Mini Review - Journal of Molecular Oncology Research (2021) Volume 5, Issue 1
Occult malignant lesions on screening mammograms: A single center experience.
Waqas Ahmad*, Hira Farooq, Khadija Nasir, Islah Ud Din
Department of Radiology, Shaukat Khanum Memorial Cancer Hospital and Research Center, Lahore, Pakistan
- Corresponding Author:
- Waqas Ahmad
Department of Radiology
Shaukat Khanum Memorial Cancer Hospital and Research Center
Lahore, Pakistan
E-mail: waqasrad@gmail.com
Tel: +923044485533
Accepted date: January 22, 2021
Citation: Ahmad W, Farooq H, Nasir K, et al. Occult malignant lesions on screening mammograms:A single center experience. J Mol Oncol Res. 2020;5(1):25-26.
Abstract
Aim: Breast cancer is the most common cancer in females and its emerging day by day. In our population, it is estimated to be found in every ninth woman via clinical examination or screening imaging including ultrasound, mammography and MRI in selected cases. Screening mammogram is suggested in all women above 40 years of age and younger with positive family history. Promoting screening mammograms helps in early detection, timely management and treatment at an early stage of the disease. The aim of the study was to detect the frequency of malignant breast lesions and suspicious calcifications during screening.
Materials and methods: Retrospective analysis of all screening mammograms for suspicious features via electronic data was performed in the women imaging unit from July 2018-July 2019.
Results: Out of all patients, 170 patients had lesions with suspicious features mostly falling in category 4 BIRADS and 39 females had category 5 BIRADS mammograms. Age ranges from 40- 50, 50-60 and 60 above were identified separately. 2 treated breast cancer patients had contra lateral tumors noted on follow up screening mammograms after many years.
Conclusion: Digital mammography improves early detection of breast cancer. Prevalence of malignancies in screening mammogram varies with age and helps in reducing morbidity of disease burden.
Keywords
Breast cancer, Screening, Mammogram.
Introduction
Breast cancer is one of the most common cancer affecting 2.09 million people worldwide and the most common cancer in females. Breast cancer risk factors include positive family history, age at menarche, late menopause, nulliparity, use of Hormone Replacement Therapy (HRT), increasing age, smoking and radiation exposure. Modalities used to screen breast lesions include breast ultrasound, mammogram, and Digital Breast Tomosynthesis (DBT) and MRI breast. Each screening modality has its own limitations. Ultrasound breast is operator dependant and requires expertise with associated possible risk of falsenegative results. Digital Breast Tomosynthesis (DBT) is not commonly available in less-resourced settings. MRI is an expensive and used for screening purpose only in selected patients. Most recommended routine breast screening for women, irrespective of being asymptomatic, is annual breast mammogram for all women age above 40 years and younger if there is a positive family history for breast cancer. In the case of breast lumps, screening is done by performing breast ultrasound in young females with age less than 30 years.
Pakistan has the highest rate of breast cancer incidence among Asian countries. In 2019, more than 90000 new cases of breast cancer were reported in Pakistan with an alarming number of mortality of more than 40000 patients due to breast cancer in a year. In the Pakistani population, the lifetime risk of breast cancer is estimated to be every ninth woman. They are diagnosed after a clinical examination or screening imaging including ultrasound and mammography. In our hospital, breast cancer screening is usually done by the mammogram. A study was performed to review the incidence of malignant lesions in screened asymptomatic patient’s age more than 40 with no prior history of a breast lump or family history.
Materials and Methods
Study design and population
A retrospective analysis of all screening mammograms in the women imaging unit from July 2018 to July 2019 via electronic data was performed. Family history, mammographic findings with BIRADS of 4 and above and age ranges were identified. Data was analyzed on SPSS format. Ethical approval from our institution was obtained.
Screening procedure
All digital mammograms were performed on GE system machine with a 70 μm pixel size and a 232 × 286 mm field of view. The standard Cranio Caudal (CC) and Medio Lateral Oblique (MLO) views of all mammograms with adequate diagnostic quality were reviewed by breast imaging fellow and a consultant. Mammographic findings were categorized as malignant lesion, pleomorphic suspicious calcifications, combination of both or architectural distortion.
Diagnostic work up
After identifying suspicious findings on mammograms, all patients were advised biopsy correlation for confirmation where solid lesions under ultrasound guided and calcifications under stereo guided core biopsies respectively. Two patients who were already treated breast cancer undergoing screening of contra lateral side for many years also had to undergo biopsy for confirmation.
