Research Article - Current Pediatric Research (2020) Volume 24, Issue 6
Nutritional counseling on modifying lifestyle practices of obese children
Samundeeswari Arunachalam1*, Maheswari K2
1 Department of Childhealth Nursing, Vinayaka Missions College of Nursing, Vinayaka Missions Research Foundation, Puducherry, India
2 Department of Child Health Nursing, Vinayaka Missions Annapoorna College of Nursing, Vinayaka Missions Research Foundation, Salem, India
Corresponding Author:
- Samundeeswari Arunachalam
Department of Childhealth Nursing Vinayaka Missions College of Nursing Vinayaka Missions Research Foundation Puducherry, India
Tel: 9442056146 Email: samu_mourougan@yahoo.co.in
Accepted date: December 01, 2020
Keywords
Obesity prevention, Childhood obesity, Lifestyle practices, Nutritional counseling.
Abstract
Worldwide prevalence of childhood obesity dramatically increases every year. To combat this obesity, parents play a key role. The present study focuses the effectiveness of nutritional counselling to prevent childhood obesity by assessing the lifestyle practices of obese children. Experimental research design with stratified random sampling method 150 obese school children (age group of 6-12 years) parents were called for interview to assess the lifestyle practices of their children. Nutritional counselling was given to the parents in 3 sittings and at the end of 6th month post assessment done. Statistical significance calculated by using one-way analysis of variance and student independent t-test. The study finding reveals more number of obese children in the age group of 6.1-8 years (39.19%). Their birth order two (56.66%) and two child family norm (71.67%). The obese children mother’s education was mostly higher secondary standard (42.50%) and was homemaker (78.33%). All obese children consuming non-vegetarian food and their frequency of intake is thrice a week (40%). The life style practices of obese during pre-test were poor (53.33%) and after nutritional counselling 65.83% of them scored good practice and 34.17% of them scored moderate practice. Nutrition counselling was very effective to parents of obese children who help them to adapt the healthy lifestyle practices preventing the obesity among children and prevent the increasing risk of obesity and chronic diseases in adult.
Introduction
Overweight and obesity is one among non-communicable diseases which will increases the morbidity among children and adolescents. The excess body fat is otherwise termed as obesity in terms of height and weight [1]. The term obesity defined and quoted over 95th percentile, but overweight is quantified between 85th and 95th percentile as per Indian study [2]. World Health Organization (WHO) report on obesity shows that worldwide obesity has tripled since 1975. The obesity threshold with BMI beyond 30 was observed in nearly 108 million children. The two largest population in the world viz., China and India were compared for obesity, where China leading with 15.3 million obese children. According to the latest statistics children and adolescent of age 5-19 were estimated to be over 400 million. The prevalence was increased from 18% in 2016 to 26% in 2018. This rise was noted equally among both girls and boys [3].
The Prevalence of childhood obesity shows that overweight increased from 9.7% to 13.9% between 2001 and 2010. The overweight and obesity were on the rising trend from 19.3% (2010) to 23.5% (2016). Hence, uphill trend of overweight and obesity among children/adolescents were noted [4]. Dramatic increase of prevalence of obesity mainly because of consumption of high calorie and high density foods, unhealthy food choices, physical inactivity, unhealthy lifestyle practices, over stress, poor parenting, parent lifestyle influences, lack of playground, media, school society influences and genetic factor [5]. Childhood obesity has been much correlated with diet and exercise, and the complex relationship between them and lifestyle practices indicate the significance of interventions [6,7]. The sedentary behaviors are highly associated with risk of mortality and psychological issues [8, 9]. The role of the parents played a pivotal point in promoting physical activity and eliminating sedentary lifestyle, by converting home environment and reducing the screen time [10,11].
The childhood obesity around the world is controlled by adopting proper intervention at school level along with diet and physical exercises [12]. Systematic reviews of childhood obesity prevention studies proved that interventions at school level was highly effective [13,14]. Educational interventions included behavioral change, nutrition, and physical activity is reckoned as a key tool to prevent being overweight and obesity, it significantly reduced body mass index (BMI) in obesity children [15].
The studies were conducted to assess the lifestyle practices of obese children with age group of 6-12 years among parents. The researcher interest is to give counselling to the parents of obese children about the healthy food, importance of avoiding junk food, adequate sleep and rest and finally the leisure and physical activities to the children to promote the healthy lifestyle practices. The effectiveness of nutritional counselling to change the lifestyle practices of obese children was also analyzed.
