inflammatory drugs such as Aleve or Motrin may ease pain. Some people may require a stronger painkiller such as those containing morphine. Anticonvulsant and antidepressant drugs seem to work in some cases.
If another condition such as diabetes is involved better management of that disorder may alleviate the pain. Effective management of the condition can also help prevent further nerve damage.
In cases that are difficult to treat a pain specialist may use an invasive or implantable device to effectively manage the pain. Electrical stimulation of the nerves involved in neuropathic pain may significantly control the pain symptoms [36-60].
Other kinds of treatments can also help with neuropathic pain. Some of these include:
• Physical therapy
• Working with a counsellor
• Relaxation therapy
• Massage therapy
• Acupuncture
Unfortunately neuropathic pain often responds poorly to standard pain treatments and occasionally may get worse instead of better over time. For some people it can lead to serious disability. A multidisciplinary approach that combines therapies however can be a very effective way to provide relief from neuropathic pain [61-75].
Patient Information and Clinical History
The patient is a 63-12 month-ancient male, Filipino identified with variety 2 DM 12 years in the past. He got here in complaining of reasonable to severe (7-8/10 VAS) spontaneous pricking pains over each toes for the past 4 months. He famous that the pains would also show up when he walked and when his feet touched the cold ground. Eventually there used to be noted accompanying numbness that involved now not best each his feet but also both of his arms. Even though he claimed that he had quite excellent glycaemic manipulate (latest regimen: weight loss program, exercise, sitagliptin or metformin 5/500 mg/tab 1 tab BID and gliclazide 60 mg/tab 1 tab OD) with an HbA1c 6.1%, his pains endured inflicting impaired sleep anxiety symptoms and recurrent work absenteeism.
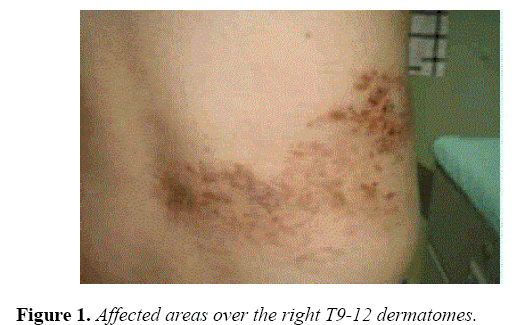
In the final 6 months he developed varicella zoster lesions located on the proper T9-12 dermatome levels accompanied with the aid of power stabbing pains (VAS 7/10) 2 months after. The agony would additionally show up at any time when cloth would touch the affected body components.
Likewise he had a body Mass Index (BMI) of 40 and a known dyslipidemia on healing with a statin. He had no earlier varicella zoster vaccinations. He is negative for HIV and there is no consumption of medicinal drugs that could cause neuropathies (e.g. Colchicine amiodarone and isoniazid among others). Household historical past is likewise unremarkable for any neuromuscular ailments.
As a part of his earlier scientific historical past he was once given from somewhere else a routine for his PDN with vitamin B16, B12 and naproxen (more often than not prescribed for nociceptive ache). Despite 2 months into the routine these didn't alleviate his PDN pains.
He was earlier given a prognosis of “claudication” considering the fact that the suffering was noted more upon ambulation. Nonetheless the dorsalis pedis pulses and ankle-brachial index (1-ranking on the test) have been usual. Upon further historical past taking and examination it was once noted to be considering the fact that of mechanical allodynia (i.e., Affliction occurring on movement).
Clinical Findings and Diagnostic Assessment
On neurologic examination his cognitive repute was average and there have been no cranial nerve deficits. Motor examinations didn't show any atrophy fasciculation’s and ataxia. He used to be competent to ambulate good together with a just right toe and heel walking. Deep tendon reflexes were symmetric and graded +2 in all extremities. Sensory examination was once natural for testable modalities (pinprick, light touch, monofilament and role/ vibration senses focusing on distal limbs (chiefly the enormous toe). However, he had allodynia upon cotton and cold utility typically over the edges of his shingle-affected areas over the proper T9-12 dermatomes (Figure 1).
Activities Nerve Conductions experiences (NCS) revealed usual latencies conduction velocities and amplitudes of evoked motor and sensory nerves (together with emphasis over the sural and superficial fibular nerves). The late response stories (i.e., F-waves and tibial H-reflexes) have been likewise common and aspect-part similar. The electro-physiologic Sympathetic skin Response (SSR) was once absent in the scale down limbs but could be elicited on the upper limbs.
Therapeutic Intervention
The sufferer was once at the beginning started on pregabalin at a hundred and fifty mg/day which was slowly titrated up to 600 mg/day in three weeks. The PDN improved with VAS lowered to 2/10. For the reason that of the PHN the remedy finally needed an augmented cure with lidocaine patch (5%) applied 12 hours per day plus rescue remedy of tramadol+paracetamol combination. With these multi-modal medicines, there was an over-all famous 70% anguish discount and patient have been able to sleep higher think better and return to work more conveniently. Sufferer informed consent was secured as good as Ethics approval [76-85].
