Case Report - Ophthalmology Case Reports (2021) Volume 5, Issue 1
Ocular tuberculosis-diagnostic difficulties and therapeutic features
Nicoleta Anton1,2, Ciprian Danielescu1,2*, Laura Popa2, Anisia Iuliana Alexa1,2, Alina Cantemir3, Camelia Margareta Bogdanici1,2, Roxana Elena Ciuntu1,2
1Department of Surgery, University of Medicine and Pharmacy "Gr. T. Popa", Iasi, Romania
2Ophthalmology Clinic "St. Spiridon", Iasi, Romania
3Ophthalmology Clinic "Oftaprof”, Iasi, Romania
- *Corresponding Author:
- Ciprian Danielescu
Department of Surgery University of Medicine and Pharmacy "Gr. T. Popa"
Romania"
E-mail: ciprian.danielescu@umfiasi.ro
Accepted date: July 10, 2020
Citation: Anton N, Danielescu C, Popa L, et al. Ocular tuberculosis-diagnostic difficulties and therapeutic features. Ophthalmol Case Rep. 2021;5(1):2-6.
Abstract
Intraocular Tuberculosis is a Granulomatous Chronic Infection with Mycobacterium tuberculosis with or without systemic involvement. It is a challenge to put a correct diagnosis and to establish a specific therapeutic protocol. We present the case of a patient with a history of Pulmonary Tuberculosis, with ocular signs and symptoms suggesting Intraocular Tuberculosis, a rare form of extra Pulmonary Tuberculosis. The chief complaints of the patient were: progressive loss of vision in the left eye for about 5 days, night sweating, oral ulcerations. Taking into account the infectious context, we requested a pneumologic consult. The thoracic X-ray was normal, the sputum examination was negative for M. tuberculosis and QuantiFERON: positive. Before initiating the therapy, we made an anterior chamber paracentesis for aqueous bacteriology test. Under anti-tuberculosis drugs and systemic steroids the visual acuity got better, we observed also a full recovery of visual field defects and the disappearance of retinal changes. Intraocular Tuberculosis is difficult to diagnose and, in general, it is a diagnosis of exclusion. Most of the patients with Ocular Tuberculosis don't have systemic manifestations. A delay in the diagnosis and treatment could lead to permanent loss of vision.
Keywords
TB ocular, Mycobacterium tuberculosis, Tuberculostatics, Corticosteroids, Choroiditis, Peripapillary edema.
Introduction
Intraocular Tuberculosis is a chronic granulomatous infection caused by Mycobacterium tuberculosis with or without systemic involvement. Making the diagnosis and establishing the specific therapeutic protocol represents a great challenge. It may involve whatever tissue of the eye and orbit. Ocular involvement can occur through direct inoculation or it can be an immunological reaction. Commonly, it occurs in an immunocompromised person. A certain diagnosis of tuberculosis can be confirmed by specific investigations like aqueous humour Polymerase Chain Reaction (PCR). However, the sensitivity and specificity of the tests are not strong enough, so the definitive diagnosis is difficult [1].
Case Report
We present the case of a 23-year-old patient, computer programmer, living in an urban environment, with a history of Pulmonary Tuberculosis, with ocular symptoms and suggestive aspects of Intraocular Tuberculosis, a rare complication of extrapulmonary infection with Mycobacterium tuberculosis.
Method and Materials
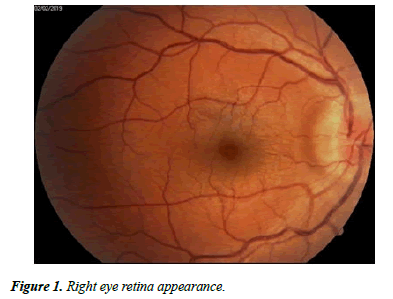
The patient presented on 31.01.2019 in the Ophthalmology Department of “Sf Spiridon” Hospital Ia?i complaining about progressive decrease of visual acuity in the left eye for about 5 days and associating symptoms such as profuse night sweats, oral ulcerations. The ophthalmological examination revealed: RE (right eye)=1 without correction, LE (Left Eye)=0.7 with correction (-0.75sf); dischromatopsy in the red-green axis in LE, normal chromatic sense in RE. Examination of the anterior segment revealed central round pupils, without afferent pupillary defect in any eye (Figure 1); normal ocular motility, and normal intraocular pressure.
