Research Article - Otolaryngology Online Journal (2020) Volume 10, Issue 2
Paediatric tympanoplasty: surgical outcomes and successful prognostc factors
- *Corresponding Author:
- Borges-Costa J, Otorhinolaryngology Department
Pedro Hispano Hospital, Rua Nova do Sameiro 39
4405-769, Madalena, Vila Nova de Gaia, Portugal
Tel: +351 913582058
E-mail: costa.jrb@gmail.com
Received date: December 16, 2019; Accepted date: March 05, 2020; Published date: March 12, 2020
Abstract
Introducton: Paediatric tympanoplasty (PT) is a common performed procedure with variable described success rates. There’re many factors that may in?uence the anatomic and functonal surgical outcomes and this study’s aim is to present our PT experience and to assess the factors that may in?uence the PT success. Methods: This retrospectve study is about the children who underwent tympanoplasty in our insttuton (2011-2016). The factors tested as outcome predictors were: patent age, gender, previous adenoidectomy, operated ear side, perforaton cause, site and size, infecton at the tme of surgery, middle ear mucosa state, graf material used, contralateral ear status, pre and postoperatve hearing levels and postoperatve complicatons. We defned anatomic success as an intact graf and functonal success as a minimum of 10-dB gain in the auditory threshold afer a 6 months postoperatve period.
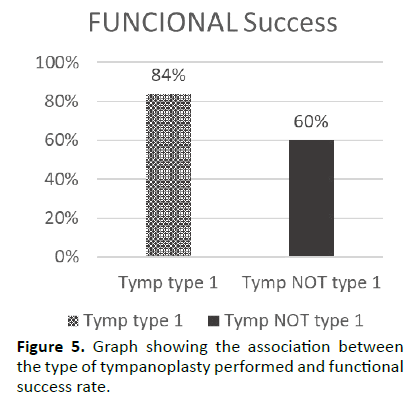
Results: Of the 60 patents and 78 procedures included, 29 were female and the patent’s mean age was 12(5) years. When only perforaton closure was considered, the success rate was 71%; however, when we measured the anatomic success plus the auditory threshold gain, the surgical success rate fell to 61%. There is a statstcally signifcant associaton between the middle ear mucosa and anatomic success rate (p=0,02) and between type of tympanoplasty performed and functonal success results (p=0,03).
Conclusions: Tympanoplasty’s the frst-line chronic otts media treatment and there’re di?erent factors that in?uence the surgical outcomes. This study should and will be complement with a bigger sample to defne the best prognosis factors. Keywords: Tympanoplasty, Paediatric tympanoplasty, Chronic otts media.
Keywords
Tympanoplasty; Paediatric tympanoplasty; Chronic otitis media.
Introduction
Chronic otitis media (COM) is a term used to describe a variety of middle-ear inflammatory diseases that commonly affects children and that, in most cases, is associated with a perforation of tympanic membrane perforation (TM). COM interferes with the hearing capacity and reduces the patient’s quality of life. Tympanoplasty techniques are the gold standard COM treatment and the main goal of surgical intervention is to remove the pathologic tissues, reconstruct TM perforation, eradicate the chronic middle ear inflammation and improve the hearing thresholds.
Although paediatric tympanoplasty (PT) is a commonly performed procedure, there are several and different success rates reported in literature, from 35% to 94% [1,2] mainly attributed to different selection criteria and success definitions. Besides that, tympanic membrane repair success in children is often behind what is typically achieved in adults with similar underlying risk factors [3]. Factors as frequent upper respiratory tract infections (URI), middle ear infections, eustachian tube dysfunction and immune system immaturity may justify the poorer children outcomes when compared to adults [4,5].