Discussion
Diabetic polyneuropathy is one of the most fashioned longterm problems of DM. Most patients would present with distal symmetrical polyneuropathy by and large beginning at the toes and step by step ascending towards the palms. For both forms 1 and a couple of DM, the chance of constructing distal polyneuropathies – together with painful neuropathies – appears to be inversely involving the measure of glycaemic manipulate and is straight correlated with the duration of diabetes. Diagnosis of diabetic neuropathy is more commonly clinic-centred and neurophysiologic tests could also be applied where doubts exist (e.g. Uneven presentation motor weak point and atrophy “pink flags”) [86-100]. Activities NCS findings may yield common findings in those with PDN that will off with small nerve fiber involvement. NCS is a risk-free scan for tremendous fiber neuropathies. In the situations where NCS are average Quantitative Sensory testing, epidermal nerve fiber densities obtained from epidermis biopsies, confocal retinal microscopy and Laser evoked capabilities reviews will in this day and age provide documentation.
In this reward case the events NCS was no longer invaluable and now not unexpected in a sufferer with excellent tendon reflexes and proprioceptive assessments. The SSR an autonomic scan may function a surrogate scan for small nerve fibre neuropathy principally if absent in the lessen limbs (a case in factor for symmetric length-dependent diabetic neuropathy). While clinically ruled out on this present case one must be aware of differentials in small nerve fibre neuropathy that comprise the following: Metabolic issues (e.g. Porphyria and Fabray’s sickness) Infiltrative/Immune (e.g. Lupus, HIV Lyme’s ailment and Amyloidosis) and Toxins/drugs (e.g. Heavy metals, Metronidazole, Nitrofurantoin isoniazid and anti-cancer medications). These differential diagnoses have been ruled out in this present case with thorough historical past taking physical and neurologic examination and common laboratory examinations [101-112].
Prognosis administration and practice parameters for HZ and PHN have been systematically achieved prior to now [113]. In regard to DM and PHN regardless of usual potential that most beneficial glucose manipulate is sought new reports show that improved glucose control may have an impact on more in sufferers with style 1 diabetes than these with sort 2 DM [114,115].
DM patients are extra inclined to viral infections which may be of accelerated severity than in more immune competent subjects. Some measures of phone-mediated immunity are depressed in members with DM (for example T-Mobile deregulation attribute in DM would outcome in an increased incidence of HZ [116]. In one study [117] the cell-mediated immunity closer to HZ virus amongst sufferers with and without DM used to be analysed by means of the gamma interferon ELISPOT assay. Even though the learn did not show any gigantic variations it was once found that the ELISPOT rely was scale back for these with DM than the healthful topics in age-matched groups [118].
Guingard’s group estimated that the crude incidence of HZ infection was greater amongst kind 2 (4.59 per 1000 individual years) than style 1 DM (2. 13 per 1000 individual years). The magnitude of the threat is related to the sufferer’s age (≤ sixty five years old) and the presence of comorbid explanations comparable to (cardiac and power pulmonary disorder). A different workforce [119] recognized 4, 20, 515 cases of HZ (approximately 88 million man or woman-years). Participants with DM represented 8.7% of the individual years they analysed accounting for 14.5% of the patients with HZ contamination. Their incidence of HZ was once larger (78%) in DM and DM used to be related to a 45% adjusted threat of HZ. Additionally, they discovered greater premiums of PHN in individuals with DM than these without and that DM was once associated with an 18% adjusted danger of persistent PHN [120].
Hyperglycaemia used to be located to be a predictor for PHN in one more learns [14]. Despite the fact that they'd a small DM population it's of be aware that four out of 7 (57.14%) DM patients developed PHN compared to healthful topics (15.55%).
Enough pain manipulate is likely one of the targets of medication on account that affliction is probably the most debilitating symptom of PDN and PHN. There are more than one drugs used to deal with these agony syndromes and a discomfort practitioner must correctly weigh the treatment’s protection, efficacy, price and aspect outcome profile of the sufferer’s general knowledge tolerability and repute. For instance, antidepressants could take delivery of two patients who boost symptoms of melancholy, medicinal drugs will also depend on sufferer’s comorbidities like cardiac-hepato-renal impairments with a couple of drug regimens on board [121-125].
Just as utilized in this gift case pregabalin unlike gabapentin (one more alpha-2 delta ligand) was the first option for healing in PDN [126] and it belongs to the tier of first line therapies derived from a couple of instructional materials. The common antagonistic results of pregabalin include somnolence, dizziness, peripheral edema and weight reap. At the same time pregabalin dose of one hundred fifty mg/day in two divided doses is encouraged as preliminary healing slowly augmenting the dose to 600 mg/day will obtain higher efficacy gleaned from this gift case. Algorithms for medication of PDN would start with choicest glycaemic manipulate and first line medication with anticonvulsant medicinal drugs (gabapentin and pregabalin) or antidepressants (duloxetine and tricyclic antidepressants). If these cures deem inadequate for right manipulate 2nd line agents (oxycodone, tramadol, topical and sodium channel blockers) or combination cures could also be used.
