Research Article - Biomedical Research (2017) Volume 28, Issue 2
Oral ketamine administration for radiation therapy in children
Erdal Doğan1, Abdulmenap Güzel1*, Seyit Burhanedtin Zincircioğlu2, Mehmet Şerif Arslan3, Feyzi Çelik1, Mehmet Beşir Yildirim4, Zeynep Baysal Yildirim1 and Mahir Kuyumcu11Department of Anesthesiology, School of Medicine, Dicle University, Diyarbakır, 21280, Turkey
2Department of Radiation Oncology, School of Medicine, Dicle University, Diyarbakır, 21280, Turkey
3Department of Pediatric Surgery, School of Medicine, Dicle University, Diyarbakır, 21280, Turkey
4Department of Anesthesiology, The Pediatrics Hospital of Diyarbakır, Turkey
- *Corresponding Author:
- Abdulmenap Güzel
Department of Anesthesiology and Reanimation, Faculty of Medicine
Dicle University, Diyarbakır, Turkey
Accepted date: June 20, 2016
Abstract
Background: Radiotherapy is a reliable and effective treatment for various malignancies and can be used for both curative and palliative/prophylactic ends. In order to achieve accuracy, reliability and success in the implementation of radiotherapy, it is imperative that patients adapt to the treatment and remain motionless.
Material and Methods: In this study, the records of anesthetic agents utilized in 26 patients aged 2-10 being treated by external beam radiotherapy were examined.
Results: Radiotherapy under anesthesia was implemented in a total of 56 sessions conducted on 26 patients. During the radiotherapy applications, only 10 (17%) sessions required the use of an extra dose of ketamine. The radiotherapy session duration was 6.3 ± 2.4 minutes. (The anesthesia start time was 20.5 ± 4.6.) Additionally, the patients' recovery time from anesthesia was found to be 68.6 ± 6.2. 61.5% of the patients were administered prophylactic cranial radiotherapy due to acute lymphoblastic leukaemia (ALL). Before and after the procedure, hemodynamic and respiratory parameters were found to be stable.
Conclusion: Since a combination of oral ketamine and midazolam provides effective sedation and comfort and can be administrated easily, we believe that it can be safely used in radiotherapy procedures on children.
Keywords
Anesthesia, Oral ketamine, Children, Radiotherapy.
Introduction
Radiotherapy is a reliable and effective treatment for various malignancies and can be used for both curative and palliative/ prophylactic ends [1]. In order to achieve accuracy, reliability and success in the implementation of radiotherapy, it is imperative that patients adapt to the treatment and remain motionless [2].
Using an appropriate approach with older children and in collaboration with their parents, radiotherapy applications can be administered without resorting to anesthesia. However, during radiotherapy applications, the need for anesthesia shows an inverse proportional increase, and the implementation of anesthesia or sedation is required, especially during the treatment of children aged 0–5 [3].
In cases of radiotherapy involving children, aside from physical issues such as positioning limitations required by the procedure and difficulties in reaching the patient, health issues stemming from the patient's primary diagnosis also require special care and preparation. In addition, in certain cases that require repeated radiotherapy, frequent anesthetic procedures may be necessary [4].
In this study, we aimed to determine the efficacy of oral ketamine used during radiotherapy procedures of the cases of 26 children aged 2-10.
Material and Methods
In this study, with the permission of the Ethics Board between September 2007 and September 2010 at Dicle University Faculty of Medicine Radiation Oncology Department Treatment Unit, the records of 26 patients aged 2-10 being treated by external beam radiotherapy were examined. Aside from the patients' demographic data such as age and sex, their primary diagnoses, the doses of anaesthetic agents utilized, procedure times and any complications were recorded.
Before each anaesthesia procedure, the presence of an oxygen source, aspirator, AmbuR (ballon-mask airway) system, laryngeal mask, laryngoscope, intubation tube, airway and intravenous (IV) line equipment, as well as emergency medicine within the procedure room was checked and verified. For all patients, 5 mg/kg ketamine and 0.5 mg/kg midazolam were prepared in a mixture of sour cherry juice. Atropine was used to prevent adverse effects (such as prevention salivation) with a dose of 0.01 mg/kg. Following 4-6 hours of fasting, the patients were fed the concoction by their parents at 0.5 ml/kg. Once their Ramsay sedation score [5] reached 3 or above, the patients were taken to the radiotherapy unit, IV lines were started, and EKG, SpO2 and non-invasive arterial pressure monitoring were provided. Throughout the procedure, O2 at a rate of 3 L/min was delivered to the patients via nasal cannula.