Several authors have been studying the factors that may influence the surgical outcomes in order to improve COM prognosis. One of the most studied and controversial factors is the age of children at the time of the surgery. Some scientists do not considerate age as an outcome predictor factor [6,7] and others consider that children age influence the surgical results. Based on the assumption that surgery is successful, the arguments in favour of surgery at an earlier age are: to minimize the hypoacusis and privation of aquatic activities effects; to limit the damage that chronic infection can cause to other middle ear structures; to improve quality of life, to reduce school absences and to improve children cognitive development [8-10]. On the other hand, there is evidence in the literature that delaying tympanoplasty is also a valuable option, generally until six years of age. The aspects that support this approach are: older children theoretically present better healing and immunological maturity and eustachian function, with consequent reduction of number of URI and middle ear infections; possibility of spontaneous resolution; easier surgical technique due to better anatomical development of external and middle ear structures [9,11,12]. In addition to age, other factors have been suggested as surgical outcome predictors: previous adenoidectomy, perforation cause, location and size, infection at the time of surgery, middle ear mucosa state, graft material used and contralateral ear status.
The aim of this study is to present our PT experience, to evaluate the surgical results and to determine the factors that may influence the PT success.
Materials and Methods
Children with COM who underwent tympanoplasty in our institution between January 2011 and December 2016 were retrospectively reviewed. Patients with cholesteatoma or atelectasis, patients who underwent mastoidectomy or myringoplasty and patients with craniofacial malformations were excluded. For each patient included in the study, the factors tested as outcome predictors were: patient age, gender, operated ear side, previous adenoidectomy, contralateral ear status, perforation cause, site and size, infection at the time of surgery, middle ear mucosa state, graft material used, pre and postoperative hearing levels and postoperative complications. The perforation cause was defined as post-transtympanic ventilation tube extrusion, post-recurrent middle ear infections or post-trauma. The TM were evaluated with an otomicroscopy observation one or two weeks before surgery and some characteristics were recorded: perforation site was classified as anterior, posterior, central, inferior or total; the perforation size was classified as small for those that affected <25% of TM, medium for those that affected between 25% and 50% of TM and large for those that occupied >50% of TM; contralateral ear status was registered as normal, atelectatic, simple COM or cholesteatoma. The infection at the time of surgery was defined as present or absent, the middle ear mucosa state was verified as normal or edematous/polypoid and the graft material used in surgery was temporal muscle fascia or auricular cartilage graft from tragus. Pre and postoperative audiometric pure-tone average (PTA) were calculated according to the American Academy of Otolaryngology Head and Neck Surgery [13,14].
All patients underwent underlay fascia or cartilage tympanoplasty type 1, 2 or 3 according the Portman classification [15]. A post auricular approach under general anaesthesia was used for every case. The patients were followed up and we defined anatomic success as an intact graft and functional success as a minimum of 10-dB gain in the auditory threshold after a 6 months postoperative period. The global surgical success was considered for those patients who achieved both anatomic and functional success.
All data was statistically analyzed using IBM SPSS Statistics, version 20.0, IBM Corp, Armonk, NY. Categorical variables are presented as frequencies and percentages and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distributions. Normal distribution was checked using Shapiro-Wilk test or skewness and kurtosis. Categorical variables were compared with the use of Fisher’s exact test or the qui-square test, as appropriate. Continuous variables were compared with the use of Student’s t-test or Mann-Whitney U test as appropriate.
All reported P values are two-tailed, with a P value of 0.05 indicating statistical significance. Categorical variables are presented as frequencies and percentages and continuous variables as means and standard deviations (SD) [mean ± SD] or medians and interquartile range (IQR) [median (IQR)] for variables with skewed distributions. Normal distribution was checked using Shapiro-Wilk test or skewness and kurtosis.
Results
The study sample was composed by 60 patients and 78 procedures. Thirty-one patients (51.7%) were male, 29 patients (48.3%) were female, the median age was 12(5) years, with a minimum of 7 and a maximum of 17 and 19 were ≤ 10 years old at the time of surgery. Fifty patients (64.1%) underwent previously to adenoidectomy and the right ear was the operated ear in 45 patients (57.7%). Fortyfive patients’ perforation (57.7%) was the result of repeated otological infections, for 32 patients (41%) the perforation resulted from transtympanic ventilation tube extrusion and in one case (1.3%) the perforation was a post-traumatic perforation consequence.