Brand new pooled reports, algorithms and instructions also point out that multimodal healing procedure in peripheral neuropathic soreness may be worthy [127,128] and to which can maintain actual with the extra use of lidocaine patch and opiates in PHN. Topical medicinal drugs provide curb facet result profiles and are useful for sufferers who are unable to tolerate oral medications. Lidocaine is a voltage-gated sodium channel antagonist and when applied on the dermis binds to the sodium channels on nociceptors stopping generation and conduction of neuronal motion potentials thereby reducing agony. Lidocaine patch (5%) is authorized each in US and Europe for the healing of PHN and has few regional side results (i.e., Erythema rash dermatitis skin irritation and hypersensitivity reactions). In keeping with Barbano et al. [18] up to four 5% lidocaine patches used for up to 18 h/day could tremendously reinforce pain and great of existence for patients with PDN.
As was once modelled in this present case a randomized manages study by using Baron et al. [129] recruited sufferers with each PDN and PHN. A colossal proportion of sufferers could not be handled with monotherapy. These patients have been then requested to take a combo of lidocaine patch and pregabalin. The addition of lidocaine patch supplied better ache discount. Furthermore, pregabalin would be titrated down to a scale back dose minimizing aspect effects. Use of oxycodone in combo with pregabalin has likewise been studied in PDN with PHN [130].
While we underscore the improved chance of PHN danger in sufferers with DM, the suffering symptomatology may even pose the better crisis to a struggling sufferer with PDN. The clinician must be able to respect the predicament and not depart the sufferer to “reside with discomfort.” The procedure of awareness by means of the application of validated screening tools is vital to a better care. Nonetheless, there are occasions when the clinician’s acumen on this state of affairs is also a mission as verbal exchange gaps may just exist between them and the sufferers. This used to be once more exemplified on this reward case wherein medicinal drug (vitamin B1, B6 B12 and anti-nociceptive medicine) with unproven advantages in neuropathic suffering had been initially given. Sooner or later “two” a lot of the pains the patient suffered has been noticeably managed with cause use of combo remedies [131-150].
Conclusion
Post herpetic neuralgia (PHN) is a common and often devastatingly painful condition. It is also one of the most extensively investigated of the neuropathic pains. Patients with PHN have been studied using quantitative testing of primary afferent function skin biopsies and controlled treatment trials. Together with insights drawn from an extensive and growing literature on experimental models of neuropathic pain these patient studies have provided a preliminary glimpse of the pain-generating mechanisms in PHN. It is clear that both peripheral and central pathophysiological mechanisms contribute to PHN pain. Some PHN patients have abnormal sensitization of unmyelinated cutaneous nociceptors (irritable nociceptors). Such patients characteristically have minimal sensory loss. Other patients have pain associated with small fibre differentiation. In such patients’ pain and temperature sensation are profoundly impaired but light moving mechanical stimuli can often produce severe pain (allodynia). In these patients allodynia may be due to the formation of new connections between no nociceptive large diameter primary afferents and central pain transmission neurons [151-155]. Other differentiation patients have severe spontaneous pain without hyperalgesia or allodynia and presumably have lost both large and small diameter fibres. In this group the pain is likely due to increased spontaneous activity in deafferented central neurons and/or reorganization of central connections. These three types of mechanism may coexist in individual patients and each offers the possibility for developing new therapeutic interventions.
References
- Cohen JI. Herpes zoster. New Engl J Med. 2013;369:255-63.
- Tesfaye S, Boulton AJM, Dyck PJ, et al. Diabetic neuropathies: Update on definitions, diagnostic criteria, estimation of severity and treatments. Diabetes Care. 2010;33:2285-93.
- Suaya JA, Chen SY, Li Q, et al. Incidence of herpes zoster and persistent post-zoster pain in adults with or without diabetes. Open Forum Infect Dis. 2014;1:49.
- Guingard AP, Greenberg M, Lu C, et al. Risk of herpes zoster among diabetics: A matched cohort study in a US insurance claim database before introduction of vaccination, 1997-2006. Infection. 2014;42:729-35.
- Jambart S, Ammache Z, Haddad F, et al. Prevalence of painful diabetic peripheral neuropathy among patients with diabetes mellitus in the middle east region. J Int Med Res. 2011;39:366-77.
- Deguchi T, Rosales RL, Hashiguchi T, et al. Antiplatelet therapy, diabetic neuropathy and peripheral vascular disease: A unitary approach. J Diabetes Metab. 2012;S5:005.
- Dworkin RH, Gnann JW, Oaklander AL, et al. Diagnosis and assessment of pain associated with herpes zoster and post herpetic neuralgia. J Pain. 2008;9:S37-S44.
- Dubinsky RM, Kabbani H, El-Chami Z, et al. Practice parameter: Treatment of postherpetic neuralgia. Am Acad Neurol. 2004;63:959-965.
- Solomon CG, Cohen JI. Herpes zoster. N Engl J Med. 2013;369:255-63.
- Tyring SK (2007) Management of herpes zoster and postherpetic Neuralgia. J Am Acad Dermatol. 2007;57:S136-42.
- Javed S, Petropoulous IN, Alam U, et al. Treatment of painful diabetic neuropathy. Ther Adv Chronic Dis. 2015;6:15-28.
- Peltier A, Goutman S, Callaghan BC. Painful diabetic neuropathy. BMJ. 2014;348:1799.
