Research Article - Biomedical Research (2017) Volume 28, Issue 14
Operative versus non-operative treatment of posterior malleolus fragment in trimalleolar fracture: A retrospective cohort study
Mehmet Selçuk Saygılı1*, Barış Özkul1, Engin Çetinkaya1, Ali Cagri Tekin2, Avni Ilhan Bayhan1, Ismail Kalkar3, Deniz Akbulut1 and Bilal Demir1
1M.S. Baltalimani Bone Diseases Training and Research Hospital, Istanbul, Turkey
2Okmeydani Training and Research Hospital, Istanbul, Turkey
3Taskopru State Hospital, Turkey
- *Corresponding Author:
- Mehmet Selçuk Saygılı
M.S. Baltalimani Bone Diseases Training and Research Hospital
Istanbul, Turkey
Accepted on June 27, 2017
Abstract
Introduction: The treatment of Posterior Malleolus (PM) fracture in trimalleolar surgery is still controversial. Fixation of PM is determined according to joint congruency and posterior fragment size. When the ratio of posterior fragment is less than 25% of anteroposterior dimension of the articular surface, conservative treatment is suggested in the literature. The aim of this study was to evaluate the functional and radiological outcomes of the patients with trimalleolar fracture that had either PM fixation or not when the PM ratio is less than 25%.
Materials and Methods: Archives of 73 patients that had trimalleolar surgery in our hospital between 2010 and 2014 were evaluated retrospectively. Inclusion criteria’s were as follow: being over 18 y old, PM fractures measuring less than 25% of the joint surface in the lateral ankle x-ray, having preoperative ankle Computer Tomography (CT) , both medial and lateral malleolar fixation, with at least 2 y of follow-up. Exclusion criteria’s were as follow: pathologic fractures, metabolic disorders, ipsilateral fracture, fracture history in the same ankle, incongruous talocrural angle, medial and superior talo tibial incongruity in the postoperative early x-rays. Haraguchi classification, PM size and ratio, use of transsyndesmotic screw, American Orthopaedic Foot and Ankle Society (AOFAS) anklehind foot scores were evaluated. Kolmogorov-Smirnov was used to evaluate the distribution of the variables and Mann-Whitney U-test was used for statistical analysis.
Results: Among the patients who had PM fixation and without fixation, there was no statistically significant difference in their AOFAS score.
Conclusions: There was no significant functional difference found in trimalleolar fracture when PM fraction ratio is smaller than 25% in comparison of PM fixation, however, the decreased need of transsyndesmosis fixation needs to be taken into consideration.
Keywords
Ankle, Posterior malleol, Trimalleoler fracture, Haraguchi classification.
Introduction
The ankle fracture rate is 107 fractures per 105 person/y [1]. Trimalleolar fracture consists 7% of all ankle fractures [2]. The treatment of Posterior Malleolus (PM) fracture in trimalleolar surgery is still controversial [3-6]. Fixation of PM should be considered, when articular surface of PM fragment is larger than 25% and need for greater syndesmotic stability [7]. However, the joint congruency is shown to be important than fixation or size of the PM fragment for long term radiological outcome [8]. In their review Odak et al. reported that PM doesn’t have a major role in weight bearing and ankle stability [9]. Our hypothesis was that fixation of PM fragment regardless of fragment size has good functional outcomes compared to unfixed. The aim of this study was to evaluate the functional and radiological outcomes of the patients with trimalleolar fracture that had either PM fixation or not.