Results
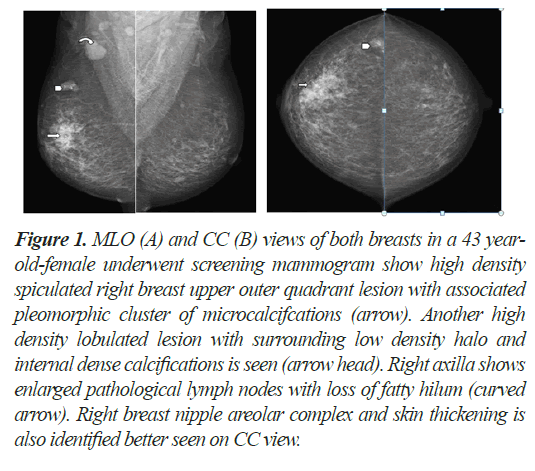
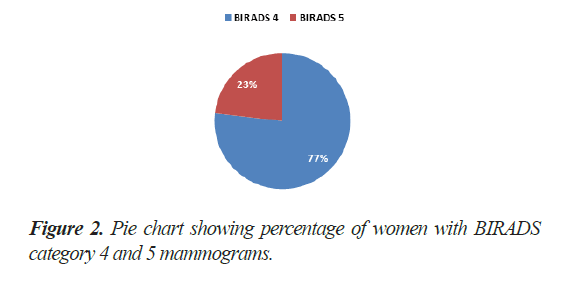
A total of 1079 patients over the age of 40 years and younger with positive family history underwent screening mammograms in the year July 2018 to July 2019. Out of these, 170 patients had unilateral or bilateral lesions with malignant morphological features with and without associated calcifications (Figure 1). 129 patients (77%) had BIRADS category 4 breast masses and remaining 39 patients (23%) had BIRADS category 5 mammograms (Figure 2).
Figure 1: MLO (A) and CC (B) views of both breasts in a 43 yearold- female underwent screening mammogram show high density spiculated right breast upper outer quadrant lesion with associated pleomorphic cluster of microcalcifcations (arrow). Another high density lobulated lesion with surrounding low density halo and internal dense calcifications is seen (arrow head). Right axilla shows enlarged pathological lymph nodes with loss of fatty hilum (curved arrow). Right breast nipple areolar complex and skin thickening is also identified better seen on CC view.
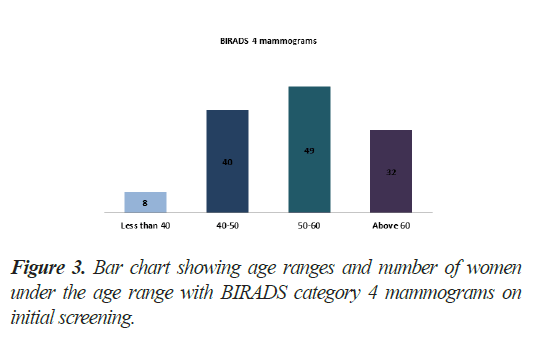
From patients with BIRADS category 4 mammograms, all patients had high density lesions. Alone suspicious calcifications were not seen in any patient. 40 patients had age range of 40-50 years while 49 patients fell in the range of 50-60 years. 32 patients were above 60 year of age. Remaining 08 patients below 40 had strong positive family history of breast carcinoma at age limits between 30s-40s (Figure 3).
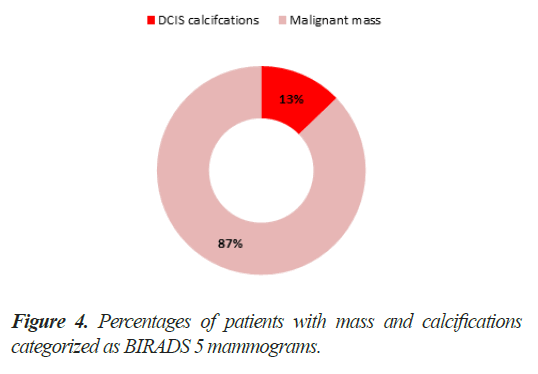
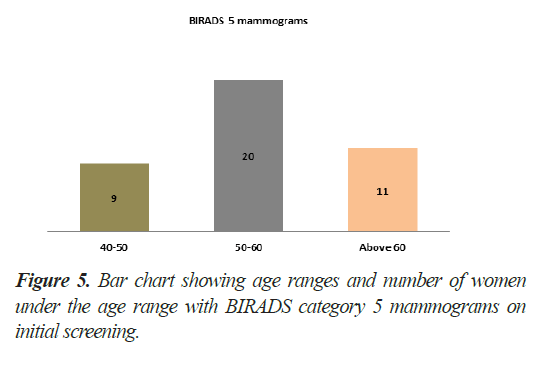
Regarding BIRADS category 5 patients, 05 patients (13%) had only suspicious calcifications of Ductal Carcinoma in situ (DCIS), rest of 34 patients (87%) had solid lesions (Figure 4). 09 patients were in range of 40-50 years while 20 patients fell in 50 to 60 years. A total of 11 patients were above the age of 60 years in this category (Figure 5). Only 2 patients of treated breast cancer had contralateral breast lesions with malignant features found and both were above 60 years of age.