- Okamoto S, Hata A, Sadaoka K, et al. Comparison of varicella-zoster virus-specific immunity of patients with diabetes mellitus and healthy individuals. J Infect Dis. 2009;200:1606-10.
- Shalayel MH, El-Agraa BE. Hyperglycemia as a predictor of postherpetic neuralgia in patients with Herpes zoster. J App Med Sci. 2013;1:661-3.
- Finnerup N, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 14:162-73.
- Bril V, England J, Franklin GM, et al. Evidence-based guideline: Treatment of painful diabetic neuropathy— report of the American Association of Neuromuscular and Electrodiagnostic Medicine, the American Academy of Neurology and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2011;76:1758-65.
- Zeigler D, Fonseca V. From guideline to patient: A review of recent recommendations for pharmacotherapy of painful diabetic neuropathy. J. Diabetes. Complications. 2015;29:145-156.
- Barbano RL, Hermann DN, Hart-Gouleau S, et al. Effectiveness, tolerability and impact on quality of life of the 5% lidocaine patch in diabetic polyneuropathy. Arch Neurol. 2004;61:914-8.
- Baron R, Mayoral V, Leijon G, et al. Efficacy and safety of combination therapy with 5% lidocaine medicated plaster and pregabalin in post-herpetic neuralgia and diabetic polyneuropathy. Curr Med Res Opin. 2009;25:77-1887.
- Zin CS, Nissen LM, Callaghan JP, et al. A randomized, controlled trial of oxycodone vs. placebo in patients with post herpetic neuralgia and painful diabetic neuropathy treated with pregabalin. J Pain. 2009;11:462-71.
- Rosales RL, Bashford G, Chaudakshetrin P, et al. Developing neuropathic pain treatment guidelines for Asia Pacific. Pain Pract. 2009;9:2-323.
- Nwasor OE, Adaji SE, Bature SB, et al. Pain relief in labor: A survey of awareness, attitude, and practice of health care providers in Zaria, Nigeria J Pain. 2011;4:27-232.
- Ness TJ, Jones L, Smith H. Use of compounded topical analgesics results of an Internet survey. Reg Anesth Pain Med. 2002;27:309-12.
- Bradley SG, Gammaitoni RG. Use of topiceuticals (topically applied, peripherally acting drugs) in the treatment of chronic pain. Curr Drug Ther. 2006;1:273-82.
- Tekelioglu UY, Apuhan T, Akkaya A, et al. Comparison of topical tramadol and ketamine in pain treatment after tonsillectomy. Paediatr Anaesth. 23:496-501.
- Holt RJ, Taiwo T, Kent JD. Bioequivalence of diclofenac sodium 2% and 1.5% topical solutions relative to oral diclofenac sodium in healthy volunteers. Postgrad Med. 2015;127:581-90.
- Peppin JF, Albrecht PJ, Argoff C, et al. Skin matters: A review of topical treatments for chronic pain. Part one: Skin physiology and delivery systems. Pain Ther. 2015;4:17-32.
- Brewer AR, McCarberg B, Argoff CE. Update on the use of topical NSAIDs for the treatment of soft tissue and musculoskeletal pain: A review of recent data and current treatment options. Phys Sportsmed. 2010;8:62-70.
- Kopsky DJ, Hesselink JMK, Bhaskar A, et al. Analgesic effects of topical ketamine. Minerva Anestesiol. 2015;81:440-9.
- Keppel HJM, Kopsky DJ, Sajben NL. Vulvodynia and proctodynia treated with topical baclofen 5 % and palmitoylethanolamide. Arch Gynecol Obstet. 2014;290:389-93.
- Kopsky DJ, Keppel HJM. Neuropathic pain as a result of acromegaly, treated with topical baclofen cream. J Pain Symptom Manage. 2013;46:e4-5.
- Kopsky DJ, Keppel HJM. High doses of topical amitriptyline in neuropathic pain: Two cases and literature review. Pain Pract. 2012;12:148-53.
- Vaegter HB, Andersen PG, Madsen MF, et al. Prevalence of neuropathic pain according to the IASP grading system in patients with chronic non-malignant pain. Pain Med. 2014;15:120-7.
- Friebel U, Eickhoff SB, Lotze M. Coordinate-based meta-analysis of experimentally induced and chronic persistent neuropathic pain. Neuroimage. 2011;58:1070-80.
- Dworkin RH, O’Connor AB, Kent J, et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. 2013;154:2249-61.
- Hubbard CS, Khan SA, Xu S, et al. Behavioral, metabolic and functional brain changes in a rat model of chronic neuropathic pain: A longitudinal MRI study. Neuroimage. 2014;107:333-44.
- Benoliel R, Eliav E, Tal M. Strain-dependent modification of neuropathic pain behaviour in the rat hind paw by a priming painful trigeminal nerve injury. Pain. 2002; 97:203-12.
- Metz AE, Yau HJ, Centeno MV, et al. Morphological and functional reorganization of rat medial prefrontal cortex in neuropathic pain. Proc Natl Acad Sci. 2009;106:2423-8.