Materials and Methods
The research was quantitative in approach with experimental study which was conducted during 2017-2018. Total, 1256 school children with the age group of 6-12 years were screened for obesity, of which 209 children were obese. With the help of stratified random sampling method, 25 students from class I to VII were chosen and their parents were called for interview at school premises. The questionnaire has four domains such as healthy diet, avoidance of junk food, sleep and rest, leisure and physical activity. The overall practice score was classified as poor, moderate and good practice based on the score obtained by the study participants.
Inclusion criteria
• Obese children of 6-12 years
• Obese children of 90th percentile and above
• Parents willing to participate in the study
Exclusion criteria
• Obese children with the history of hereditary
• Chronic illness
Nutritional counselling was given to parents of obese children, to change the obese children lifestyle practices. Age proper sample menu plan such as calorie and nutrients based on Recommended Dietary Allowances (RDA) according to the age was distributed to the parents for providing proper diet with adequate calorie to their child. Followed by two counselling was given in weekly interval. After the last counselling, six-month follow-up was done to assess the children lifestyle practices in line with assessment conducted before counselling, to find the effectiveness of nutritional counselling on modifying the lifestyle practices preventing childhood obesity among parents of obese children.
Analysis was done suing IBM “Statistical Package for the Social Sciences” (SPSS) version 16 and Software for Statistics and Data Science (STATA) version 10 and Statistical Software for Epidemiology (Epi info) Version 3.5.1. Demographic variables in categorical/dichotomous were given in frequencies with their percentages. Practice score was given in mean and standard deviation. Quantitative variances between pre and post-test were measured by paired t-test. Qualitative dissimilarities between pre and post-test were evaluated using McNemar’s test. Effectiveness of the study was given in mean with 95% confidence interval and percentage with 95% confidence interval. Association between practice gain score with demographic variables was computed by one-way analysis of variance F-test and student independent t-test.
Results
In this study, 39.19% of obese children are at the age group of 6.1 to 8 years. With regard to standard of education, when compared to other standard, 18% of obese children are studying in class five. Regarding gender distribution, equal percentage (50%) of distribution were seen on both the sex. 71.67% of obese children family has two children with birth order two (56.66%) and they are residing in urban sectors (88.33%). With regard to father education, 26% of fathers are graduate or post-graduate, about mother’s education, 42.50% of them were studied higher secondary. 38.66% of fathers are unskilled worker but mothers are homemakers (78.33%). All children diet pattern was nonvegetarian and 40% of obese children are consuming nonvegetarian thrice a week.
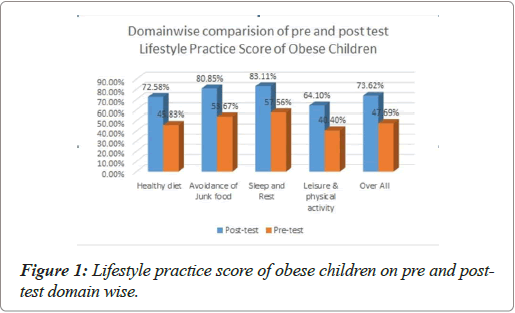
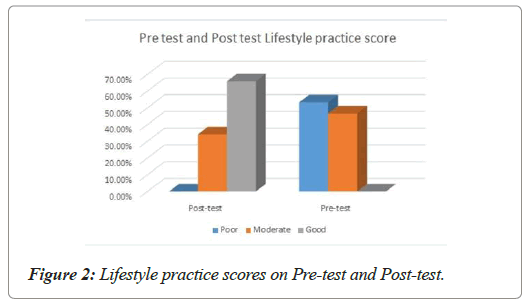
In pre-test, the lifestyle practice of obese children was 51.50 ± 6.98 and the mean percentage was 47.69%. The domain wise mean and standard deviation (SD) calculated as follows, Healthy Diet (HD) 16.50 ± 3.08, Avoidance of Junk Food (AJF) 17.71 ± 4.74, Sleep & Rest (S&R) 5.18 ± 1.69, and Leisure & Physical activity (L&PA) 12.12 ± 2.53. The Figure 1 shows the mean percentage of domain wise lifestyle practice score of obese children during pre and post-test. The nutritional counselling the lifestyle practice score was way ahead. The overall mean and SD was 79.51 ± 4.70 and the mean percentage was 73.62%. The domain wise post nutritional counselling mean and standard deviation were HD 26.13 ± 3.21 (Mean percentage 72.58%), AJF 26.68 ± 3.42 (Mean percentage 80.85%), S&R 7.48 ± 2.08 (Mean percentage 83.11%), L&PA 19.23 ± 4.03 (Mean percentage 64.10%). The Figure 2 depicts the overall pre and post-test life style practice score of obese children. From the Table 1 significant difference in pre and post-test lifestyle practice score with the t value of 38.43 at p=0.001 level were highlighted. The extended McNemar’s test was calculated for qualitative purpose, the result was shown with the significance c2= 51.02 at p=0.001.