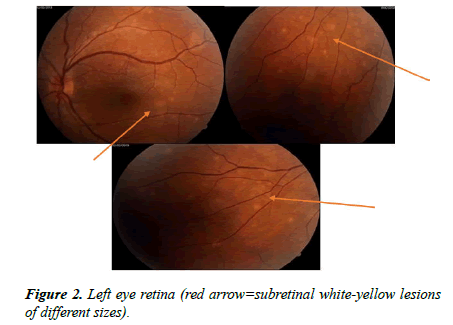
Fundus examination shows in the right eye: congestive optic disc not well outlined, with peripapillary edema; dilated veins, Case Report https://www.alliedacademies.org/ophthalmic-and-eye-research/ 2 Ophthalmol Case Rep. 2020 Volume 4 Issue 2 granular aspect of the macula (Figure 1); in the left eye not well outlined optic disc, dilated veins, macula without lesions, subretinal white-yellow lesions of different sizes in the inferior and nasal periphery, granular aspect of the macula (Figure 2).
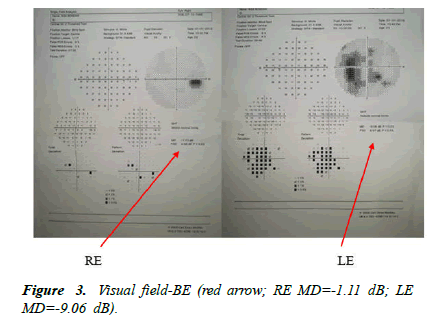
The visual field examination was normal for the right eye, but the left eye showed several absolute scotomas not well systematized (Figure 3). Taking into account the infectious context, we required a pulmonology consultation. The chest Xray was normal, sputum examination was negative for Mycobacterium tuberculosis and the lab tests including blood count, antibodies: anti-HIV, anti-citomegalovirus (Ig M, Ig G); anti-Toxoplasma gondii (Ig M, Ig G); anti-Borrelia burgdoferi (Ig M, Ig G); anti-herpes simplex IgM, IgG were normal. The angiotensin-converting-enzyme test was negative and ruled out sarcoidosis. We found positive: anti-Candida albicans IgG; anti-Ebstein-Barr Ig G, QuantiFERON test.
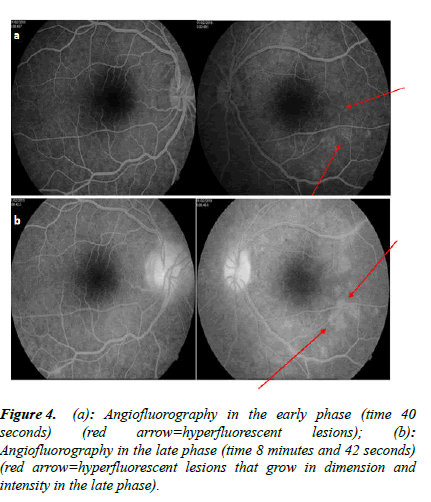
ENT, neurological, dermatological exams were normal. Fluorescein angiography showed an early phase in the left eye hyperfluorescent lesions that grow in dimension and intensity in the late phase (Figure 4a and 4b). Orbito-cerebral MRI (Magnetic Resonance Imaging) does not show the presence of a brain tumour.
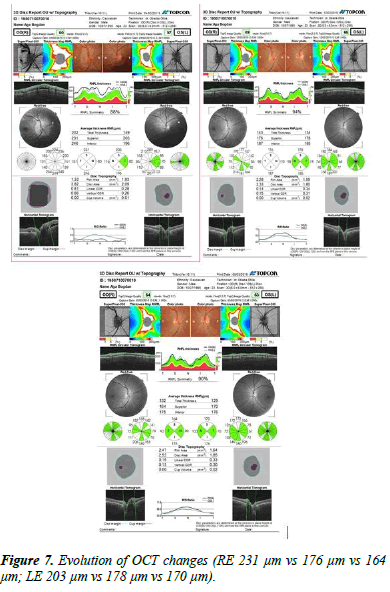
OCT exam revealed thickening of the retinal nerve fibre layer at BE with an average of 231 μm in the upper sector in RE and an average of 203 μm in LE. A 0.2 ml aqueous humour sampling from each eye was performed for bacteriological examination before initiating the therapy.