Once sufficient sedation was achieved, patients at their first RT session underwent measurements for RT and simulation processes to determine the exact locations. When patient motionlessness was achieved, and if the vital parameters (SpO2, BP, BFR values) were within normal limits, the patient was left in the RT room and the RT process started through observation from outside via a camera system. If the procedure time exceeded five minutes or any movement in the extremities was observed, an extra dose of 0.5 mg/kg IV ketamine was delivered.
Afterward, the patients were taken to the recovery room. Patients whose spontaneous respiration was regular and sufficient, whose airway protective reflexes were existent, and whose vital parameters evaluated within normal clinical limits were observed for at least 45 minutes and then discharged.
The sedation levels of the patients from the beginning to the end of the procedure were evaluated every ten minutes using the Ramsay sedation scale (1: Tense, nervous; 2: Calm, relaxed; 3: Responds to aural stimuli; 4: Responds to physical stimuli; 5: Responds to painful stimuli; 6: Does not respond to painful stimuli) until they have gone to their clinics have been evaluated. Patients with sedation score of 3 or higher were administered radiotherapy.
The statistical analyses of the study data were performed by SPSS 16.0 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics of the demographic data and continuous variables were given as mean ± standard deviation and percentages.
Results
The demographic data from the patients evaluated in the study are shown in Table 1. Radiotherapy under anesthesia was implemented in a total of 56 sessions conducted on 26 patients. During the radiotherapy applications only 10 (17%) sessions required the use of an extra dose of ketamine. The radiotherapy session duration was 6.3 ± 2.4 minutes. (The anesthesia start time was 20.5 ± 4.6.) Additionally, the patients' recovery time from anesthesia was found to be 68.6 ± 6.2 minutes.
| Mean ± SD, n | |
|---|---|
| Age (years) | 4,85 ± 2.97 |
| Height (cm) | 102 ± 17.16 |
| Weight (kg) | 16.8 ± 5.87 |
| Gender (f/m) | 15/11 |
| ASA I/II | 18/8 |
| The radiotherapy session duration (min) | 6.3 ± 2.4 |
| The onset of anesthesia (min) | 20.5 ± 4.6 |
| Recovery time | 68.6 ± 6.2 |
| ASA: American Society of Anesthesiologists risk scores; Value was calculated as mean ± SD; f: female; m: male | |
Table 1. Demographic data of the patients.
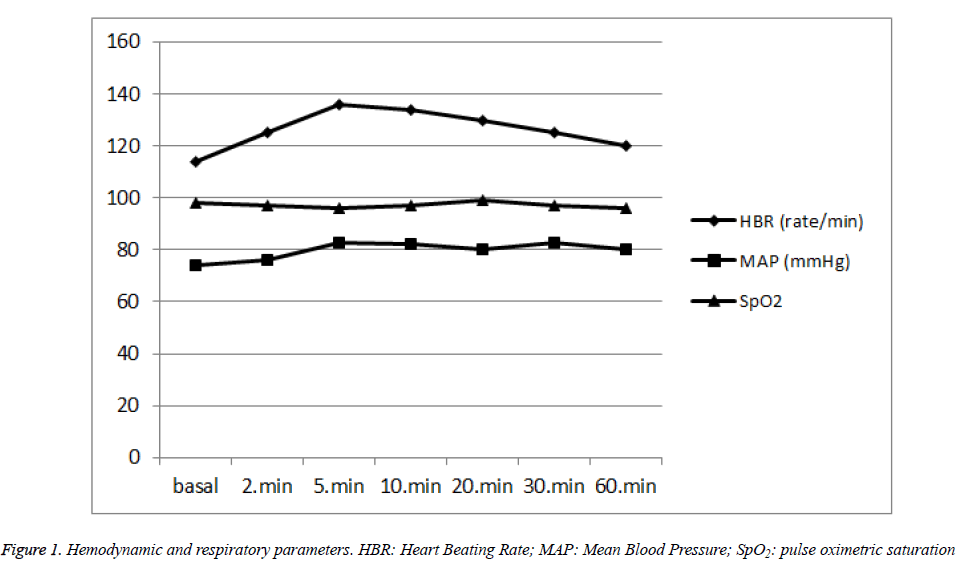
The clinical diagnoses of the patients are shown in Table 2. 61.5% of the patients were administered prophylactic cranial radiotherapy due to acute lymphoblastic leukemia (ALL). Before and after the procedure, the patients’ hemodynamic and respiratory parameters were found to be stable (Figure 1). No serious complications were observed in the patients during the procedure.
| Diagnoses | n (%) |
|---|---|
| Neurofibromatosis | 1 (3.8) |
| ALL* | 16 (61.5) |
| Neuroblastoma | 2 (7.6) |
| Medulloblastoma Glioblastoma Multiforme |
3 (11.5) 4 (15.4) |
| *ALL: Acute Lymphoblastic Leukemia; n: number, %: percent | |
Table 2. Clinical diagnoses of the patients.
Discussion
The success of modern radiotherapy procedures depends on teamwork. In cases of children whose general condition is poor due to illness, and whose long radiotherapy sessions require a motionless position difficult to maintain, anaesthesiology modalities are used in order to successfully implement radiotherapy [6]. It has been reported that during radiotherapy, some patients are not able to receive the required radiation due to insufficient immobilization [7].
What are expected from an ideal sedation method are reliability, amnesiac properties, and its ability to provide immobility and analgesia. It should not depress respiratory or cardiovascular reflexes while providing these effects. The effects of the administered drugs should start quickly and end shortly, should not lead to delays in recovery, and the dosage should be adjustable depending on the patient’s response [8]. Additionally, in children, the drugs should decrease anxiety and make separation from the child’s family easier [9,10].
Different methods have been tried to achieve this. Chloral hydrate, midazolam and ketamine have been used both orally and rectally [11]. Intravenous sedation (IV) is efficient and reliable in children's radiotherapy procedures. Especially in cases where peripheral or central IV cannulation is ready and available for use, sedation can be started quite quickly using the IV route [12]. However, IV injections are one of the most serious causes of anxiety in hospitalized children. Additionally, IV routes are one of the primary sources of infections that develop in these children due to the disruption of dermal barrier [13].
During radiotherapy, IV propofol is preferred due to its quick onset, short mechanism of action, and its prevention of nausea and vomiting. However, the significant respiratory depression induced by propofol limits its use in anesthesiology procedures outside of the operating room [7]. Midazolam is a short-acting anxiolytic agent without any analgesic properties. It is preferred in sedation procedures due to its short duration of action, ease of administration, and the ability of flumazenil to antagonize its effects. However, in sedative doses it can cause respiratory depression, and when administered intravenously, quickly and in high doses, it can lead to apnea [14,15]. In our study, considering the work environment and the risk of respiratory depression, we did not administer sedation through IV midazolam or propofol. It has been reported that the oral use of benzodiazepines and ketamine has a similar effect to their IV use [DT2] [16].
Ketamine is a quick-onset, short acting anaesthetic agent with analgesic properties. It does not lead to respiratory depression or hypotension in therapeutic doses [17]. Used alone, ketamine often causes involuntary movements in patients. For this reason it might have a negative effect on the successful treatment of radiotherapy procedures. Ketamine combined with midazolam both prevents involuntary movements and provides a more efficient level of sedation [18]. Additionally, with the use of midazolam, ketamine-related increases in intracranial pressure and cardiovascular side effects can be prevented [17]. In a study, only oral midazolam was used for sedative purposes in radiological imaging, it was reported that the sedation was insufficient for 50% of the patients [19]. However, in a study in which oral ketamine and midazolam were used in combination, sufficient sedation was achieved [11].
In an experimental model, ketamine inhibited monoamine transporters expressed in human embryonic kidney cells in a dose-dependent manner. This could explain the psychotomimetic and sympathomimetic effects of ketamine, but according to an in vitro study, high ketamine doses are needed [20]. In this study, we used low-dose ketamine. Side effects of ketamine such as psychotomimetic and sympathomimetic effects were not observed. Ketamine also mediates its effects via cholinergic, nicotinic and muscarinic receptors. The inhibitory effect on muscarinic receptors can explain the increase in bronchial secretions and mucus formation after ketamine use [21]. In our study, the prevention of secretion was provided with atropine and we did not encounter any problems.
In external anesthesia procedures, a monitor, oxygen source, anesthesia machine, aspirator, and emergency drugs should be at hand, and standard anesthesia monitoring should always be performed. During radiotherapy procedures, the biggest disadvantage for the anesthesiologist is the need to leave the patient’s side. During this period, the anesthesiologist watches the patient from the monitoring room via video cameras. Even though radiotherapy procedures are usually short, being physically separated from the patient is risky in terms of patient safety. Additionally, it is imperative for the patient to remain motionless throughout the procedure to ensure its safety and success. For this reason, the anesthesiologist should apply a level of sedation that will ensure motionlessness without risking patient safety.
In our clinic, we give a combination of oral ketamine and midazolam to all our radiotherapy patients. In 82.2% of our patients, the procedure is successfully completed without any need for additional dosage. We have not encountered any complications such as nausea-vomiting or respiratory depression in any of our patients.
Conclusions
Since oral ketamine and midazolam in combination provide effective sedation and comfort and can also be administrated easily, we believe that they can be safely used in radiotherapy procedures on children.
