Research Article - Journal of Primary Care and General Practice (2022) Volume 5, Issue 3
Oral ulceration with clinical decision-making in primary care practice.
Bronagh McGuckin, Brian Swinson*
Department of Oral and Maxillofacial Surgery, Altnagelvin Area Hospital, Western Health and Social Care Trust, Northern Ireland, United Kingdom
- *Corresponding Author:
- Brian Swinson
Department of Oral and Maxillofacial Surgery
Altnagelvin Area Hospital
Western Health and Social Care Trust
Northern Ireland
United Kingdom
E-mail: bronagh.mcguckin@nhs.net
Received: 22-Jan-2022, Manuscript No. AAPCGP-22-52163; Editor assigned: 25-Jan-2022, PreQC No. AAPCGP-22-52163(PQ); Reviewed: 09-Feb-2022, QC No. AAPCGP-22-52163; Revised: 26-Apr-2022, Manuscript No. AAPCGP-22-52163(R); Published: 05-May-2022, DOI: 10.35841/aapcgp-5.3.111
Citation: Swinson B. Oral ulceration with clinical decision-making in primary care practice. J Prim Care Gen Pract. 2022;5(3):111
Abstract
Oral ulceration is a common disorder of the oral mucosa with individuals regularly presenting to primary care practitioners seeking advice and treatment. Diagnosis of oral ulceration remains a challenge for clinicians due to the overlap in clinical presentations and the diverse aetiological processes that can be involved in their development. A recent study evaluating general medical practitioners’ attitudes towards oral examination identified problems in clinicians’ confidence in differentiating between benign and malignant ulcers, with a lack of knowledge and training being cited as contributing factors. This article aims to provide an overview of the diagnosis and management of oral ulceration, providing a framework to guide clinical decision-making in a primary care setting.
Keywords
Oral ulceration, Oral mucosa, Medical practitioners, Aetiological processes.
Introduction
An ulcer is defined as a “break in the skin or mucous membrane which fails to heal leading to a loss of surface tissue, disintegration and epithelial necrosis” [1]. Oral ulcers are common, with individuals presenting to primary care practitioners complaining of pain, discomfort and functional compromise. Due to the variety of presenting clinical features and causative factors, diagnosis of oral ulcerative lesions may be relatively challenging. Fortunately, the majority of oral ulcers are benign and can be managed using a variety of medications.
A small proportion of ulcers are malignant, with 6,500 cases of oral cancers diagnosed in the UK every year [2]. Over 95% of oral cancers are oral squamous cell carcinomas (SCC) and the major risk factors for these are smoking and alcohol consumption [3]. The main treatment for oral cavity SCC is surgery with complementary radiotherapy, chemotherapy or both to reduce the possibility of recurrence. The National Institute for Health and Care Excellence (NICE) has developed national referral guidelines to accelerate the process from initial referral by a generalist to be seen by a specialist within two weeks of referral [4]. It has been shown that timely diagnosis of oral SCC reduces mortality. A survey recently showed that 66-69% of patients with an oral ulcer would first approach their general medical practitioner (GMP) for advice; therefore it is imperative that GMPs are confident in the diagnosis and management of such ulcers [5].
Aetiology
Causes of oral ulceration can range from localised trauma to oral cancer or a manifestation of systemic disease. A surgical sieve approach to differential diagnosis, shown in Table 1, provides a useful framework to consider various types of pathologies systematically [6].
|
Clinical features |
Examples |
|---|---|
|
Reactive
|
Traumatic ulcers |
|
Infectious diseases
|
Herpetic infection (primary or secondary) |
|
Local immune-dysregulation
|
Recurrent aphthous stomatitis |
|
Immune-mediated conditions
|
Lichen planus |
|
Neoplastic
|
Squamous cell carcinoma |
Table 1. Surgical sieve approach to oral ulceration (Ferneini and Goupil, 2019)
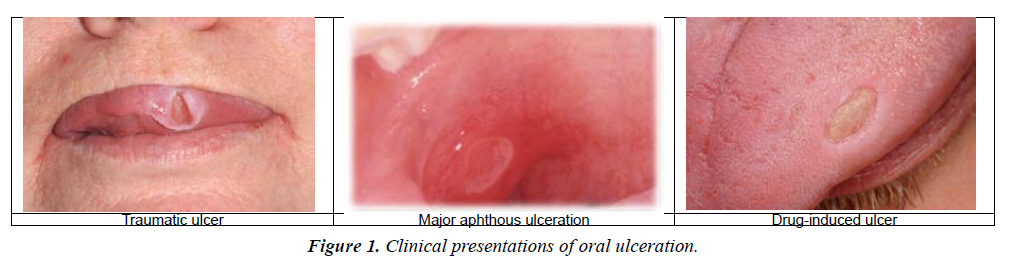
Traumatic ulcers
Traumatic ulcers are the most common oral ulcer and usually present as single, painful, irregular ulcer. Classically, patients recall an incident that preceded the development of the ulcer such as cheek/tongue bite or may be aware of a sharp tooth or restoration. Clinically, they present as a single shallow yellowwhite ulcer with irregular, erythematous borders which heal within three weeks of the initial injury. Traumatic ulcers will persist or recur if the stimulus is not resolved.