Before initiating therapy, it was necessary to exclude pathologies that have in common papillary edema and the presence of choroidal infiltrates. Multiple Evanescent White Dot Syndrome (MEWDS) is the main diagnosis, the presence of choroidal lesions, unilateral damage, mainly in women, is associated with mild vitreous, AGF early hyperfluorescent lesion, the appearance of the wreath. Acute posterior placoid epitheliopathy, often unilateral, with subsequent congenital eye damage, affects young people with a history of recent viral infection, may associate papillitis. Sarcoidosis, Granulomatous Inflammatory Disease, bilateral, has vitreous inflammation, perivascular, Periphlebitis, may also affect the optic nerve. All these conditions are excluded based on clinical and paraclinical investigations [2-4].
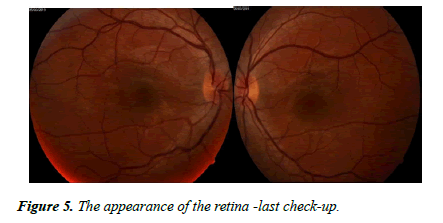
The therapy was started 9 days after the initial presentation with tuberculostatics according to the recommendations of the pulmonologist (Table 1) in association with pulse steroid therapy 1 g/day, 3 days, followed by oral steroids in decrease. The tuberculostatics treatment was according to the protocol for 9 months, and the corticosteroids were maintained for 3 months, with periodic ophthalmological and pneumological evaluation. The evolution under treatment was favourable with reduction of bilateral papillary edema, the subretinal lesions diminished in size and number, visual field improvement, increased visual acuity (Figures 5 and 6a and 6b).
| Rifampicin | 2 tablets/day |
| Pyrazinamide | 4 tablets/day |
| Ethambutol | 3 tablets/day |
| Ofloxacin | 4 tablets/day |
| Vitamin B6 | 1 tablet/day |
Table 1. Treatment with tuberculostatics according to the recommendations of the pulmonologist.
The OCT exam showed a reduction in the thickness of the retinal nerve fibre layer with an average of 176 μm in RE and 178 μm in LE (Table 2).
| Optic disc OCT | RE | LE |
|---|---|---|
| 4.02.2019 | 231 µm Sup, 246 µm inferior, 151 µm nasal, 180 µm temporal | 203 µm Sup, 196 µm inferior, 116 µm nasal |
| 12.02.2019 | 176 µm Sup, 187 µm inferior, 110 µm nasal, 98 µm temporal |
178 µm Sup, 185 µm inferior, normal Nasal, temporal |
| 7.03.2019 (last check-up) | 164 µm sup, 175 inferior, normal temporal, nasal | 170 µm sup, 176 µm inferior, normal nasal, temporal |
Table2. Evolution of RNFL (Retinal Nerve Fiber Layer) thickness.
In the last check-up (7.03.2019), visual acuity: 1 without correction (Figure 7).
There are few data regarding Intraocular Tuberculosis prognosis, despite this, it is reasonable to suppose that this type of infection requires a long drown treatment to eradicate the bacteria.