Discussion
Breast cancer is one of the most common cancers in the world but it has a good 5-year prognosis 86%-99% if treated at an earlier stage [1]. Many methods have been devised to detect any abnormal breast lump or mass including selfbreast examination and clinical examination with imaging modalities including breast ultrasound, conventional 2-D mammogram, 3-D Digital Breast Tomosynthesis (DBT) and MRI breast. Of all these modalities, the mammogram is the standardized choice for breast screening due to its effectiveness in detecting small lesions and reproducible results. A mammogram uses X-rays to image the breast. It has been proven by evidence that mammography is helpful in the reduction of morbidity and mortality related to breast cancer [2,3]. Although Digital Breast Tomosynthesis (DBT) can produce more detailed images as compared to mammogram, According to USPSTF there is insufficient evidence to determine the benefits and harms of Digital Breast Tomosynthesis (DBT) to be used as the primary screening modality [4].
There are many guidelines established to perform routine screening of breast tissue for any abnormality. These guidelines vary in recommending the commencement age for screening and establishing the interval between two screenings. USPSTF and NHS recommend screening beginning at the age of 50 with a yearly or biennial interval [4]. American College of Obstetricians and Gynecologists (ACOG), American Cancer Society, National Comprehensive Cancer Network (NCCN) and NICE guidelines recommend yearly screening beginning at age 40 [5].
The discrepancy between age for initiation of screening is largely due to the fact that mammography has the harmful effect of radiation and there are fewer cases of breast cancer at a young age. So early age screening with mammography can lead to false-positive results and in turn be more harmful to the patient, earlier screening means more patients overburdening the resources and additional radiation exposure to breast over the years can lead to breast cancer. Radiation risk is the key ingredient hampering early age screening. Recently a modelled study has shown that the benefits of early screening beginning at 40 years far outweigh the harms done by the radiation exposure by 60-folds [6]. Our above-mentioned audit report also seconds this recommendation of initiation of early screening at age 40.
In most western countries proper breast screening has reduced the mortality due to breast cancer. In the United States, the number of breast cancer patients has increased in the past few decades but after implementation of proper early screening mammography the mortality has decreased. In Pakistan, non-existent proper regional guidelines, lack of awareness and stigma associated with breast cancer has hindered the screening process for the few decades leading to diagnoses at later stages contributing to poorer outcomes for the patient. There needs to be proper regional guidelines catering to the needs of the local population, increased awareness regarding breast cancer by running campaigns and educating masses about benefits of early detection and reducing the stigma by promoting the success stories and proper registration of breast cancer cases. Promoting screening mammograms will help in early detection, timely management and treatment at an early stage of the disease.
Conclusion
Digital mammography improves early detection of breast cancer. Prevalence of malignancies in screening mammogram varies with age and helps in reducing morbidity of disease burden.
Funding
No funding has been done for this study.
Conflict of interest
Authors have no conflict of interest.
Ethical approval
IRB approval obtained before start of this study as per requirement of ethical practices.
References
- Ruhl JL, Callaghan C, Hurlbut, A, et al. Summary Stage 2018: Codes and Coding Instructions. National Cancer Institute, Bethesda, MD, 2018.
- Whitman GJ. The role of mammography in breast cancer. prevention. Curr Opin Oncol. 1999;11(5):414-418.
- Mandelblatt JS, Cronin KA, Bailey S, et al. Effects of mammography screening under different screening schedules: Model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738-747.
- Bray F, Ren JS, Masuyer E, et al. Estimates of global cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer. 2013;132(5):1133-1145.
- Siu AL. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(4):279-296.
- Miglioretti DL, Lange J, van den Broek JJ, et al. Radiation- Induced Breast Cancer Incidence and Mortality from Digital Mammography Screening: A Modeling Study. Ann Intern Med. 2016;164(4):205-214