Patients and Methods
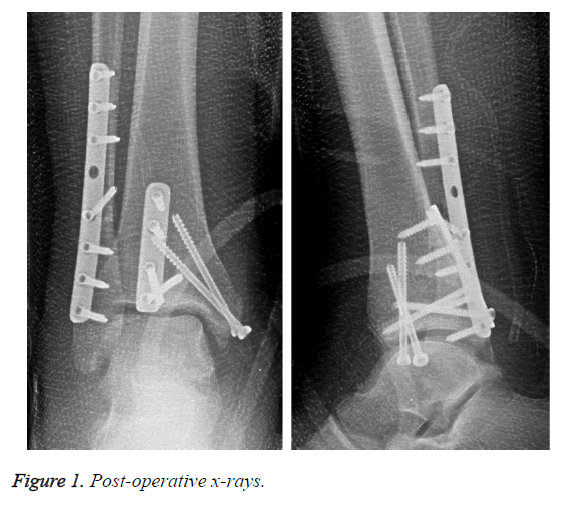
After IRB approval (Baltalimani Bone Diseases Training and Research Hospital IRB No: 19.04.2016-49), archives of the patients that had trimalleolar surgery in our hospital between 2010 and 2014 were evaluated retrospectively. Inclusion criteria’s were as follow: being over 18 y old, PM fractures measuring less than 25% of the joint surface in the lateral ankle x-ray, having preoperative ankle computer tomography (CT), both medial and lateral malleolar fixation, with at least 2 y of follow-up. Exclusion criteria’s were as follow: pathologic fractures, metabolic disorders, ipsilateral fracture, fracture history in the same ankle, incongruous talocrural angle, medial and superior talo tibial incongruity in the postoperative early x-rays (Figure 1) [10].
151 patients were found and 78 were excluded for not meeting the inclusion criteria. Patients were divided into two groups as PM fixation (27) and not (46). In the PM fixation group 12 (44.44%) were male and 15 (55.55%) female. Mean age was 45.29 ± 15.47 (18-75). In the other group 22 (47.82%) were male, 24 (52.17%) female. Mean age was 41.11 ± 12.64 (18-73). Fractures were classified according to AO/OTA and Haraguchi (Table 1 and Table 2). According to Haraguchi classification, there were 48% (13) type 1, 44% (12) type 2 and 8% (2) type 3 in the PM fixation group and 56% (13) type 1, 35% (12) type 2 and 9% (2) type 3 in the other group.
| No | Age/Sex | Side | AO classification | Haraguchi classification | PM fixation technique | Transsyndesmotic screw | AOFAS |
|---|---|---|---|---|---|---|---|
| 1 | 18/F | R | 44B3 | 1 | Posterior Plate | No | 100 |
| 2 | 23/M | L | 44B3 | 2 | Posterior Plate | No | 100 |
| 3 | 33/F | L | 44B3 | 1 | Posterior Plate | No | 90 |
| 4 | 45/F | R | 44B3 | 2 | Posterior Plate | No | 87 |
| 5 | 46/M | L | 44B3 | 2 | Posterior Plate | No | 87 |
| 6 | 46/F | R | 44C1 | 1 | Posterior Plate | No | 85 |
| 7 | 55/F | R | 44C1 | 1 | Posterior Plate | Yes | 90 |
| 8 | 60/M | L | 44C2 | 1 | Posterior Plate | No | 87 |
| 9 | 60/M | L | 44B3 | 2 | Posterior Plate | No | 87 |
| 10 | 63/F | R | 44C2 | 1 | Posterior Plate | Yes | 84 |
| 11 | 75/F | L | 44B3 | 2 | Posterior Plate | Yes | 84 |
| 12 | 33/M | L | 44B3 | 1 | Posterior Plate | No | 100 |
| 13 | 42/M | L | 44B3 | 3 | AP Screw | Yes | 80 |
| 14 | 52/M | R | 44B3 | 1 | AP Screw | No | 90 |
| 15 | 26/M | L | 44B3 | 3 | Posterior Plate | No | 90 |
| 16 | 22/F | L | 44B3 | 1 | AP Screw | No | 90 |
| 17 | 37/M | R | 44B3 | 1 | AP Screw | No | 84 |
| 18 | 35/F | R | 44C1 | 2 | Posterior Plate | No | 84 |
| 19 | 56/F | R | 44C2 | 2 | AP Screw | Yes | 80 |
| 20 | 62/M | L | 44C2 | 2 | AP Screw | No | 84 |
| 21 | 67/F | R | 44B3 | 2 | AP Screw | No | 80 |
| 22 | 51/F | R | 44B3 | 2 | Posterior Plate | No | 90 |
| 23 | 23/M | L | 44B3 | 1 | Posterior Plate | No | 90 |
| 24 | 40/F | L | 44C1 | 2 | Posterior Plate | No | 90 |
| 25 | 57/M | R | 44C2 | 2 | AP Screw | No | 84 |
| 26 | 45/F | L | 44B3 | 1 | AP Screw | Yes | 84 |
| 27 | 54/F | L | 44C1 | 1 | AP Screw | No | 80 |
Table 1. Summary of the PM fixation group data and results.
| No | Age/Sex | Side | AO classification | Haraguchi classification | Transsyndesmotic screw | AOFAS |
|---|---|---|---|---|---|---|
| 1 | 63/M | L | 44B3 | 1 | No | 100 |
| 2 | 46/F | L | 44C2 | 2 | Yes | 100 |
| 3 | 48/F | L | 44C1 | 1 | Yes | 90 |
| 4 | 30/F | R | 44B3 | 2 | Yes | 87 |
| 5 | 57/M | L | 44B3 | 2 | No | 87 |
| 6 | 41/M | R | 44C2 | 1 | Yes | 85 |
| 7 | 29/M | L | 44B3 | 1 | Yes | 90 |
| 8 | 58/F | R | 44B3 | 1 | Yes | 87 |
| 9 | 63/F | R | 44B3 | 2 | Yes | 87 |
| 10 | 26/F | R | 44B3 | 1 | No | 84 |
| 11 | 33/F | L | 44B3 | 2 | Yes | 84 |
| 12 | 51/M | R | 44C1 | 1 | Yes | 100 |
| 13 | 46/M | L | 44B3 | 3 | Yes | 80 |
| 14 | 60/F | R | 44C1 | 1 | No | 90 |
| 15 | 36/M | R | 44B3 | 3 | Yes | 90 |
| 16 | 42/F | R | 44B3 | 1 | Yes | 90 |
| 17 | 43/F | L | 44B3 | 1 | No | 84 |
| 18 | 38/M | R | 44B3 | 2 | Yes | 84 |
| 19 | 26/M | R | 44B3 | 2 | Yes | 80 |
| 20 | 18/M | L | 44C1 | 2 | Yes | 84 |
| 21 | 20/M | L | 44B3 | 1 | Yes | 84 |
| 22 | 35/M | R | 44B3 | 1 | Yes | 85 |
| 23 | 42/F | L | 44C1 | 3 | No | 98 |
| 24 | 49/F | L | 44B3 | 2 | Yes | 87 |
| 25 | 41/M | R | 44C1 | 2 | No | 97 |
| 26 | 36/F | L | 44B3 | 1 | Yes | 87 |
| 27 | 42/F | R | 44B3 | 1 | Yes | 80 |
| 28 | 33/M | R | 44B3 | 2 | Yes | 84 |
| 29 | 27/F | L | 44B3 | 2 | Yes | 87 |
| 30 | 56//F | R | 44B3 | 2 | No | 90 |
| 31 | 44/M | L | 44B3 | 1 | No | 90 |
| 32 | 19/M | L | 44B3 | 1 | Yes | 100 |
| 33 | 39/M | L | 44B3 | 3 | Yes | 84 |
| 34 | 47/M | R | 44B3 | 1 | No | 87 |
| 35 | 29/F | R | 44C1 | 2 | Yes | 90 |
| 36 | 31/F | L | 44C1 | 1 | Yes | 85 |
| 37 | 37/M | R | 44B3 | 2 | Yes | 88 |
| 38 | 22/F | L | 44B3 | 1 | Yes | 84 |
| 39 | 56/F | L | 44B3 | 1 | No | 87 |
| 40 | 41/F | R | 44B3 | 2 | No | 100 |
| 41 | 43/F | R | 44C1 | 1 | No | 72 |
| 42 | 34/M | R | 44B3 | 1 | Yes | 80 |
| 43 | 55/F | L | 44B3 | 1 | Yes | 81 |
| 44 | 44/M | R | 44C1 | 1 | No | 84 |
| 45 | 73/M | L | 44B3 | 1 | No | 78 |
| 46 | 43/F | L | 44B3 | 1 | Yes | 80 |
Table 2. Summary of the PM conservative group data and results.
Surgeries are performed by five surgeons. All of them are working in the same trauma section. Fixation of PM fragments which are smaller than 25% of the joint surface is still controversial so PM fixation was performed by surgeon’s decision. It was a subjective decision. Two surgical techniques were used while fixating PM. One of them is open reduction and internal fixation with 3.5 mm DCP plate. Posterolateral approach was chosen for this fixation. The other surgical technique was percutaneous anterior to posterior screw fixation. PM Fixation with posterior plate was used in 17 (63%) patients and percutaneous screw fixation was used in 10 (34%) patients.
Need for transsyndesmotic screw fixation is decided after malleolus fixation intraoperatively. Intraoperatively fluoroscopic external rotation stress test was applied to all patients after malleolus fixation. When tibiofibular and tibiotalar clear space was >1 mm from other side, stress test was defined as positive and transsyndesmotic screw was used.
Both groups were followed with partial weight-bearing after surgery. No cast was applied. Transsyndesmotic screws were extracted 6 weeks after surgery. There was no difference in post-operative rehabilitation protocol between two groups. Superficial infection was seen in 4 patients and treated with oral antibiotics. One patient had reflex sympathetic dystrophy and healed completely.
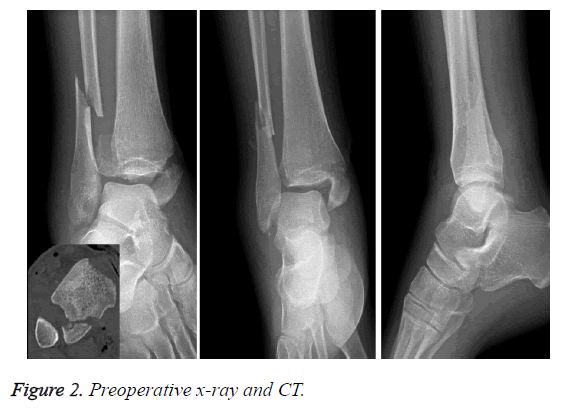
The length of the PM fracture measurement was conducted from preoperative lateral x-rays. PM fracture was classified according to Haraguchi classification from preoperative ankle CT [11]. Use of transsyndesmos screw was obtained from postoperative x-rays. American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hind foot score was used to evaluate the functional outcomes at the latest follow-up (Figure 2).
Data was analysed with SPSS 22.0 program. Mean, standard deviation, median, frequency and ratio values are used in the descriptive statistics of the data. The distribution of the variables was measured by the Kolmogorov Simirnov test. Independent sample t-test and Mann-Whitney u-test were used in the analysis of quantitative independent data. Chi-square test was used to analyse qualitative independent data, and fischer-test was used when chi-square test conditions were not met. This was a retrospective study. Sample size calculations were not conducted for that reason.
Results
In 27 patients with PM fixation, mean of preoperative PM fracture ratio was 20% ± 4.66% (15-25). Mean of AOFAS was 87.44 ± 5.67 (80-100). In 46 patients without PM fixation, mean of preoperative PM fracture ratio was 19.8% ± 4.54% (10-25). Mean of AOFAS was 87.22 ± 6.37 (72-100). In the PM fixation group, transsyndesmosis screw was used in 6 patients (22%). In the group where PM was not fixated, transsyndesmosis screw was used in 31 patients (67%).
The age, sex and side distribution of the patients in the PM fixation and conservative groups did not differ significantly (p˃0.05). AOFAS, Haraguchi classification, AO/OTA classification and PM ratio did not differ significantly. Use of transsyndesmotic screw in conservative group was significantly higher (p˂0.05) than PM fixation group. Correlation was found between PM ratio and Haraguchi type 1 and 2 fractures. Frequency in type 3 is statistically incompatible.
Discussion
Ankle fractures along with PM fracture have clinically worse outcomes [5,12,13]. Generally, in trimalleolar fractures, fixation of PM is determined according to the posterior fragment’s ratio to the ankle joint. In PM fractures which are less than 25% of ankle joint, conservative treatment can be chosen because the joint biomechanics is not altered and the functional results do not show difference [8,14,15]. However, there are publications in the literature claiming that, even if the posterior fragment is less than 25% fixation is recommended in order to maintain the syndesmotic stability [7]. Since there is a consensus on posterior fragment fixation which is for PM fragment size larger than 25% in trimalleolar fracture, in our study we evaluated the outcomes of the posterior fragments less than 25% of ankle joint in trimalleolar fractures. There are no certain criteria defined for PM fixation indication since cases do not belong to sole surgeons and study being retrospective one. However, there was no significant statistical difference found between PM fixation and without PM fixation groups in terms of demographic, fracture type, size and ratio.
In PM fixation, percutan screw or Open Reduction Internal Fixation (ORIF) can be used. O'Connor et al. claimed that using plate fixation can achieve better clinical results than A-P percutan screw with the posterolateral plate [16]. In our study, plate and open reduction was applied in 19 out of 27 patients in PM fixation group, whereas percutan A-P fixation with screw is used for the rest. Posterolateral incision was preferred for all of the patients whom plate was used. No statistically significant functional difference was found between screw and plate groups.
PM fractures are categorized into three types by Haraguchi et al. Haraguchi type 3 fractures were observed in the ratio of 5% similar to the previous studies [11]. Haraguchi type 2 fractures were 38%. No statistically significant difference in distribution of the patients was found between both groups (PM fixated and not) in terms of Haraguchi classification. On the other hand, there has been a correlation between Haraguchi classification type 1, type 2 fractures and PM ratio whereas there has been no correlation found for type 3. As for the reason why there has not been such a correlation for type 3 is related to less amount of patients with type 3. It is again mentioned in the literature that, PM accurate size is not calculated via plain radiographer because of fracture line variance [11,17].
It is indicated in the literature that PM fixation increases the sindesmosis stability [18]. The strongest part of syndesmosis is posteroinferior tibiofibular ligament (PITFL) [19]. The syndesmotic stability of the groups couldn’t be compared in our study. However, this is provided indirectly by comparing transsyndesmotic fixation need.
While transsyndesmotic screw was used 22% in the PM fixated group, in the group where PM is treated conservatively the ratio was 68%. The need for transsyndesmotic fixation in the PM fixation group was less. There was no statistically significant difference between Haraguchi classification and transsyndesmotic fixation. While the need for syndesmosis screw in Haraguchi type 1 and type 2 fractures are identical, the numbers of type 3 fractures are not considered adequate.
After transsyndesmotic fixation there is a need for screw removal and the second operation is likely to be occurred. There are studies in the literature related to the removal of syndesmosis screw [20]. It is thought that patients with PM fixation and transsyndesmotic fixation, PITFL’s rupture is distinguished from PM. Full load weight-bearing is not advised in transsyndesmotic fixation before removal of screw.
Different results have been identified in the literature when functional results are compared. Mingo et al. mentioned the importance of anatomic reduction and ORIF is suggested even if PM fracture ratio is smaller than 25% when the reduction is not enabled with ligamentotaxis [4]. However, there has been no significant difference found between Olerud and Molande scores. Drijfhout et al. emphasized that if PM fracture ratio is higher, osteoarthritis development increases and this risk is independent of PM fixation but there has been no significant functional difference found [8]. In our study, there was no statistically significant difference between both groups. Loss of score is mainly observed between function and pain parts. None of them had limitations during daily activities but during sports activities, they reported some limitations and rare pain. Because of the short follow-up time osteoarthritis development wasn’t observed in both groups.
Conclusion
There has been no significant functional difference found in trimalleolar fracture when PM fraction ratio is smaller than 25% in comparison of PM fixation, however, the decreased need of transsyndesmosis fixation needs to be taken into consideration. More prospective and randomized controlled studies are needed in this respect.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical Approval
Institutional review board approval was obtained prior to the study (IRB No. 19.04.2016-49).
References
- Jensen SL, Andresen BK, Mencke S, Nielsen PT. Epidemiology of ankle fractures: a prospective population-based study of 212 cases in Aalborg, Denmark. Acta Orthop Scand 1998; 69: 48-50.
- Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures: an increasing problem? Acta Orthop Scand 1990; 69: 43-47.
- Katioz H, Bombaci H, Gorgec M. Treatment of trimalleolar fractures. Is osteosynthesis needed in posterior malleolar fractures measuring less than 25% of the joint surface? Acta Orthop Traumatol Turc 2002; 37: 299-303.
- Mingo-Robinet J, López-Durán L, Galeote JE, Martinez-Cervell C. Ankle fractures with posterior malleolar fragment: Management and results. J Foot Ankle Surg 2011; 50: 141-145.
- De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg 2005; 44: 211-217.
- Irwin, Todd A, John L, Anish RK. Posterior malleolus fracture. J Am Acad Orthop Surg 2013; 21: 32-40.
- Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 2013; 447: 165-171.
- Drijfhout van Hooff CC, Verhage SM, Hoogendoorn JM. Influence of fragment size and postoperative joint congruency on long-term outcome of posterior malleolar fractures. Foot Ankle Int 2015; 36: 673-678.
- Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S. Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg 2016; 55: 140-145.
- Donken CC, Verhofstad MH, Edwards MJ, Schoemaker MC, van Laarhoven CJ. Use of an acrylic mold for mortise view improvement in ankle fractures: a feasibility study. J Foot Ankle Surg 2011; 50: 525-528.
- Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am 2006; 88: 1085-1092.
- Leyes M, Torres R, Guillen P. Complications of open reduction and internal fixation of ankle fractures. Foot Ankle Clin 2003; 8: 131-147.
- Jaskulka RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma 1989; 29: 1565-1570.
- Harper MC, Hardin G. Posterior malleolar fractures of the ankle associated with external rotation-abduction injuries. Results with and without internal fixation. J Bone Joint Surg Am 1988; 70: 1348-1356.
- Fitzpatrick DC, Otto JK, McKinley TO, Marsh JL, Brown TD. Kinematic and contact stress analysis of posterior malleolus fractures of the ankle. J Orthop Trauma 2004; 18: 271-278.
- OʼConnor TJ, Mueller B, Ly TV, Jacobson AR, Nelson ER, Cole PA. "A top" screw versus posterolateral plate for posterior malleolus fixation in trimalleolar ankle fractures. J Orthop Trauma 2015; 29: 151-156.
- Ebraheim NA, Mekhail AO, Haman SP. External rotation-lateral view of the ankle in the assessment of the posterior malleolus. Foot Ankle Int 1999; 20: 379-83.
- Miller AN, Carroll EA, Parker RJ, Helfet DL, Lorich DG. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res 2010; 468: 1129-1135.
- Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy 1994; 10: 558-560.
- Lalli TA, Matthews LJ, Hanselman AE, Hubbard DF, Bramer MA, Santrock RD. Economic impact of syndesmosis hardware removal. Foot 2015; 25: 131-133.