- Borsook D, Moulton EA, Schmidt KF, et al. Neuroimaging revolutionizes therapeutic approaches to chronic pain. Mol Pain 2007;3:25.
- Scrivani S, Wallin D, Moulton EA, et al. A fMRI evaluation of lamotrigine for the treatment of trigeminal neuropathic pain: Pilot study. Pain Med. 2010;11:920–41.
- Zeidan F, Grant Ja, Brown Ca, et al. Mindfulness meditation-related pain relief: evidence for unique brain mechanisms in the regulation of pain. Neurosci Lett 2012;520:165-73.
- Zeidan F, Coghill RC. Functional connections between self-referential thought and chronic pain: A dysfunctional relationship. Pain. 2013;154:3-4.
- Bolwerk A, Seifert F, Maihöfner C. Altered resting-state functional connectivity in complex regional pain syndrome. J Pain. 2013;14:1107-15.
- Broyd SJ, Demanuele C, Debener S, et al. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev. 2009;33:279-96.
- Baliki MN, Mansour AR, Baria AT, et al. Functional reorganization of the default mode network across chronic pain conditions. PLoS ONE. 2014;9:e106133.
- Baliki MN, Geha PY, ApkarianaV, et al. Beyond feeling: Chronic pain hurts the brain, disrupting the default-mode network dynamics. J Neurosci. 2008;28:1398-1403.
- Gold C, Fachner J, Erkkilä J. Validity and reliability of electroencephalographic frontal alpha asymmetry and frontal midline theta as biomarkers for depression. Scandi J Psychol. 2012.
- Pérez-Edgar K, Kujawa A, Nelson SK, et al. The relation between electroencephalogram asymmetry and attention biases to threat at baseline and under stress. Brain Cogn. 2013;82:337-43.
- Malinen S, Vartiainen N, Hlushchuk Y, et al. (2010) Aberrant temporal and spatial brain activity during rest in patients with chronic pain. Proc Natl Acad Sci. 2010;107:6493-7.
- Ney JP, Devine EB, Watanabe JH, et al. Comparative efficacy of oral pharmaceuticals for the treatment of chronic peripheral neuropathic pain: Meta-analysis and indirect treatment comparisons. Pain Med. 2013;14:706-19.
- Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 2015;14:162-73.
- Grimaldi CR, Berrocoso E, Alba-Delgado C, et al. Stress increases the negative effects of chronic pain on hippocampal neurogenesis. Anesth Analg. 2015;121:1078-88.
- Mulla SM, Buckley DN, Moulin DE, et al. Management of chronic neuropathic pain: A protocol for a multiple treatment comparison meta-analysis of randomised controlled trials. Neurology. 2014;4:e006112.
- Elmofty DH, Anitescu M, Buvanendran A.Best practices in the treatment of neuropathic pain. Pain Manag. 2013;3:475-83.
- Bentley LD, Duarte RV, Furlong PL, et al. Brain activity modifications following spinal cord stimulation for chronic neuropathic pain: A systematic review. Eur J Pain. 2015.
- Kupers R, Kehlet H. Brain imaging of clinical pain states: A critical review and strategies for future studies. Lancet Neurol. 2006;5:1033-44.
- Reynolds C, Osuagwu BA, Vuckovic A. Influence of motor imagination on cortical activation during functional electrical stimulation. ClinNeurophysiol. 2014;126:1360-9.
- Gustin SM, Wrigley PJ, Henderson LA, et al. Brain circuitry underlying pain in response to imagined movement in people with spinal cord injury. Pain. 2010;148:438-45.
- Gustin SM, Wrigley PJ, Gandevia SC, et al. Movement imagery increases pain in people with neuropathic pain following complete thoracic spinal cord injury. Pain. 2008;137:237-44.
- Knotkova H, Cruciani RA, Tronnier VM, et al. Current and future options for the management of phantom-limb pain. J Pain Res. 2012;5:39-49.
- Moseley GL. Graded motor imagery is effective for long-standing complex regional pain syndrome: A randomized controlled trial. Pain. 2004;108:192-8.
- Arnstein P Chronic neuropathic pain: issues in patient education. Pain ManagNurs. 2004;5:34-41.
- Oberfeld E, Ammann B, Vögelin E. Therapeutic modalities influencing neuropathic pain in hand surgery patients. Ther Umschau Rev The´rapeutique. 2014;71:423-9.
- Walz AD, Usichenko T, Moseley GL, et al. Graded motor imagery and the impact on pain processing in a case of CRPS. Clin J Pain. 2013;29:276-9.
- Lagueux E, Charest J, Lefrançois-Caron E, et al. Modified graded motor imagery for complex regional pain syndrome type 1 of the upper extremity in the acute phase: a patient series. Int J Rehabil Res. 2012;35:138-45.
- Bowering KJ, O’Connell NE, Tabor A, et al. The effects of graded motor imagery and its components on chronic pain: a systematic review and meta-analysis. J Pain. 2013;14:3-13.
- Reiner K, Tibi L, Lipsitz JD.Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med. 2013;14:230-42.
- Fox KCR, Zakarauskas P, Dixon M, et al. Meditation experience predicts introspective accuracy. PLoS ONE. 2012;7:e45370.
