Research Article - Journal of Clinical Dentistry and Oral Health (2017) Oral Medicine and Surgery
Orofacial bone complications in thalassemic children associated with cephalometric evaluation
Murat Tutanc1*, Elif Guler Kazanc2, Tugba Colak3 and Erhan Yengil4
1Department of Pediatrics, Yuksek Ihtisas Training and Research Hospital, Bursa, Turkey
2Department of Pediatric Hematology, Yuksek Ihtisas Training and Research Hospital, Bursa, Turkey
3Department of Orthodontics, Dentistry Faculty of Kırıkkale University, Kırıkkale, Turkey
4Department of Family Medicine, Medical School of Mustafa Kemal University, Hatay, Turkey
- *Corresponding Author:
- Murat Tutanc
Yuksek Ihtisas Training and Research Hospital
Department of Pediatrics
Bursa, Turkey
Tel: +90 555 380 34 84
E-mail: drtutanc@hotmail.com
Accepted on November 29, 2017
Citation: Tutanc M, Kazanc EG, Colak T, et al. Orofacial bone complications in thalassemic children associated with cephalometric evaluation. J Oral Med Surg 2017;1(1):23-26.
Abstract
Introduction: Beta Thalassemia (BT) disorders are characterized by a genetic abnormality in the compound of beta-globin chains, one of the most common hereditary diseases in Turkey and worldwide. Some of the characteristic orofacial complication of BT is associated with bone structure. Material and method: Thalassemic and control groups selected retrospectively from the archives of Dortcelik Pediatric Hospital, Bursa. Cephalometric measurements were used in the current study. All statistical analyses were conducted using student’s-test and Mann-Whitney U test. Results: Significant findings were shorter SNB angles, greater ANB angles, greater condylion to point A sizes, protrusive upper lips, shorter interincisal angles, greater value of wits, shorter interincisial angle, greater U1-NA, shorter anterior face height (NaMe), shorter posterior face height (SGo) are significantly in thalassemic patients (n: 26). All measurements have indicated affected orofacial structure. Conclusions: Orofacial complication due to bone structure development in thalassemic patients is pronounced. Distinct findings are treated by orthodontics. When orofacial intervention is applied, the complications were evaluated. All treatments must be controlled by a hematologist.
Keywords
Thalassemia, Developmental toxicology, Orofacial complications.
Introduction
Beta-thalassemia major (BT) is considered one of the most prevalent genetic anomalies in the world, including in countries like Turkey [1,2]. These are a group of hereditary blood disorders characterized by abnormalities in the composition of the beta chains of hemoglobin. The total annual Beta-thalassemia incidence of symptomatic individuals is estimated at 1 in 100,000 in worldwide and 1 in 10,000 people in the European Union [3].
The patients of BT usually come to medical practice within the initial years of life and require successive RBC transfusions to stay alive. The clinical feature of BT in serious findings include growth retardation, pallor, jaundice, poor musculature, genu valgum, hepatosplenomegaly, leg ulcers, extramedullary hematopoiesis, and skeletal deformities caused by enlargement of the bone marrow.
The deformities involve changes in the long bones of the legs and distinctive craniofacial changes (bossing of the skull, prominent malar eminence, depression of the bridge of the nose, tendency to a mongoloid slant of the eye, and hypertrophy of the maxillae, which tends to expose the upper teeth) [4-7]. The distinctive features of orofacial findings of BT are prominent cheekbones and protrusive premaxilla. Cephalometric analysis reveals dilatation of the diplopic space, subperiostal bone grows, partialy oblitered maxillary sinus. The findings are due to extra medullar erythroid hyperplasia [8-11].
According to our knowledge, scarcely any detailed studies on craniofacial measurements and deformities in thalassemic population have been published. We aimed to perform cephalometric analysis of patients with thalassemic patients consistent with the most widely-known orofacial clinical manifestations.
Materials and Methods
Records of talasemia patients and heath individuals (control group) were selected retrospectively from the archives of Dortcelik Pediatric Hospital. Selection criteria included no previous orthodontic treatment and having cephalometric films and records for talasemia, age and sex mismatch. A control group was selected from records of Class I malocclusion patients with no systemic disease who came to the dentistry clinic of Dortcelik Pediatric Hospital.
Standardized lateral cephalograms of 26 talasemia patients (17 girls, 9 boys) and age and sex-matched 30 healthy individuals that had been taken with the same digital cephalometric imaging system (Blue X Imaging Srl, Assango, Italy) in a natural head position were selected. Cranial and dentofacial parameters were measured using a cephalometric analysis program (Nemoceph Imaging Cephalometric and Tracing Software S.L, Spain).
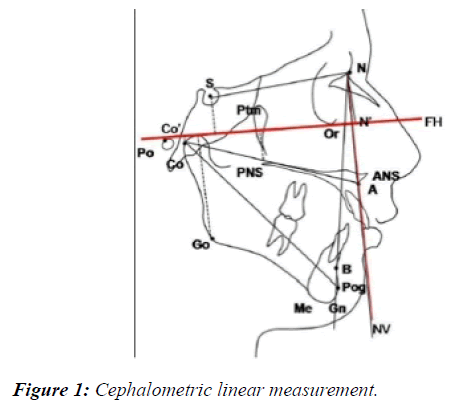
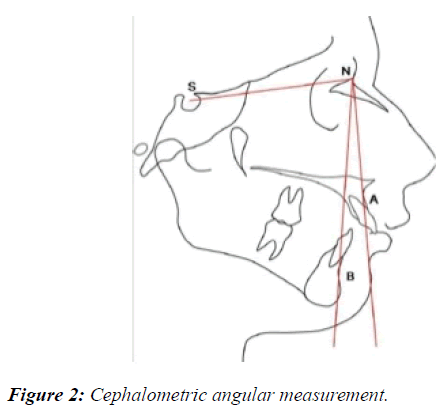
A total of 26 measurements were performed on the lateral cephalograms. Cephalometric landmarks were marked and digitized by one of the authors. Cephalomtric reference points and planes used in the study are shown in Figures 1 and 2. Used in cephalometric landmarks are listed in Table 1 [12].
| N | The most anterior point of the nasofrontal suture on midsagital plane |
| S | The center of the hypophyseal fossa |
| A | Deepest point on midsagitalplane between ANS and prosthion |
| B | The deepest midlinepoint on the mandible in the median plane |
| Go | A posterio-inferiorpoint of the ramus |
| Gn | The most anterio-inferior point of the bony chin |
| Me | Most inferior point on the symphysis of the mandible in the median plane |
| U1 | The most point on the margin of the upper membranous lip |
| L1 | The most point on the margin of the lower membranous lip |
| Co | The most posterio-superior point of the condyle of the mandible |
| Wits | From points A and B to the occlusal plane |
| Pog | The most anterior point on the soft tissue chin in the midsaggital plane |
Table 1: Cephalometric landmarks.
Statistical method
All statistical analyses were conducted using SPSS version 13.0 (Statistical Package for Social Sciences). Student’s-test and Mann-Whitney U test was used on between-group comparisons. All statistical data, p<0.05 was accepted as significant.
Results
Thalassemic patients (n:26) mean age is 14.07 ± 3.27 and control group mean age is 12.57 ± 2.76. Either group’s ages were the same. (p=0.068). Sex ratio of patients was M/F, 9 (34.6%)/ 17(65.4%), and control group was M/F 14 (46.7%)/ 16(53.3%). Either group was same for sex. (p=0.361).
Cephalometric measurements and the relationship between patient and control groups were summarized in Table 2. SNB (p=0.001) angles were significantly shorter in the thalassemic group while ANB (p=0.0001) angles were significantly greater. Posterior face height (SGo) (p=0.025), and P-A face height (%) (p=0.033) were significantly shorter. Condylion to point A sizes were significantly greater. The upper lips were protrusive (p=0.013). The interincisal angles were significantly shorter (p=0.047). Value of wits were significantly greater (p=0.0001). Interincisial angles were significantly shorter (0.047). U1-NA measurements were significantly greater (p=0.016).
| Parameter | Thalassemic Patients | Healthy Individuals | P | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Minumum | Maximum | Mean | SD | Minumum | Maximum | ||
| ANB (º) | 5.43 | 2.41 | -1.5 | 9.5 | 1.89 | 1.71 | -0.5 | 5.3 | 0.0001* |
| SNA (º) | 79.5 | 3.45 | 70.6 | 85 | 78.82 | 2.52 | 75.2 | 83.8 | 0.398* |
| SNB (º) | 74.07 | 3.48 | 65.4 | 79.1 | 76.9 | 2.6 | 70.1 | 82.2 | 0.001* |
| GoGn-SN | 34.93 | 6.66 | 15 | 49 | 33.65 | 4.89 | 24.6 | 43.3 | 0.412* |
| Anterior face height (NaMe) | 106.7 | 8.38 | 90 | 125 | 108 | 5.97 | 97 | 121 | 0.513* |
| Posterior face height (SGo) | 65.69 | 5.37 | 54 | 77 | 69.03 | 5.46 | 56 | 81 | 0.025* |
| P-A face height (%) | 61.69 | 3.93 | 54 | 68 | 64.03 | 4.03 | 55 | 72 | 0.033* |
| Lower anterior facial height | 61.96 | 6.72 | 48 | 77 | 61.03 | 4.92 | 52 | 71 | 0.554* |
| Ramus height | 38.38 | 3.99 | 32 | 48 | 40.06 | 3.54 | 32 | 49 | 0.100* |
| Mandibular body | 63.69 | 5.12 | 54 | 75 | 64.1 | 4.05 | 57 | 72 | 0.741* |
| Condylion to point A | 78.03 | 5.19 | 64 | 88 | 74.43 | 4.82 | 63 | 84 | 0.009* |
| Anterior cranial base length | 63.69 | 3.6 | 56 | 71 | 62.6 | 3.14 | 57 | 70 | 0.231* |
| Condylion to gnathion | 97.73 | 10.4 | 64 | 114 | 99.83 | 6.02 | 85 | 112 | 0.350* |
| Nasolabial angle | 103.8 | 12.7 | 78 | 130 | 105 | 10 | 90 | 129 | 0.695* |
| Upper lip protrusion | -0.92 | 2.57 | -5 | 4 | -2.33 | 1.44 | -5 | 0 | 0.013* |
| Lower lip protrusion | 0.96 | 3.03 | -5 | 8 | 1.66 | 11.7 | -4 | 63 | 0.064** |
| Wits | 2.3 | 2.6 | -4 | 7 | -2.23 | 2.29 | -7 | 1 | 0.0001* |
| Interincisal angle | 129.7 | 5.86 | 120.8 | 142.7 | 133.3 | 7 | 117 | 148.7 | 0.047* |
| U1-NA (mm) | 3.15 | 1.43 | 1 | 6 | 4.03 | 1.21 | 2 | 6 | 0.016* |
| L1-NB (mm) | 4.6 | 2.17 | 1 | 9 | 3.8 | 1.25 | 1 | 6 | 0.114* |
| Pog-NB (mm) | 1.15 | 1.15 | -2 | 4 | 1.46 | 1.25 | -2 | 4 | 0.338* |
*Student’s t test **Mann-Whitney U test
Table 2: Comparsion of the cephalometric variables.
Discussion
Cephalometric characteristics of thalassemic patients are very important for orofacial application such as orthodontics. Reports of orofacial complications of thalasemic patients are inadequate in the literature. These complications are important for orthodontic and surgical procedures in the patients [13-15].
Significant greater ANB angles in thalassaemia major patients attributed to a short mandible. This finding was consistent with the literature [13-15]. The SNB measurements have shown mandibular regression and increase in the thickness of the soft tissue of the chin in thalassemic kids. Short mandibles were reported in thlassemic patients some of our findings were associated with a short mandible [13-16].
Shortness of SGo and P-A face height was founded. These findings were similar to literature [13,15].
The condylion to point A measurement and upper lip protrusion in thalassemic patients show maxillary protrusion. These findings contribute to the typical appearance of thalassemic patients [11,17]. Differently, Abu Alhaija et al. and Amini claimed normal Maxilla length of thalassemic patients [12,13]. The porgnathism was attributed by a short mandible and a short cranial base length according to their articles [13,14]. We found long U1-NA measurements and normal cranial base lengths in thalassemic patients. We think that maxillary protrusion is due to thalassemia complications.
Increases in the angle of ANB in the thalassemic patients reveal an expansive intermaxillary discrepancy. This finding was consistent with the literature [13]. Interincisal angles and wits associated with the biting process are affected in thalassemic patient. We came across similar findings in the literature, but not exact matches [7,13].
Orofacial abnormalities in these patients are important in three aspects. Firstly, hemoglobin values of these patients need to be kept at an optimal level (base line of hemoglobin level between 9 and 10 gr/dL). This application will reduce the occurrence orofacial complications [13,18,19]. Secondly, orofacial complications should be treated by an orthodontist. Cephalometric evaluation must be done during orthodontic treatment. Characteristic complications of thalassemic patients are well known. This knowledge is necessary for any orofacial intervention. And finally, all treatment plans should be consulted to a hematologist.
References
- Karimi M, Haghpanah S, Taher AT, et al. β-Thalassemia: New Therapeutic Modalities, Genetics, Complications, and Quality of Life. Anemia. 2012: 902067.
- Guvenc B, Canataroglu A, Unsal C, et al. β-Thalassemia mutations and hemoglobinopathies in Adana, Turkey: results from a single center study. Arch Med Sci. 2012:8(3):411-14.
- Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010;5:11.
- Cappellini MD, Cohen A, Porter J, et al. Guidelines for the Management of Transfusion Dependent Thalassaemia. Thalassemia International Federation 2014.
- Haidar R, Musallam KM, Taher AT. Bone disease and skeletal complications in patients with beta thalassemia major. Bone. 2011;48(3):425-32.
- Wonke B. Bone disease in beta-thalassaemia major. Br J Haematol. 1998.103(4):897-901.
- Hattab FN, Y OM. Dental arch dimensions in subjects with beta-thalassemia major. J Contemp Dent Pract. 2011; 12(6):429-33.
- Weel F, Jackson IT, Crookendale WA, et al. A case of thalassaemia major with gross dental and jaw deformities. Br J Oral Maxillofac Surg. 1987;25(4):348-52.
- Van Dis ML, Langlais RP. The thalassemias: oral manifestations and complications. Oral Surg Oral Med Oral Pathol. 1986;62(2):229-33.
- Hattab FN. Patterns of physical growth and dental development in Jordanian children and adolescents with thalassemia major. J Oral Sci. 2013;55(1):71-7.
- Danjou F, Anni F, Galanello R. Beta-thalassemia: from genotype to phenotype. Haematologica. 2011;96(11):1573-5.
- Yildırım E, Olmez H, Gorgulu S, et al. Evaluation of differences between two and three-dimensional cephalometric measurements. Gulhane Med J. 2011;53(1):43-49.
- Abu Alhaija ES, Hattab FN, MA al-Omari. Cephalometric measurements and facial deformities in subjects with beta-thalassaemia major. Eur J Orthod. 2002;24(1):9-19.
- Amini F, Jafari A, Eslamian L, et al. A cephalometric study on craniofacial morphology of Iranian children with beta-thalassemia major. Orthod Craniofac Res. 2007;10(1):36-44.
- Bassimitci S, Yucel-Eroglu E, Akalar M. Effects of thalassaemia major on components of the craniofacial complex. Br J Orthod. 1996;23(2):157-62.
- Hazza'a AM, Al-Jamal G. Radiographic features of the jaws and teeth in thalassaemia major. Dentomaxillofac Radiol. 2006;35(4):283-8.
- Toman HA, Nasir A, Hassan R. Skeletal, dentoalveolar, and soft tissue cephalometric measurements of Malay transfusion-dependent thalassaemia patients. Eur J Orthod. 2011;33(6):700-4.
- Soriano AC, Gil Montoya JA, Lopez-Gonzalez Garrido Jde D. Thalassemias and their dental implications. Med Oral. 2002;7(1):36-40.
- Cao A, Moi P, Galanello R. Recent advances in beta-thalassemias. Pediatr Rep. 2011;3(2):e17.