Thirty-one ears (39.7%) exhibited anterior perforations, 33 ears (42.3%) exhibited posterior perforations, 8 ears (10.3%) presented with inferior perforations and 6 individuals (7.7%) had a central perforation in preoperative microscopic observation. Of the perforations, 16 (20.5%) were small, 55 (70.5%) were medium and 7 of them (9%) were large. Forty-three (51.1%) patients' contralateral ears were identified as normal, 25 patients (32.1%) presented bilateral COM and 10 patients (12.8%) presented an atelectatic contralateral ear. At the time of surgery, 70.5% of ears (55) presented purulent otorrhea and the middle ear mucosa was found normal in 48 ears (61.5%). Fifty-eight ears included (74.4%) presented with a normal and totally functional ossicular chain, for which they were submitted to tympanoplasty type 1; 20 ears (25.6%) presented ossicular chain anomalies at the time of the surgery and 15 of them (19.2%) were submitted to tympanoplasty type 2 and the remaining 5 (6.4%) were submitted to tympanoplasty type 3.
Temporal fascia was the graft material used in 44 ears (56.4%) and in the remaining 34 ears (43.6%) the tragus cartilage was used to repair the TM defect. The median pre and postoperative PTA was 35(15) dB and 20(15) dB respectively and there was a statistical difference between both measurements (p<0.001). According to the definition of surgical success, after at least 6 months of follow-up, in this bigger group of patients the functional success rate achieved was 78.2% (61 ears) and the anatomic success rate was 71.8% (56 ears). However, when it was considered the group of patients with perforation closure and auditory threshold gain, the global surgical success rate fell to 61.5% (48 ears). The descriptive statistics are summarized in Table 1.
| Successful Prognostic Factors Studied | 60 patients; 78 procedures |
|---|---|
| Age - yrs | 12 (5) |
| Min | 7 |
| Max | 17 |
| Male - no. (%) | 31 (51.7) |
| Right - no. (%) | 45 (57.7) |
| - no. (%) | 50 (64.1) |
| - no. (%) | |
| Normal | 43 (51.1) |
| Atelectatic | 10 (12.8) |
| Simple COM | 24 (30.8) |
| Cholesteatoma | 1 (1.3) |
| no. (%) | |
| < 25% | 16 (20.5) |
| 25-50% | 55 (70.5) |
| > 50% | 7 (9) |
| no. (%) | |
| Anterior | 31 (39.7) |
| Posterior | 33 (42.3) |
| Inferior | 8 (10.3) |
| Central | 6 (7.7) |
| Total | 0 (0) |
| no. (%) | |
| Infectious | 45 (57.7) |
| Post-TV extrusion | 32 (41) |
| Traumatic | 1 (1.3) |
| Active no. (%) | 55 (70.5) |
| - no. (%) | |
| Normal | 48 (61.5) |
| Edematous/ polypoid | 30 (39.5) |
| – no. (%) | |
| Tymp. type 1 | 58 (74.4) |
| Tymp. type 2 | 15 (19.2) |
| Tymp. type 3 | 5 (6.4) |
| - no. (%) | |
| Temporal fascia | 44 (56.4) |
| Tragus cartilage | 34 (43.6) |
| dB | 35 (15) |
| dB | 20 (15) |
| - no. (%) | |
| Functional | 61 (78.2) |
| Anatomic | 56 (71.8) |
| Surgical | 48 (61.5) |
Table 1. Summary of descriptive analyses.
No significantly association was found between surgery outcomes and factors as patient gender, previous adenoidectomy, operated ear side, contralateral ear status, perforation cause, site and size, infection at the time of surgery and graft material used (Table 2).
| Funct Success | P-value Anat Success | Surg Success | |
|---|---|---|---|
| Gender | p=0.41 | p=0.31 | p=0.35 |
| Previous Adenoidectomy | p=0.10 | p=0.64 | p=0.55 |
| Operated ear side | p=0.65 | p=0.88 | p=0.89 |
| Contralateral ear status | p=0.73 | p=0.23 | p=0.19 |
| Perforation size | p=0.37 | p=0.18 | p=0.84 |
| Perforation site | p=0.68 | p=0.82 | p=0.93 |
| Perforation cause | p=0.73 | p=0.69 | p=0.57 |
| Infection at the time of surgery | p=0.55 | p=0.79 | p=0.94 |
| Graft material used | p=0.82 | p=0.42 | p=0.61 |
Table 2. Summary of p-values of non-statistically significant associations.