- Garland EL, Froeliger B, Zeidan F, et al. The downward spiral of chronic pain, prescription opioid misuse and addiction: Cognitive, affective and neuropsychopharmacologic pathways. Neurosci Biobehav Rev. 2013;37:2597-607.
- Hanley AW, Garland EL. Dispositional mindfulness co-varies with self-reported positive reappraisal. Pers Individ Dif. 2014;66:46-152.
- Garland EL, Hanley A, Farb NA. State mindfulness during meditation predicts enhanced cognitive reappraisal. Mindfulness (NY). 2013;6:234-42.
- Grant Ja, Rainville P. Pain sensitivity and analgesic effects of mindful states in Zen meditators: A cross-sectional study. Psychosom Med. 2009;71:106-14.
- Grant JA. Meditative analgesia: The current state of the field. Ann N Y Acad Sci. 2014;1307:55-63.
- Allen M, Dietz M, Blair KS, et al. Cognitive-affective neural plasticity following active-controlled mindfulness intervention. J Neurosci. 2014;32:15601-10.
- Hölzel BK, Carmody J, Vangel M, et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011;191:36-43.
- Kerr CE, Sacchet MD, Lazar SW, et al. Mindfulness starts with the body: somatosensory attention and top-down modulation of cortical alpha rhythms in mindfulness meditation. Front Hum Neurosci. 2013;7:12.
- Moynihan JA, Klorman R, Chapman BP, et al. (2010) Mindfulness to improve elders’ immune and health status. Brain Behav Immun. 2010;24:1-13.
- Goyal M, Singh S, Sibinga EMS, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med. 2014;174:357-68.
- Fox KCR, Nijeboer S, Dixon ML, et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev. 2014;43C:48-73.
- Marineo G, Iorno V, Gandini C, et al. Scrambler therapy may relieve chronic neuropathic pain more effectively than guideline-based drug management: Results of a pilot, randomized, controlled trial. J Pain Symptom Manage. 2012;43:87-95.
- Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17:1113-88.
- Han B, Compton WM, Jones CM, et al. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314:1468-78.
- Chapman CR, Lipschitz DL, Angst MS, et al. Opioid pharmacotherapy for chronic non-cancer pain in the United States: A research guideline for developing an evidence-base. J Pain. 2010;11:807-29.
- Stein C, Reineche H, Sorqatz H. Opioid use in chronic noncancer pain: Guidelines revisited. Curr Opin Anaesthesiol. 2010;23:598-601.
- Melzack R, Wall PD. Pain mechanisms: A new theory. Science. 1965;150:971-979.
- Johnson MI, Walsh DM. Pain: Continued uncertainty of TENS' effectiveness for pain relief. Nat Rev Rheumatol. 2010;6:314-6.
- Sparadeo F, Kaufman C, D’Amato S. Scrambler therapy: an innovative and effective treatment for chronic neuropathic pain. J Life Care Plan. 2012;11:3-15.
- Lefaucheur JP, Andre-Obadia N, Antal A, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125:2150-206.
- Marineo G. Untreatable pain resulting from abdominal cancer: New hope from biophysics? JOP. 2003;4:1-10.
- Marineo G, Spaziani S, Sabato AF, et al. Artificial neurons in oncological pain: The potential of scrambler therapy to modify a biological information. International Congress Series. 2003;1255:381-8.
- Coyne PJ, Wan W, Dodson P, et al. A trial of Scrambler therapy in the treatment of cancer pain syndromes and chronic chemotherapy-induced peripheral neuropathy. J Pain Palliat Care Pharmacother. 2013;27:359-64.
- Smith TJ, Coyne PJ, Parker GL, et al. Pilot trial of a patient-specific cutaneous electrostimulation device (MC5-A Calmare(R) for chemotherapy-induced peripheral neuropathy. J Pain Symptom Manage. 2010;40:883-91.
- Notaro P, Dell'Agnola CA, Dell'Agnola AJ, et al. Pilot evaluation of scrambler therapy for pain induced by bone and visceral metastases and refractory to standard therapies. Support Care Cancer. 2015;24:1649-54.
- Park HS, Sin WK, Kim HY, et al. Scrambler therapy for patients with cancer pain - case series. Korean J Pain. 2013;26:65-71.
- Ko YK, Lee HY, Lee WY. Clinical experiences on the effect of scrambler therapy for patients with post herpetic neuralgia. Korean J Pain. 2013;26:98-101.
- Compagnone C, Tagliaferri F, Therapy GS. Chronic pain treatment and scrambler therapy: A multicenter retrospective analysis. Acta Biomed. 2015;86:149-56.
- Starkweather AR, Coyne P, Lyon DE, et al. Decreased low back pain intensity and differential gene expression following Calmare(R): results from a double-blinded randomized sham-controlled study. Res Nurs Health. 2015;38:29-38.
- Ricci M, Pirotti S, Scarpi E, et al. Managing chronic pain: Results from an open-label study using MC5-A Calmare(R) device. Support Care Cancer. 2012;20:405-12.
- Sabato AF, Marineo G, Gatti A. Scrambler therapy. Minerva Anestesiol. 2005;71:479-82.
- Moon JY, Kurihara C, Beckles JP, et al. Predictive factors associated with success and failure for Calmare (Scrambler) therapy: A multicenter analysis. Clin J Pain. 2015;31:750-6.
- Pachman DR, Weisbrod BL, Seisler DK, et al. Pilot evaluation of Scrambler therapy for the treatment of chemotherapy-induced peripheral neuropathy. Support Care Cancer. 2015;23:943-51.
- La Cesa S, Tamburin S, Tugnoli V, et al. How to diagnose neuropathic pain? The contribution from clinical examination, pain questionnaires and diagnostic tests. Neurol Sci. 2015;36:2169-75.
- Palmer G. Complex regional pain syndrome. AustPrescr. 2015;38:82-6.
- Callaghan BC, KerberKA, Lisabeth LL, et al. Role of neurologists and diagnostic tests on the management of distal symmetric polyneuropathy. JAMA Neurol. 2014;71:1143-9.
- Finnerup NB, Haroutounian S, Kamerman P, et al. Neuropathic pain: An updated grading system for research and clinical practice. Pain. 2016.
- Ellis A, Bennett DL. (2013) Neuroinflammation and the generation of neuropathic pain. Br J Anaesth. 2013;111:26-37.
- Odrcich M, Bailey JM, Cahill CM, et al. Chronobiological characteristics of painful diabetic neuropathy and post herpetic neuralgia: diurnal pain variation and effects of analgesic therapy. Pain. 2006;120:207-12.
- Attal N, Lanteri-Minet M, Laurent B, et al. The specific disease burden of neuropathic pain: Results of a French nationwide survey. Pain. 2011;152:2836-43.
- Dieleman JP, Kerklaan J, Huygen FJ, et al. Incidence rates and treatment of neuropathic pain conditions in the general population. 2008;137:681-8.
- Moore RA, Chi CC, Wiffen PJ, et al. (2015) Oral non-steroidal anti-inflammatory drugs for neuropathic pain. Cochrane Database Syst Rev. CD010902.
- O'Connor AB, Dworkin RH. Treatment of neuropathic pain: An overview of recent guidelines. Am J Med. 2009;122:S22-32.
- Dworkin RH, O'Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: Evidence-based recommendations. Pain. 2007;132:237-51.
- Gharibian D, Polzin JK, Rho JP. Compliance and persistence of antidepressants versus anticonvulsants in patients with neuropathic pain during the first year of therapy. Clin J Pain. 2013;29:377-81.
- Mick G, Baron R, Finnerup NB, et al. What is localized neuropathic pain? A first proposal to characterize and define a widely used term. Pain Manag. 2012;2:71-7.
- Sawynok J, Zinger C. Topical amitriptyline and ketamine for post-herpetic neuralgia and other forms of neuropathic pain. Expert Opin Pharmacother. 2016;17:601-9.
- Allegri M, Baron R, Hans G, et al. A pharmacological treatment algorithm for localized neuropathic pain. Curr Med Res Opin. 2016;32:377-84.
- Kopsky DJ, Hesselink JM. High doses of topical amitriptyline in neuropathic pain: two cases and literature review. Pain Pract. 2012;12:148-53.
- Somberg JC, Molnar J. Retrospective study on the analgesic activity of a topical (TT-CTAC) cream in patients with diabetic neuropathy and other chronic pain conditions. Am J Ther. 2015 22:214-21.
- Kopsky DJ, Keppel Hesselink JM, Bhaskar A, et al. Analgesic effects of topical ketamine. Minerva Anestesiol. 2015;81:440-9.
- Gilron I, Bailey JM, Tu D, et al. Nortriptyline and gabapentin, alone and in combination for neuropathic pain: A double-blind, randomised controlled crossover trial. Lancet. 2009;374:1252-61.
- Gilron I, Bailey JM, Tu D, et al. Morphine, gabapentin or their combination for neuropathic pain. N Engl J Med. 2005;352:1324-34.
- Siddall PJ, McClell JM, Rutkowski SB, et al. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249-57.
- Gatchel RJ, Mayer TG, Capra P, et al. Quantification of lumbar function part 6: The use of psychological measures in guiding physical function restoration. Spine. 1986;11:36-42.
- Tachibana T, Maruo K, Inoue S, et al. Use of pain drawing as an assessment tool of sciatica for patients with single level lumbar disc herniation. Springer Plus. 2016.
- Siddall PJ. Management of neuropathic pain following spinal cord injury: Now and in the future. Spinal Cord. 2009;47:352-9.
- Yezierski RP, Burchiel KJ. Progress in pain research and management, Spinal cord injury pain: assessment, mechanisms, management, Seattle. 2002;23.
- Siddall PJ, Middleton JW. A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord. 2006;44:67-77.
- Cardenas DD, Nieshoff EC, Suda S, et al. A randomized trial of pregabalin in patients with neuropathic pain due to spinal cord injury. Neurology. 2013;80:533-9.
- Li CY, Song YH, Higuera ES, et al. Spinal dorsal horn calcium channel alpha-2-delta-1 subunit upregulation contributes to peripheral nerve injury-induced tactile allodynia. J Neurosci. 2004;29:8494-9.