Discussion
Intraocular Tuberculosis is a chronic granulomatous infection with Mycobacterium tuberculosis with or without systemic involvement. Humans are the only natural host. It is spread primarily in the form of an aerosol that gains access to sensitive hosts through the lung and results in a latent infection in normally functioning immune systems. In about 5% of patients, the infection causes the disease in the first years after exposure. Intraocular Tuberculosis can be primary-when the entry of the bacillus is at eye level or secondary in case it appears as a result of the hematogenous dissemination from a distant or nearby focal point (sinus, cranial cavity). Ocular involvement occurs in approximately 1% to 2% of TB patients [5]. It is usually disguised as other infection. The distinguishing sign of extra-Pulmonary Tuberculosis is granuloma and necrosis. Extrapulmonary TB occurs either in combination with clinically apparent Pulmonary Tuberculosis or in isolation, without clinical or laboratory evidence of lung infection [6]. Extrapulmonary disease is common in immunocompromised patients, infants, and young children. Primary infection of the eye is very rare [1,2,7-9]. Primary infection can be transmitted through the air or by contaminated hands, molds, or exposure to dust or sputum particles that contain bacilli. TB events may not be clinically or radiographically visible [2].
The most common clinical manifestations of Intraocular Tuberculosis are choroiditis, retinal vasculitis, optic disc nodules, solitary or multiple choroidal nodules, anterior and posterior uveitis. The choroid is most commonly affected; at this level, the blood flow is the highest, representing an early sign of the spread of the disease, and may be associated with papillary edema, haemorrhages in the layer of retinal nerve fibres or macular star [2,3,10]. Our patient was known with an old history of Pulmonary Tuberculosis, still under the supervision of the pulmonologist. The diagnosis of ocular TB is difficult to make due to various clinical manifestations and because of laboratory results that are inconclusive. The thoracic X-ray was normal, the sample of aqueous humor collected being in small quantity wasn ’ t sufficient for PCR detection of the Koch bacillus, and the QuantiFERON test was positive. The presence at the ocular level of the multifocal choroiditis, associated with the important papillary edema, the history of Tuberculosis, the positive QuantiFERON test, the negative chest x-ray, negative sputum examination cannot exclude the diagnosis of ocular TB, which is the reason why, under the guidance of the pulmonologist, the therapy was started. The anti-inflammatory treatment was started 48 hours after initiation of tuberculostatic therapy. Ocular TB usually occurs in apparently healthy individuals. It is rarely observed in patients with active pulmonary disease. The results of chest radiography in patients with ocular TB are normal. The diagnosis of Ocular Tuberculosis is usually presumptive and depends on indirect evidence. The presence of a systemic tuberculosis infection strongly indicates but does not prove that tuberculosis is a cause of ocular manifestations. Abrams and Schlaegel reported that in 18 patients with suspected uveitis TB, chest X-ray showed no active or inactive evidence of TB [11].
The diagnosis of certainty is made by isolating the M. tuberculosis bacilli from the ocular tissues (vitreous aspirate, aqueous humoral puncture, or retinal biopsy). There are three diagnostic criteria for ocular TB according to the studies: confirmed ocular TB 1. At least a clinical sign suggestive for ocular TB, 2. Microbiological confirmation of ocular tissues; probable intraocular TB (1. At least a clinical sign suggestive for ocular TB, 2. Radiological/microbiological confirmation of extraOcular Tuberculosis, 3. History of TB exposure/ immunological evidence of TB) and possible intraocular TB (1+3+4 or 1+2) (1, 2, 3, 4. Non-suggestive chest x-ray for TB). In general, according to the American Thoracic Society, standard treatment includes four tuberculostatics over an 8- week period (Rifampicin, Isoniazid, Ethambutol, Pyrazinamide) followed by two medications at least 18 weeks (Rifampicin and Isoniazid) [12-14]. Corticosteroids can be used to control inflammation with gradually decreasing doses over 6-12 weeks, only in combination with antituberculosis drugs, otherwise, they may have catastrophic effects if tuberculosis is active. Several studies have reported a favourable response to ATT when co-administered with systemic corticosteroids in patients with suspected tuberculous uveitis [13-15]. The specific anti-tuberculosis treatment administered for 9-12 months is extremely effective and helps reduce recurrences in the eyes. According to these principles of treatment, we recommended to our patient 9 months of treatment with anti-tuberculostatic drugs, with favourable clinical evolution, evaluated by the disappearance of the ocular choroidian lesions and the papillary edema, the increase of the visual acuity to 100% and the normalization of the visual field reported at the time of diagnosis. According to the studies, the absence of the treatment could lead to: glaucoma, cataract, cystoid macular edema, choroidal neovascularization, and retinal vasculitis, etc. The duration of treatment was longer than in the World Health Organization strategy because the incidence of tuberculosis in our country remains high. In this case, the arguments that pleaded for the diagnosis of Ocular Tuberculosis were: the previous history of TB, the fulminant evolution of the ocular manifestations, the relatively rapid lateralization of the ocular lesions, and the very good evolution only after a few days after the double therapy. Combined therapy: tuberculostatics for 9 months and corticosteroids, established immediately and carefully followed, led to a very good evolution, with complete resolution of changes at the ocular level and improvement of visual function and, implicitly, of the quality of life of the patient with full socioprofessional reintegration.
Conclusion
Intraocular Tuberculosis is a diagnosis of exclusion, very hard to establish, but the history of exposure to M. tuberculosis advocates for this. Most patients with Ocular Tuberculosis have no other systemic manifestations of the disease. Delay in diagnosis or treatment can lead to loss of vision. In general, recurrent idiopathic uveitis, which does not respond to conventional therapy, may be suggestive of tuberculous etiology. The eye examination should be routinely considered in patients with suspected or proven TB. Early diagnosis and prompt treatment of Ocular Tuberculosis can prevent serious complications and loss of vision. On the other hand, tuberculosis should be considered as a differential diagnosis in cases of uveitis and should be investigated accordingly.
Conflicts of Interest
The author declares no conflicts of interest regarding the publication of this paper.
Contributions
All authors agree to be accountable for all aspects of the work, have drafted and revised the manuscript critically, and gave final approval of the final version.
References
- Patel A. A rare presentation of ocular tuberculosis: A case report. JOJ Ophthal. 2017;5(1):1-3.
- Liang L, Xu MF, Jiang FG. Ocular Tuberculosis. Am J Case Rep. 2009;10:231-35.
- Ahnood D, Madhusudhan S, Tsaloumas MD, et al. Punctate inner choroidopathy: a review. Surv Ophthalmol. 2017;62(2):113-26.
- Gupta V, Gupta A, Arora S, et al. Presumed tubercular serpiginouslike choroiditis: clinical presentations and management. Ophthalmology. 2003;110(9):1744-9.
- Donahue HC. Ophthalmologic experience in a tuberculosis sanatorium. Am J Ophthalmol. 1967;64(4):742-8.
- Glassroth J, Robins AG, Snider Jr DE. Tuberculosis in the 1980s. N Engl J Med. 1980;302(26):1441-50.
- Bukulmez A, Koken R, Melek H, et al. Presumed ocular Tuberculosis in an immunocompetent eight-year-old boy. Singapore Med J. 2009;50(3):120-3.
- Darrell RW. Nonmiliary tuberculosis presenting solely with a choroidal lesion. Ophthalmology. 1986;93(2):276.
- Dannenberg Jr AM. Pathophysiology: basic aspects. Tuberculosis and nontuberculosis mycobacterial infections. Saunders Company (ed 4). 1999:17-47.
- Sahu GN, Mishra N. Bhutia RC, et al. Manifestations in ocular Tuberculosis. Indian J Tuberc. 1998;45(3):153-55.
- Abrams J, Schlaegel TF Jr. The role of the isoniazid therapeutic test in tuberculosis uveitis. Am J Ophthalmol. 1982;94(4):511-5.
- Figueira L, Fonseca S, Ladeira I, et al. Ocular Tuberculosis: Position paper on diagnosis and treatment management. Rev Port Pneumology. 2017:23(1):31-8.
- Morimura Y, Okada AA, Kawahara S, et al. Tuberculin skin testing in uveitis patients and treatment of presumed Intraocular Tuberculosis in Japan. Ophthalmology. 2002;109(5):851-7.
- Shakarchi FI. Ocular Tuberculosis: current perspectives. Clin Ophthalmol. 2015;9:2223-7.
- Gupta V, Gupta A, Rao NA. Intraocular Tuberculosis: an update. Surv Ophthalmol. 2007;52(6):561-87.