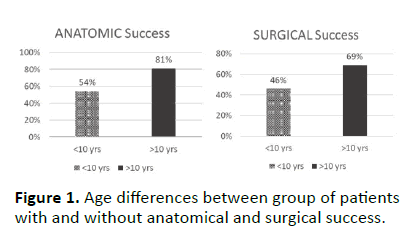
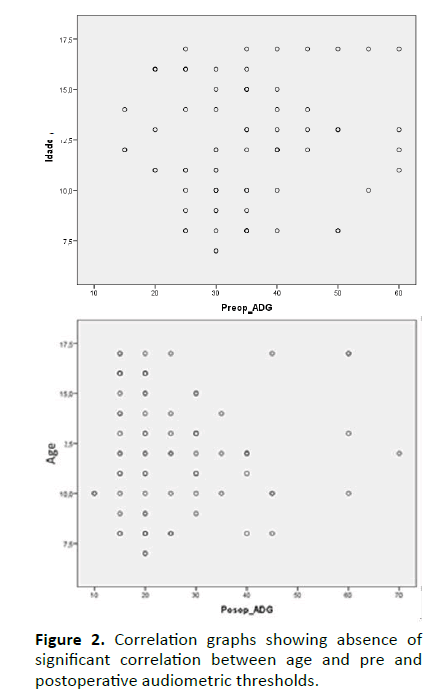
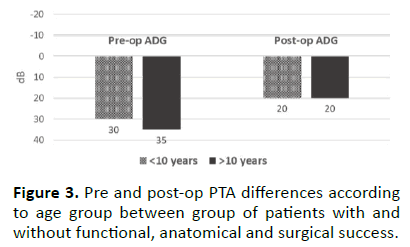
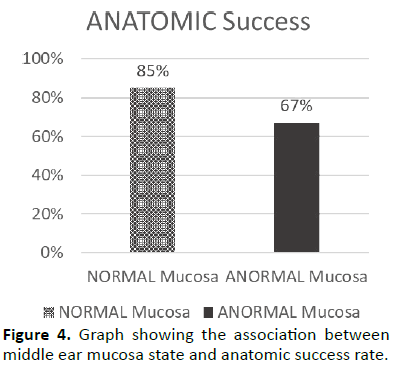
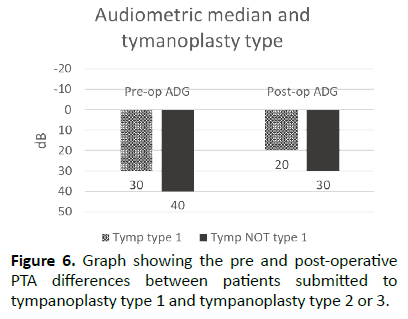
Using the Levene test, it was possible to realize that the median age of patients with functional success didn’t significantly differ from patients without success (p=0.72; Table 3). However, the median age of anatomic or surgical well succeed patients was significantly different of patients without those types of success, in a way that older patients had better outcomes than younger ones (p=0.04; p=0.02; Table 3). Accordingly, using age as a categorical variable by dividing into age groups (≤10 and >10 years), it was found a statistically association between the age groups and the anatomic and surgical success rates [p=0.01, OR=0.28 (0.09-0.78); p=0.04, OR=0.38 (0.14-1.00); Figure 1]. Relating age to median pre or postoperative PTA, it was possible to realize that regardless of using age as a continuous or categorical variable through age groups, there was no a statistically significant correlation (p=0.58; p=0.74; Figure 2) or a significantly difference respectively (p=0.73; p=0.88; Figure 3). Two more statistically significant associations were also found: patients with normal middle ear mucosa at the time of the surgery reached better anatomic success rate than patients with abnormal middle ear mucosa [p=0.02; OR=0.26 (0.08-0.86); Figure 4]; the type of tympanoplasty performed was significantly associated to the functional success rate [p=0.03; OR=0.28 (0.09-0.86)] in a way that patients submitted to tympanoplasty type 1 achieved more significant improvements in the auditory threshold than patients submitted to other types of tympanoplasty (Figure 5). Accordingly, the postoperative PTA median was statistically different between patients submitted to tympanoplasty type 1 and patients submitted to tympanoplasty type 2 or 3 (p=0.03; Figure 6).
| Age (yrs) | |
|---|---|
| Functional success | 12(5) |
| Without functional success | 12(4) |
| Anatomical success | 12(6) |
| Without anatomical success | 10(4) |
| Surgical success | 13(6) |
| Without surgical success | 11(4) |
Table 3. Age differences between group of patients with and without functional, anatomical and surgical success.