References
- Sejpal SV, Bhate A, William Small W. Palliative Radiation Therapy in the Management of Brain Metastases, Spinal Cord Compression, and Bone Metastases. Semin Intervent Radiol 2007; 24: 363-374.
- Carri K, Glide-Hurst, Chetty IJ. Improving radiotherapy planning, delivery accuracy, and normal tissue sparing using cutting edge technologies. J Thorac Dis 2014; 6: 303-318.
- Twite MD, Friesen RH. Pediatric sedation outside the operating room: The year in review. Curr Opin Anaesthesiol 2005; 18: 442-446.
- Fernández BM, Gualda CL, Fernández JMI, Castilla MM. Radiotherapy treatment under anesthesia in pediatrics. Rev Esp Anestesiol Reanim 2002; 49: 324-327.
- Michael A, Ramsay E, Newman KB, Jacobson RM, Richardson CT, Rogers L, Brown BJ, Hein HAT, Vol EBD, Yahya A. Daoud Sedation levels during propofol administration for outpatient colonoscopies. Proc (Bayl Univ Med Cent) 2014; 27: 12-15.
- Tsang RW, Solow HL, Ananthanarayan C, Haley S. Daily general anesthesia for radiotherapy in unco-operative patients: Ingredients for successful management. Clin Oncol 2001; 13: 416-421.
- Wojcieszek E, Rembielak A, Bialas B, Wojcieszek A. Anesthesia for radiation therapy-Gliwice experience. Neoplasma 2010; 57: 155-160.
- Ghai B, Grandhe RP, Kumar A, Chari P. Comparative evaluation of midazolam and ketamine with midazolam alone as oral premedication. Paediatr Anaesth 2005; 15: 554-559.
- Berry FA. Midazolam as premedication: is the emperor naked or just half-dressed Paediatr Anaesth 2007; 17: 400-401.
- Roelofse JA, Shipton EA, Harpe CJ, Blignaut RJ. Intranasal sufentanil/midazolam versus ketamine/midazolam for analgesia/sedation in the pediatric population prior to undergoing multiple dental extractions under general anesthesia: a prospective, double-blind, randomized comparison. Anesthesia Progress 2004; 5: 114-121.
- Cengiz M, Baysal Z, Ganidagli S. Oral sedation with midazolam and diphenhydramine compared with midazolam alone in children undergoing magnetic resonance imaging. Paediatr Anaesth 2006; 16: 621-626.
- Seiler G, De Vol E, Khafaga Y, Gregory B, Al-Shabanah M, Valmores A, Versteeg D, Ellis B, Mustafa MM, Gray A. Evaluation of the safety and efficacy of repeated sedations for the radiotherapy of young children with cancer: a prospective study of 1033 consecutive sedations. Int J Radiat Oncol Biol Phys, 2001; 49: 771-783.
- Burke A. Intravenous l?ne infections. Critical care clinics 1998; 14: 339-346.
- Ghai B, Grandhe RP, Kumar A, Chari P. Comparative evaluation of midazolam and ketamine with midazolam alone as oral premedication. Pediatr Anesth 2005; 15: 554-559.
- Cengiz M, Baysal Z, Ganidagli S. Oral sedation with midazolam and diphenhydramine compared with midazolam alone in children undergoing magnetic resonance imaging. Paediatr Anaesth 2006; 16: 621-626.
- Topal A, Erol A, Tavlan A, K?l?çaslan A, Yalç?n N. Comparison of Intranasal Midazolam and Midazolam-Sufentanil for Premedication in Children. Turkish Journal of the Anaesthesiology and Reanimation 2008; 36: 277-282.
- Bar-Joseph G, Guilburd Y, Tamir A, Guilburd JN. Effectiveness of ketamine in decreasing intracranial pressure in children with intracranial hypertension. J Neurosurg Pediatr 2009; 4: 40-46.
- Shewale S, Saxena A, Trikha A, Singh M, Sharief A. Oral ketamine for radiotherapy in children with cancer. Indian J Pediatr 2000; 67: 263-266.
- D’agostino J, Terndrup TE. Chloral hydrate versus midazolam for sedation of children for neuroimaging: a randomized clinical trial. Pediatr Emerg Care 2000; 16: 1-4.
- Peltoniemi MA, Hagelberg NM, Olkkola KT, Saari TI. Ketamine: A Review of Clinical Pharmacokinetics and Pharmacodynamics in Anesthesia and Pain Therapy. Clin Pharmacokinet 2016.
- Sinner B, Graf BM. Ketamine. Handb Exp Pharmacol. 2008; 182: 313-333.