Recurrent Aphthous Stomatitis (RAS)
Recurrent aphthous stomatitis (RAS) is an acute ulcerative disease of local immune dysregulation and is the second most common oral ulcerative condition with a global prevalence of 25% [7]. RAS frequently commences in young adulthood and predisposing factors that have been identified include: genetic factors, local factors such as trauma or exposure to particular foods, haematinic deficiency, and systemic conditions such as Crohn’s disease.
Clinically, patients with RAS present with painful ulcers affecting the non-keratinised mucosal surfaces (e.g. buccal mucosa, floor of the mouth, ventral tongue and soft palate), which are round-toovoid with a yellow-white fibrin necrotic centre and erythematous borders. Given the acute nature of RAS, ulcers can present suddenly and typically last for 7-10 days, with some patients reporting specific inciting triggers. RAS is classified depending on the size of ulcers: minor (less than 1cm diameter) which usually heals spontaneously within two weeks, major (more than 1cm diameter) which may take longer than three weeks to resolve and herpetic form (1-2mm diameter) which present as a cluster of ulcers. RAS is self-limiting, but in severe cases topical or systemic corticosteroids are recommended. Specialist referral for further investigation is indicated when episodes of lesions become more severe, late-onset RAS, or when lesions are accompanied by systemic symptoms.
Drugs
Oral ulceration can be the result of the use of drugs themselves. Oral mucosal burns are seen when drugs are inappropriately applied topically to the gingivae e.g. aspirin near a toothache or use of illicit drugs such as cocaine. Lichenoid reaction, similar in appearance to lichen planus, is associated with a number of drugs such as ACE inhibitors and NSAID. Some drugs may cause oral ulceration directly e.g. nicorandil, which will persist until the drug reduced or withdrawn. Anti-resorptive drugs such as bisphosphonates and denosumab have been linked to medication-related osteonecrosis of the jaws, often presenting as a non-healing ulceration of the overlying oral mucosa with exposed necrotic bone which is very challenging to manage and requires specialist referral (Figure 1).
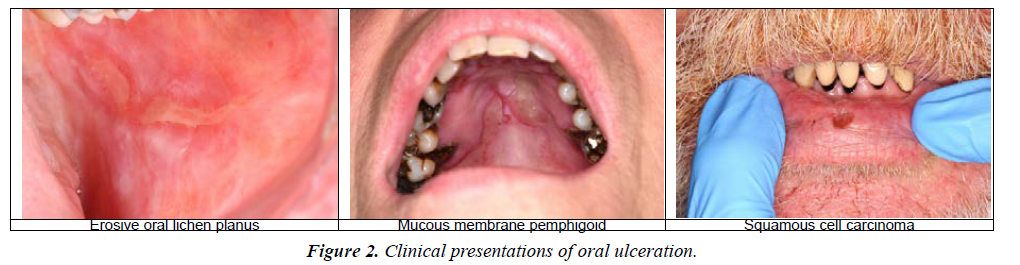
Squamous cell carcinoma
Squamous cell carcinoma (SCC) represents about 95% of all oral malignancies and accounts for 1-2% of all cancers worldwide. Approximately 80% of patients are aged 40+ years and it is twice more common in men than women, with tobacco smoking and alcohol as risk factors [8]. Clinical presentation can range from red, white or red-white patches to an ulcerative lesion. Commonly, they present as asymptomatic, slow-growing, non-healing ulcers with raised rolled borders and high risk sites include the ventral or lateral surface of the tongue, the floor of mouth or the soft palate. On presentation, 30% of patients will have involvement of the submandibular and cervical lymph nodes [9]. Given the destructive nature of SCCs, a timely and accurate diagnosis is key to improving the patients’ prognosis. Management usually involves a combination of therapeutic modalities including surgery, radiotherapy and occasionally chemotherapy.
Lichen planus
Lichen planus is a chronic T-lymphocyte mediated inflammatory disease of skin and mucous membranes with characteristic oral lesions. It generally affects females more than males and middle-aged patients. There are various clinical presentations including erosive/ulcerative, reticular, bullous and popular lesions with the frequently affected sites being the buccal mucosa, palate, gingivae and tongue. It is considered a pre-malignant lesion therefore correct diagnosis and longterm follow-up with a specialist is important. The mainstay of treatment remains topical and systemic corticosteroids.