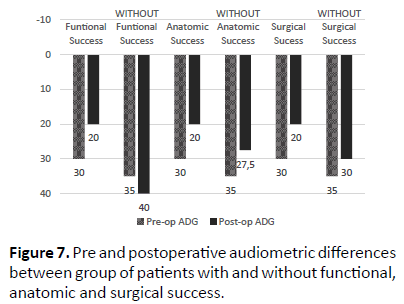
The preoperative PTA median of patients with functional, anatomical and global surgical success didn’t significantly differ from preoperative PTA median of patients without any of those types of success (p=0.15, p=0.73, p=0.36 respectively; Table 4 and Figure 7). Different patients that didn't achieved a minimum of 10dB gain in the auditory threshold after at least 6 months of follow up (p<0.001; Table 4 and Figure 7). Furthermore, the surgical well succeed patients presented a postoperative PTA significantly higher than those who didn't reach the functional gain and the perforation closure after 6 months of follow up (p<0.001; Table 4 and Figure 7). The considered measurement wasn’t statistically different between patients with and without anatomic success (p=0.07; Table 4 and Figure 7). No major complication was identified in this sample.
| Pre-op ADG (dB) | Post-op ADG (dB) | |
|---|---|---|
| Funcional success | 30(15) | 20(10) |
| Without funcional success | 35(15) | 40(30) |
| Anatomical success | 30(15) | 20(15) |
| Without anatomical success | 35(10) | 27,5(16) |
| Surgical success | 30(15) | 20(10) |
| Without surgical success | 35(10) | 30(21) |
Table 4. Pre and postoperative audiometric differences.
When the postoperative PTA mean was observed, we realized that the postoperative PTA mean of patients with functional success was statistically results are in line with the studies that defend that tympanoplasty may be delayed and performed in older children, once theoretically those are associated with improvement of eustachian function, lower rates of URI and middle ear infections and better healing and immunologic capacities. However, it can’t be ignored that these.
Discussion
Tympanoplasty is a relatively common procedure in childhood and it’s the first-line COM treatment. There are several published studies that identify several factors that may positively or negatively influence the surgical outcomes. Although age was believed to be one of the most important prognostic factors for tympanoplasty, there isn’t yet a consensus about the best surgical age for tympanoplasty in children. Some authors suggest that submitting young children (age <8 years) to tympanoplasty is a poor prognostic factor [1]; other authors suggest that age doesn’t interfere with surgical results [7,15]. In this study, it was possible to realize that the youngest children operated in our institution between 2011 and 2016 was 7 years old and that age was considered a successful prognostic factor in a way that older children achieved better perforation closure and surgical success rates regardless age is studied as a continuous or categoric variable. In fact, being > 10 years old had almost 4 times the odds to be anatomically well succeeded and almost 3 times the odds to accomplish surgical success than patient’s ≤ 10 years old.
These results may be justified by the fact that the group of patients with > 10 years is significantly bigger than the group of younger children (41 versus 19 patients) and that may influence the statistical results. Implementing the habit of operate children earlier in our institution and then creating two balanced patient groups splitted into different cutoff points would probably allow to confirm these results or to draw other conclusions.
In respect of the other factors studied, although there are authors as Vartiainen [16] that reported a higher graft success rate in girls, we didn’t find a statistically significant association between gender and surgical outcomes. The operated ear side didn’t also influence surgical results.
Some variables such as status of the contralateral ear, previous adenoidectomy and Eustachian tube function are usually analysed together by their associations with otitis media with effusion (OME) and its possible influence on paediatric tympanoplasty [17]. Caylan et al. [1] described that bilateral COM, contralateral tympanic retractions or OME were associated with lower surgery success rate; on the other hand, Vartiainen [16] found no correlation between contralateral ear status and surgical outcomes. Our results were similar to those, as there wasn’t an effect of contralateral ear status or previous adenoidectomy on surgical results.