| Life style practice on | Pre-test | Post-test | Mean difference | Student paired t-test | ||
|---|---|---|---|---|---|---|
| Mean score | SD | Mean score | SD | |||
| Healthy diet | 16.5 | 3.08 | 26.13 | 3.21 | 9.63 | t=25.91P=0.001***(S) |
| Junk food | 17.71 | 4.74 | 26.68 | 3.42 | 8.97 | t=19.57P=0.001***(S) |
| Sleep and Rest | 5.18 | 1.69 | 7.48 | 2.08 | 2.3 | t=9.77P=0.001***(S) |
| Leisure & physical activity | 12.12 | 2.53 | 19.23 | 4.03 | 7.11 | t=16.39P=0.001***(S) |
| Total | 51.5 | 6.98 | 79.51 | 4.7 | 28.01 | t=38.43P=0.001***(S) |
Table 1. Pre-test and post-test mean life style practice score of obese children.
The effectiveness of nutritional counselling were analyzed, and noted the significant mean difference and mean percentage of lifestyle practice score at 95% Class Interval (CI) between pre and post-test were 28.01 (26.56-29.45) and 25.93% (24.59- 27.27). The association was found between life style practice gain score and demographic variables such as age (F=3.12, P=0.05), education (F=2.49, P=0.02), children strength in family (F=3.08, P=0.05), birth sequence (F=3.91, P=0.03), mother education (F=2.46, P=0.05) and occupation (F=2.83, P=0.04).
Discussion
The results revealed the effectiveness of nutritional counselling on modifying the lifestyle practices of obese children to prevent childhood obesity. During pre-test, level of practice score were poor (53.33%) and moderate (46.67%) but after the nutritional counselling their post-test score level were moderate (34.17%) and good (65.83%). Social learning theory is well explained, change in parent’s behavior primes to modification in child’s deed [16]. Inclusion of parents as vigorous applicants with their children lead to marked improvement in weight control on longterm basis [17].
The children regularly ate take-away foods and fast food, indicating unhealthy dietary practices. The type of food consumed by school children can be oriented by advising a proper dietary pattern and with the help of nutritional campaign program. A school-based nutrition education campaign could have a positive impact on choices of food consumed. Obesity prevention and treatment can be linked on reducing the television screening there is a strong association between adiposity and high calorie intake of carbonated beverages [18]. According to “American Dietetic Association” obesity of children is directly linked to sweetened beverages which were supported in terms of reliable study, high and large quality data. Regular interview, motivation on change of diet plan and physical exercise in adult, started showing the reduction in obesity and treatment in children [19]. A decrease in BMI-z scores were noted in children from the study conducted by childcare health professional nurse on day-care teachers and parents [20]. A multidisciplinary approach (nutrition education/counselling, physical activity) is the most effective strategy to promote lifestyle changes and endorses that family association and noble support are the main reasons for healthier path [21-23]. Significant changes were illustrious before and after execution of nutrition counselling based on habits change on individual nutrition [24].
In one of the study the effective weight loss after nutrition counselling were noted and was due to counselling technique based on the stepwise behavioral change [25]. Thus, over all the study suggested that nutrition counselling was very effective in reducing the weight of obese children. Counselling should be given not only to the parents but also to the children of vulnerable group to understand and set the goal to reduce obesity and to promote the healthy lifestyle behavior pattern.
Conclusion
Healthy lifestyle practices promote the health status of the person. Parents are the real role model for their children. Parent lifestyle changes for adherence of healthy food choices, eating in, regular family meal timings, daily exercises and physical activity, less time on screen, avoidance of junk food, and sleep hygiene bring changes in children lifestyle practices. This nomenclature not only is followed by parents of obese children but also to all parents to keep healthy lifestyle practices and to promote good health status. Nearly 1/3rd of time children are in school, teachers also should take part to promote healthy lifestyle practices among children. Parent centric and school based intervention are very important to curb the obesity among school children.
References
- National heart, lung, and blood institute. Disease and conditions index: what are overweight and obesity? National Institutes of Health. Bethesda. 2010.
- Nawab T, Khan Z, Khan IM, et al. Influence of behavioral determinants on the prevalence of overweight and obesity among school going adolescents of Aligarh. Indian J Public Health. 2014;58(2):121-4.
- World health organization obesity and overweight fact sheet. WHO. 2016.
- Ranjani H, Mehreen TS, Pradeepa R, et al. Epidemiology of childhood overweight & obesity in India: A systematic review. Indian J Med Res. 2016;143(2):160-74.
- Sahoo K, Sahoo B, Choudhury AK, et al. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4(2):187-92.
- Taylor MJ, Arriscado D, Vlaev I, et al. Measuring perceived exercise capability and investigating its relationship with childhood obesity: a feasibility study. Int J Obes(Lond). 2016;40(1):34-8.
- Gray LA, Alava MH, Kelly MP, et al. Family lifestyle dynamics and childhood obesity: evidence from the millennium cohort study. BMC public health. 2018;18(1):500.
- Katzmarzyk PT, Church TS, Craig CL, et al. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998-1005.
- Owen N, Bauman A, Brown W. Too much sitting: a novel and important predictor of chronic disease risk?. Br J Sports Med. 2009;43(2):81-83.
- Sbruzzi G, Eibel B, Barbiero SM, et al. Educational interventions in childhood obesity: a systematic review with meta-analysis of randomized clinical trials. Prev Med. 2013;56(5):254-64.
- Ranucci C, Pippi R, Buratta L, et al. Effects of an intensive lifestyle intervention to treat overweight/obese children and adolescents. Biomed Res Int. 2017; 8573725.
- Bleich SN, Vercammen KA, Zatz LY, et al. Interventions to prevent global childhood overweight and obesity: a systematic review. Lancet Diabetes Endocrinol. 2018;6(4):332-46.
- Waters E, Silva-Sanigorski AD, Burford BJ, et al. Interventions for preventing obesity in children. Sao Paulo Med J. 2014;132(2):128-129.
- Wang Y, Wu Y, Wilson RF, et al. Childhood obesity prevention programs: comparative effectiveness review and meta-analysis. In database of abstracts of reviews of effects (DARE): quality-assessed reviews. Centre for reviews and dissemination.UK.2013.
- Wang X, Zhou G, Zeng J, et al. Effect of educational interventions on health in childhood: a meta-analysis of randomized controlled trials. Public health. 2018;164:134-147.
- Lachat C, Nago E, Verstraeten R, et al. Eating out of home and its association with dietary intake: a systematic review of the evidence. Obes Rev. 2012;13(4):329-46.
- Choudhury S, Omar O, Arora T, et al. Qatar obesity reduction study (QORS): Report on a pilot school-based nutrition education campaign in qatar. J Child Obes. 2018;S2:007.
- Alkon A, Crowley AA, Neelon SEB, et al. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health. 2014;14(1):215.
- Han JC, Lawlor DA, Kimm SY. Childhood obesity. The lancet. 2010;375(9727): 1737-48.
- Ho M, Garnett SP, Baur L, et al. Effectiveness of lifestyle interventions in child obesity: systematic review with meta-analysis. Pediatrics. 2012;130(6):e1647-e1671.
- Colquitt JL, Loveman E, O'Malley C, et al. Diet, physical activity, and behavioral interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database of Syst Rev. 2018;3(3):CD009728.
- Kraak VA, Liverman CT, Koplan JP. Preventing childhood obesity: health in the balance. Environ Health Perspect. 2005;113(10):A706.
- Anderson PM, Butcher KF. Childhood obesity: trends and potential causes. Future child. 2006;16(1):19-45.
- Kim BH, Lim H. Effects of customized nutritional education change 10 habits program according to stage of behavior change in mildly obese adults. J Korean Diet Assoc. 2015;21(3):215-26.
- Kim BR, Seo SY, Oh NG, et al. Effect of nutrition counseling program on weight control in obese university students. Clinical Nutr Res. 2017;6(1):7-17.