Mucous membrane pemphigoid
Mucous Membrane Pemphigoid (MMP) is a chronic, immunobullous condition mainly affecting the oral mucosa. It is predominantly a disease of the older population and is twice as common in women as men. The most commonly affected site in the oral cavity is the gingivae, with a characteristic desquamative gingivitis presentation, followed by the buccal mucosa and palate. Lesions may also affect the eyes, skin, nose and genitalia. Patients suspected of having MMP should be referred for specialist care and symptoms can be managed with topical or systematic corticosteroids (Figure 2).
Pemphigus vulgaris
Pemphigus vulgaris is a rare, potentially life-threatening chronic autoimmune condition which is characterised by epithelial blistering of mucocutaneous surfaces. Oral lesions begin as fragile bullae which rupture, resulting in large, irregular, painful ulcers/erosions. The lesions are most frequently observed in the buccal mucosa, palate and gingivae. Skin lesions may appear several months later. Timely specialist referral is key to promote healing of lesions, prevent infection, and decrease frequency of new lesions and control symptoms. High dose systemic corticosteroids such as prednisolone combined with an adjuvant immunosuppressant such as azathioprine remain the gold standard treatment.
Infection
Primary herpetic gingivostomatitis is the most common manifestation of the primary herpes simplex virus and is typically seen in children and young adults. Oral features consist of multiple vesicles affecting the oral mucosa which rupture forming painful ulcers with a red, elevated halomargin and a depressed yellow-white pseudomembrane. The ulcers usually heal spontaneously within one week however may persist in more severe cases.
Herpes zoster infection due to reactivation of varicella-zoster virus can also result in oral ulceration. Clinically, clustered ulcers (less than 5mm in diameter) appear on the buccal gingivae or hard palate in a characteristic unilateral pattern, and tend to heal within two weeks. Management for viral infections is directed toward pain control and hydration, with the use of antivirals only effective when started within 72 hours of disease onset.
Erythema multiforme
Erythema multiforme is an uncommon mucocutaneous hypersensitivity reaction triggered by a range of exogenous factors e.g. medications, infections such as herpes simplex virus and mycoplasma infection, and food additives or chemicals. It typically affects young males and is characterised by ‘target lesions’ on the skin and macules on the lips and buccal mucosa which evolve to bullae and ulcers with irregular borders with an inflammatory halo. Prodromal signs such as fever, lymphadenopathy, and malaise may be noticed prior to onset of mucocutaneous erythema or blisters. In the mild forms, healing takes place within three weeks; therefore, patients only need local wound care, liquid diet, and topical analgesics for pain control, however, in more severe cases, patients should be referred for treatment with systemic corticosteroids or other immunomodulatory drugs.
Diagnosis
History
A structured approach to history-taking is vital to establish the pattern and frequency of ulceration, which in turn, allows a differential and ultimately a definitive diagnosis to be determined. A useful mnemonic to guide history-taking is the SOCRATES approach, outlined in Table 1. This should be followed by a systematic medical history, noting any dermatological, ophthalmological, haematological, gastrointestinal, and rheumatological manifestations. Common drugs which have been associated with oral ulceration include NSAIDs, nicorandil and anti-hypertensives. Drug-related ulceration will resolve with either dose reduction or complete cessation of the medication. Risk factors for oral cancer should be identified and evaluated such as alcohol consumption and tobacco use. Additionally, a brief dental history can ascertain if any recent treatment has been carried out or any appliance is being worn and causing irritation (Table 2).
| Site | Location of ulcer(s) |
|---|---|
| Onset | Duration of current episode Date of first episode |
| Characteristics | Pain Painless |
| Radiation | Lesions or ulcers elsewhere in the body |
| Associated symptoms | Systemic upset at time of ulceration |
| Timing | Period of time between episodes |
| Exacerbating and relieving factors | Particular foods e.g. spicy foods Analgesics required |
| Severity | Able to eat/drink Night-waking |
Table 2. Ulceration history
Examination
The examination should begin with an extra-oral examination, visually inspecting and palpating the head and neck region to detect any swelling or lymphadenopathy. This should be followed by an intra-oral examination, which requires an adequate light source and ideally a dental mirror or tongue depressor to allow full inspection of the oral mucosa.
• Single ulcer
• Painless
• Present for more than 3 weeks
• Granular floor
• Rolled thickened edge
• Lack of inflammation surrounding ulcer.
• Sites including floor of mouth, lateral and ventral surfaces of tongue, soft palate.
Management
Symptomatic relief
Due to the often painful nature of ulceration, patients may require symptomatic relief prior to the establishment of a definitive diagnosis. A variety of pharmacological modalities can be utilised, these include: warm saline mouth rinses, topical analgesic and anti-inflammatories (e.g. benzydamine hydrochloride), antimicrobial agents (e.g. chlorhexidine gluconate), physical barrier applications (e.g. carmellose gelatine), topical anaesthetics (e.g. lidocaine hydrochloride), systemic analgesics and topical and systemic corticosteroids (e.g. betamethasone, prednisolone) [10].