The cause, size and location of the perforation are objective findings that have been commonly registered in the literature. Recent studies haven’t found a location effect on the surgical outcomes. Concerning the perforation size, there are some contradictory opinions: some authors defend that smaller perforations are associated with higher success rates [18] while other writers don’t find any influence on results. In this study, none of the above 3 parameters were associated with our institution tympanoplasties results.
Concerning the middle ear mucosa state at the time of the surgery, it’s known that pathological modifications of the middle ear mucosa may be justified by a chronic and prolonged inflammatory process that may be present in poor controlled COM cases. Morphological changes such as edema, polypoid aspect, granulations, fibrosis, tympanosclerotic plaques or bone lesions may be present [19]. Those influence the gas exchange, contribute to a eustachian disfunction and consequently to an insufficient middle ear and mastoid ventilation, leading eventually to tympanic retractions and perforations. Several authors described that when the mucosa was intraoperatively assessed as normal, this was a positive prognostic factor for the hearing outcome [20,21] and the poorest results were observed when mucosa was described as inflamed and fibrotic. Accordingly, our experience showed that having a normal middle ear mucosa at the surgery improved the perforation closure probability after 6 months of follow up from 67% for patients with abnormal mucosa to 85% for patients with normal mucosa. Therefore, having a normal mucosa ate the surgery had almost 4 times the odds to be anatomically well succeed than patients with pathologic mucosa. Even though most patients had normal mucosa, the number of patients with purulent otorrhea at the time of surgery was considerable. This discrepancy may result from registration errors or may be related to short episodes of purulent otorrhea insufficient to modify the state of the mucosa of the middle ear. The presence or absent of purulent otorrhea at the surgery didn’t significantly influence the surgical results.
The tympanoplasty type performed can’t be certainly predicted based on the preoperative findings. Only during surgery, depending on the state and the need for reconstruction of the ossicular chain, is the type of tympanoplasty performed defined, for which it can’t be considered a real prognostic predictor factor. Knowing that tympanoplasty type 1 is performed in patients that present during surgery an integral and mobile ossicular chain, it makes sense that, in the sample studied, those patients showed better pre and postoperative PTA medians than patients that presented an abnormal ossicular chain and needed some ossicular reconstruction or a prothesis application. Besides that, for the same reason, it’s also logical that tympanoplasty type 1 patients had almost 4 times the odds to be functionally well succeeded than patients with a disrupted ossicular chain.
Several graft materials have been used in tympanoplasty. Temporal muscle fascia is the most frequently used Graft material [22] but the use of cartilage is increasing, once that it’s apparently more resistant to infections, retractions and reperforations than temporal fascia [23]. Although the perforation closure rate of cartilage tympanoplasty is relatively higher than that of fascia according to some studies [24], there are still some concerns and controversy about its use because some researchers believe that cartilage may negatively interfere with postoperative hearing levels since it’s a thicker and a more rigid material than fascia. The controversy about this keeps going: Dornhoffer [25] compared audiological results of patients submitted to fascia and cartilage tympanoplasty and didn’t find a statistically significant difference; Yetiser and Hidir [22] reported that the auditory gain was higher in the group of cartilage patients; and Bozdemir et al. [26] published worse hearing outcomes with cartilage grafts. This study results are like those descripted by Dornhoffer [25], once no statistically significant differences were found between the graft material used and the functional, anatomical or global surgical success.
Conclusion
Anatomic and functional outcomes of paediatric tympanoplasty are quite satisfactory and our surgical success rates are concordant with those described in literature. This study is limited by the sample size and the fact that this is a retrospective study, without a control group also limits the results. Therefore, it should be done an effort to keep the investigation on to determine all the factors that influence the surgical results and, through this knowledge, obtaining the best possible surgical outcomes.
Conflict of Interest Statement
The authors whose names are listed certify that they have NO affiliations with or involvement in any organization or entity with any financial or nonfinancial interest in the subject matter or materials discussed in this manuscript.
References
- Caylan R, Titiz A, Falcioni M, et al. Myringoplasty in children: factors influencing surgical outcome. Otolaryngo Neck Surg. 1998;118(5):709-13.
- Lin AC, Messner AH. Pediatric tympanoplasty: factors affecting success. Curr Opin Otolaryngol Head Neck Surg. 2008;16(1).
- Lancaster JL, Makura ZGG, Porter G, et al. Paediatric tympanoplasty. J Laryngol Otol. 1999;113(7):628-32.
- Bluestone CD, Cantekin EI, Douglas GS. Eustachian tube function related to the results of tympanoplasty in children. Laryngoscope. 1979;89(3):450-58.
- Vrabec JT, Deskin RW, Grady JJ. Meta-analysis of pediatric tympanoplasty. Arch Otolaryngol Nec Surg. 1999;125(5):530-34.
- Umapathy N, Dekker PJ. Myringoplasty: Is it worth performing in children?. Arch Otolaryngol Neck Surg. 2003;129(10):1053-5.
- Carr MM, Poje CP, Nagy ML. Success rates in paediatric tympanoplasty. J Otolaryngol. 2001;30:199-202.
- Uyar Y, Keleş B, Koç S, et al. Tympanoplasty in pediatric patients. Int J Pediatr Otorhinolaryngol. 2006;70(10):1805-9.
- Singh GB, Sidhu TS, Sharma A, et al. Tympanoplasty type I in children - an evaluative study. Int J Pediatr Otorhinolaryngol. 2005;69(8):1071-6.
- Chandrasekhar SS, House JW, Devgan U. Pediatric tympanoplasty: A 10-year experience. Arch Otolaryngol Neck Surg. 1995;121(8):873-8.
- Pignataro L, Grillo della Berta L, Capaccio P, et al. Myringoplasty in children: anatomical and functional results. J Laryngol Otol. 2001;115(5):369-73.
- Tos M, Orntoft S, Stangerup SE. Results of Tympanoplasty in Children after 15 to 27 Years. Ann Otol Rhinol Laryngol. 2000;109(1):17-23.
- Gurgel RK, Jackler RK, Dobie RA, et al. A New Standardized Format for Reporting Hearing Outcome in Clinical Trials. Otolaryngol Neck Surg. 2012;147(5):803-7.
- Yung M, Neumann C, Vowler SL. A Longitudinal Study on Pediatric Myringoplasty. Otol Neurotol. 2007;28(3).
- Portmann M, Portmann D. Techniques of tympanomastoidectomy. Otolaryngol Clin N Am. 1989;22:29-40.
- De Vos C, Gersdorff M, Gérard J-M. Prognostic Factors in Ossiculoplasty. Otol Neurotol. 2007;28(1).
- Gurr A, Hildmann H, Stark T. Die Therapie der Tympanosklerose. HNO. 2008;56(6):651-8.
- RJ B. Basic considerations for success in tympanoplasty. Arch Otolaryngol. 1969;90(6):732-41.
- Vartiainen E, Vartiainen J. Tympanoplasty in Young Patients: The Role of Adenoidectomy. Otolaryngol Neck Surg. 1997;117(6):583-5.
- Charlett SD, Knight LC. Pediatric Myringoplasty: Does Previous Adenoidectomy Improve the Likelihood of Perforation Closure? Otol Neurotol. 2009;30(7).
- Lee P, Kelly G, Mills RP. Myringoplasty: does the size of the perforation matter?. Clin Otolaryngol Allied Sci. 2002;27(5):331-4.
- Yetiser S, Hidir Y. Temporalis Fascia and Cartilage-Perichondrium Composite Shield Grafts for Reconstruction of the Tympanic Membrane. Ann Otol Rhinol Laryngol. 2009;118(8):570-4.
- Schuknecht HF, Shi S-R. Surgical pathology of middle ear implants. Laryngoscope. 1985;95(3):249-58.
- Albirmawy OA. Comparison between cartilage-perichondrium composite ‘ring’ graft and temporalis fascia in type one tympanoplasty in children. J Laryngol Otol. 2010;124(9):967-74.
- Dornhoffer JL. Hearing Results With Cartilage Tympanoplasty. Laryngoscope. 1997;107(8):1094-9.
- Bozdemir K, Kutluhan A, Yalçıner G, et al. Tympanoplasty with Island Cartilage or Temporalis Fascia: A Comparative Study. ORL. 2012;74(1):28-32.