- Tanabe M, Takasu K, Takeuchi Y, et al. Pain relief by gabapentin and pregabalin via supraspinal mechanisms after peripheral nerve injury. J Neurosci Res. 2008;86:3258-64.
- Patel R, Bauer CS, Nieto-Rostro M, et al. Alpha-2-delta-1 gene deletion affects somatosensory neuron function and delays mechanical hypersensitivity in response to peripheral nerve damage. J Neueosci. 2013;33:16412-26.
- Borujerdi A, Zeng J, Sharp K, et al. Calcium channel alpha-2-delta-1 protein upregulation in dorsal spinal cord mediates spinal cord injury induced neuropathic pain states. Pain. 2011;152:649-55.
- Finnerup NB, Sindrup SH, Jensen TS. The evidence for pharmacological treatment of neuropathic pain. Pain. 2010;150:573-81.
- Vranken JH, Hollmann MW, Vegt MH, et al. (2011) Duloxetine in patients with central neuropathic pain caused by spinal cord injury or stroke: A randomized, double-blind, placebo-controlled trial. Pain. 2011;152:267-73.
- Mehta S, Guy S, Lam T, et al. Antidepressants are effective in decreasing neuropathic pain after SCI: A meta-analysis. Top Spinal Cord Inj Rehabil. 2015;21:166-73.
- Allen RE, Kirby KA. Nocturnal leg cramps. Am Fam Physician. 2012;86:350-5.
- Garrison SR, Dormuth CR, Morrow RL, et al. Nocturnal leg cramps and prescription use that precedes them: A sequence symmetry analysis. Arch Int Med. 2012;17:120-6.
- Mohamed M, Hayes R. Quinine-induced severe thrombocytopenia: the importance of taking a detailed drug history. BMJ Case Rep. 2013.
- Guerrera MP, Volpe SL, Mao JJ. Therapeutic uses of magnesium. Am Fam Physician. 2009;80:157-62.
- Katzberg HD, Khan AH, So YT. Assessment: Symptomatic treatment for muscle cramps (an evidence-based review): Report of the therapeutics and technology assessment subcommittee of the American academy of neurology. Neurology. 2010;7:691-6.
- Blyton F, Chuter V, Walter KE, et al. Non-drug therapies for lower limb muscle cramps. Cochrane Database Syst. 2012;Rev 1:CD008496.
- Daniell HW. Simple cure for nocturnal leg cramps. N Engl J Med. 1979;301:216.
- Keppel Hesselink JM. The terms ‘autacoid’, ‘hormone’ and ‘chalone’ and how they have shifted with time. J Autonomic Autacoid Pharmacol. 2016.
- Ambrosino P, Soldovieri MV, Russo C, et al. Activation and desensitization of TRPV1 channels in sensory neurons by the PPAR-alpha agonist palmitoyl ethanolamide. Br J Pharmacol. 201;168:1430-44.
- Bean BP, Mackinnon D, Mackinnon R. Methods and compositions for preventing and relieving muscle cramps and for recovery from neuromuscular irritability and fatigue following exercise. 2010.
- Keppel Hesselink JM, de Boer T, Witkamp RF. Palmitoylethanolamide: A natural body-own anti-inflammatory agent, effective and safe against influenza and common cold. Int J Inflam. 2013;2013:151028.
- Hesselink JM, Hekker TA. Therapeutic utility of palmitoyl ethanolamide in the treatment of neuropathic pain associated with various pathological conditions: A case series. J Pain Res. 2012;5:437-42.
- Keppel Hesselink JM. Chronic idiopathic axonal neuropathy and pain, treated with the endogenous lipid mediator palmitoyl ethanolamide: A case collection. Int Med Case Rep. 2013;Jl6:49-53.
- Hesselink JM, Kopsky DJ. Palmitoylethanolamide, a neutraceutical, in nerve compression syndromes: Efficacy and safety in sciatic pain and carpal tunnel syndrome. J Pain Res. 2015;8:729-34.
- Paladini A, Fusco M, Cenacchi T, et al. Palmitoyl ethanolamide, a special food for medical purposes, in the treatment of chronic pain: A pooled data meta-analysis. Pain Physician. 2016;19:11-24.
- Ghafouri N, Ghafouri B, Larsson B, et al. Palmitoyl ethanolamide and stearoyl ethanolamide levels in the interstitium of the trapezius muscle of women with chronic widespread pain and chronic neck-shoulder pain correlate with pain intensity and sensitivity. Pain. 201;1:1649-58.
- Minetto MA, Holobar A, Botter A, et al. Origin and development of muscle cramps. Exerc Sport Sci Rev. 2013;41:3-10.
- Esposito E, Cuzzocrea S. Palmitoylethanolamide in homeostatic and traumatic central nervous system injuries. CNS Neurol Disord Drug Targets. 2013;1:55-61.
- Abad ANA, Mir HadiKhayate MH, Nouri, et al. Effect of Salvia officinalis hydroalcoholic extract on vincristine-induced neuropathy in mice. Chin J Nat Med. 2011;9:354-8.
- Attal N, Cruccu G, Baron R, et al. European Federation of Neurological Societies: EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17:1113-88.