Topical Preparations
Topical anaesthetic
Lidocaine hydrochloride 5% ointment or 10% spray apply as required, rub sparingly and gently on affected areas.
Topical analgesics/anti-inflammatory agent
Benzydamine hydrochloride 0.15% mouthwash or mucosal spray, rinse 15ml or spray 4-8 times every 1.5-3 hours as required.
Topical antimicrobial agents
Chlorhexidine gluconate 0.2% mouthwash or spray, rinse 10ml four times daily or apply up to 12 sprays twice daily to ulcer surface.
Topical corticosteroids
Betamethasone 500 micrograms soluble tablets dissolved in 20ml water and rinsed around the mouth, not to be swallowed, up to four times daily.
Special investigations
Haematological investigations are useful and can exclude any underlying causes of ulceration such as iron, vitamin B12 or folic acid deficiency or deficiencies? If cancer is suspected, a tissue biopsy must be performed by an Oral Medicine/ Maxillofacial specialist [11-14].
Referral
When there is a high suspicion that an ulcer is of traumatic origin due to a dental prostheses or restoration, the patient should be advised to contact their general dental practitioner.
If an ulcer persists for more than three weeks, in the absence of obvious traumatic aetiology, a red flag referral should be made to the local Oral Medicine or Maxillofacial Surgery Department. Additionally, recurrent ulceration, or ulcers with a systemic background or requiring further investigations may also benefits from specialist referral.
Key Points
• Oral ulceration is common and mostly benign.
• A detailed history and thorough examination will aid diagnosis and management.
• Suspicious oral lesions can present in a wide variety of forms and patients with an ulcer persisting for more than three weeks should be referred urgently to an Oral Medicine or Maxillofacial specialist.
• Alcohol and tobacco smoking are key risk factors for the development of oral cancer.
• Referral to secondary care for specialist opinion is appropriate in cases where the potent topical corticosteroids and systemic therapy is likely to be required.
• Clinical photographs (taken with patient consent) attached to the referral will benefit accepting clinicians.
Conclusion
A systematic approach to this examination, beginning with the lips, followed by the cheek mucosa, floor of mouth, tongue, teeth and gums and palate, will avoid a lesion being missed. The ulcer(s) should be inspected with respect to: site, size, shape, margin, base and consistency. The presence of any prosthesis, sharp teeth or dental restoration, in relation to an ulcer should be recorded. Clinical features of an ulcer which should raise suspicion are outlined in clinical features of malignant oral ulcer.
Acknowledgement
Clinical photographs all original with consent for publication and are copyright of Belfast Health and Social Care Trust.
References
- Edsberg LE, Black JM, Goldberg M. Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585.
- National Institute of Health and Care Excellence. Head and neck cancers – recognition and referral. 2020.
- Cancer Research UK. Mouth and Oropharyngeal Cancer 2018.
- National Institute of Health and Care Excellence. Suspected cancer: Recognition and Referral. 2015.
- Gill Y, Scully C. Mouth ulcers: A study of where members of the general public might seek advice. Br Dent J. 2007;202(6):E16.
- Ferneini EM, Goupil MT. Evidence-based Oral Surgery: A Clinical Guide for the General Dental Practitioner. Springer International Publishing; 2019.
- Barrons RW. Treatment strategies for recurrent oral aphthous ulcers. Am J Health Syst Pharm. 2001;58(1):41-50.
- Joint Formulary Committee. British national formulary 81. London: BMJ Publishing and the Royal Pharmaceutical Society. 2021.
- Thermos G, Kalogirou EM, Tosios KI. Oral ulceration with bone sequestration: Retrospective study of eight cases and literature review. Oral Dis. 2019;25(2):515-22.
- Farah CS, Savage NW. Oral ulceration with bone sequestration. Australian dental J, 2020;48(1), 61-64.
- Lee J, Shin D, Roh JL. Treatment of intractable oral ulceration with an oral mucosa equivalent. J Biomed Mater Res B Appl Biomater. 2019;107(6):1779-85.
- Palla B, Burian E, Klecker JR. Systematic review of oral ulceration with bone sequestration. J Craniomaxillofac Surg. 2016;44(3):257-64.
- Lidhar T, Ethunandan A, Ethunandan M. Spontaneous oral ulceration with bone sequestration: its relevance in current clinical practice. Br J Oral Maxillofac Surg. 2020;58(9):e75-9.
- Peters E, Lovas GL, Wysocki GP. Lingual mandibular sequestration and ulceration. Oral Sur Oral Med Oral Path. 1993;75(6):739-43.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref