Research Article - Biomedical Research (2017) Volume 28, Issue 19
Nurses assisted linked color imaging chromoendoscopy improves colonic polyp detection rate
Yang Xu, Weiqing Shi, Xueting Zhang, Hanqin Zhang, Teng Yang, Aitong Li and Ranyun Zhou*
Department of Gastroenterology, 307 Hospital, Beijing, PR China
Accepted date: September 18, 2017
Abstract
Objective: Linked Color Imaging (LCI) is a newly developed endoscopic imaging technique, which has been proved to be able to improve the diagnostic efficacy. Here, we aimed to investigate the effects of nurses assisted LCI chromoendoscopy on the detection of colonic polyp.
Methods: A total of 200 patients who underwent colonoscopy from August 2015 to October 2016 in our endoscopy center were enrolled and randomized into White Light (WL) group, WL intervention group, LCI group and LCI intervention group. Endoscopic nurses assisted the endoscopists in completing the procedures in WL intervention and LCI intervention group. The polyp detection rate was compared and the characteristics of the polyp were analysed.
Results: The polyp detection rate in LCI intervention group was significantly higher than those in LCI group and WL group (P<0.05). The left and right colonic polyp detection rate in intervention groups were both higher than those in non-intervention groups.
Conclusion: Nurses assisted LCI chromoendoscopy could greatly improve the colonic polyp detection rate.
Keywords
Colonic polyp detection, Endoscopic nurses, Linker color imaging, Colonoscopy
Introduction
Colonoscopy is a useful method for diagnosing and treating colorectal cancer. In recent years, as more attentions have been paid to the screening and surveillance of colorectal cancer, the number of colonoscopy has been on the increase [1]. In addition, how to guarantee the quality and improve the detection rate is still the focus of the researches. In fact, there are a series of different factors that could influence the detection rate, including gender, age, withdrawal time, bowel preparation, and endoscopic device [2,3].
Linked Color Imaging (LCI) is a new endoscopic imaging technique, which simultaneously combines the blue laser and white to achieve a high brightness [4]. LCI mode can clearly observe the mucosal surface vessels and structure, and make the red areas redder and white areas whiter. This color enhancement is able to help the endoscopists detect the changes of the mucosal vessels and structure easily and confirm the corresponding diagnosis [5]. Previous studies indicated that the assistance from the nurses may influence the detection rate during endoscopic examination, and this may alleviate the patients’ discomfort [6,7]. In this study, we analysed the effects of nurses assisted LCI chromoendoscopy on the colonic polyp detection rate, by evaluating and comparing the detection rate and missing rate. These results could provide useful evidence for modifying the current endoscopic diagnostic and therapeutic strategy.
Patients and Methods
Patients
A total of 200 patients who underwent colonoscopy from August 2015 to October 2016 in our endoscopy center were enrolled. If the patients had contraindications for colonoscopy, had multiple colonic polyps (≥ 15), had poor bowel preparation, were diagnosed as inflammatory bowel diseases or did not undergo the whole colonoscopy examination, they were excluded from the study.
This study was approved by the Ethic Committee of 307 hospital. All the patients gave their written informed consent.
Study design
All the patients were randomized into White Light (WL) group, WL intervention group, LCI group and LCI intervention group. In WL group and LCI group, the colonoscopy was completed by the endoscopists alone and the nurses did not provide assistances in evaluating the bowel preparation and observing the location and size of the lesions during the withdrawal. In WL intervention group and LCI intervention group, the nurses assisted the endoscopists during the procedures, both of whom evaluated the bowel preparation and observed the location and size of the lesions. Endoscopic nurses assisted the endoscopists in completing the procedures in WL intervention and LCI intervention group. The polyp detection rate was compared and the characteristics of the polyp were analyzed. The endoscopists and nurses had experiences of over 2 years.
Bowel preparation
The patients had liquid diet 1 night before the colonoscopy. Compound polyethylene glycol electrolyte was administrated for bowel preparation. Boston score was used to evaluate the bowel preparation. It was considered to be qualified if Boston score ≥ 5.
Statistical analysis
All the statistical analysis were conducted using SPSS 17.0 software (SPSS Inc., Chicago, USA). The categorical and continuous data were shown as percentage and mean ± standard deviation, and the differences were compared using independent student t-test and chi-square, respectively. A two tailed P value less than 0.05 was considered to be statistically significant.
Results
Demographic and clinical characteristics
There were 50 patients in each group. In WL group, there were 26 men and 24 women, and the average age was 51.32 ± 5.2 y old. In WL intervention group, there were 33 men and 17 women, and the average age was 53.11 ± 2.5 y old. In LCI group, there were 35 men and 15 women, and the average age was 52.16 ± 1.9 y old. In LCI intervention group, there were 28 men and 22 women, and the average age was 55.25 ± 1.2 y old (Table 1). No statistically significant differences on the age, gender, withdrawal time and indications for colonoscopy were found among the groups (P>0.05).
| WL group (n=50) | LCI group (n=50) | WL intervention group (n=50) | LCI intervention group (n=50) | P value | |
|---|---|---|---|---|---|
| Age, years | 51.32 ± 5.2 | 52.16 ± 1.9 | 53.11 ± 2.5 | 55.25 ± 1.2 | 0.821 |
| Gender (male/female) | 26/24 | 35/15 | 33/17 | 28/22 | 0.614 |
| Boston score | 7.19 ± 1.3 | 7.11 ± 1.2 | 7.11 ± 1.5 | 7.13 ± 1.1 | 0.827 |
| Withdrawal time | 11.12 ± 1.1 | 10.17 ± 2.3 | 12.35 ± 2.0 | 10.56 ± 1.7 | 0.463 |
| Indications | |||||
| Routine examination | 19 | 15 | 23 | 19 | 0.259 |
| Clinical symptoms | 15 | 18 | 16 | 17 | 0.831 |
| Other | 16 | 17 | 11 | 14 | 0.475 |
Table 1: Demographic and clinical characteristics.
Polyp detection rate
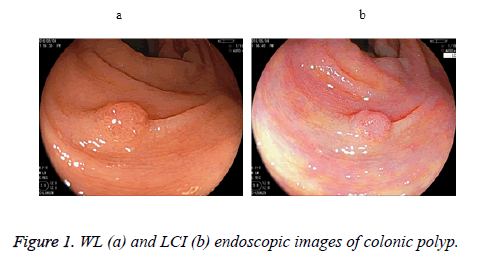
The polyp detection rate in LCI intervention group was significantly higher than that in LCI group, which in WL intervention group was significantly higher than that in WL group (P<0.05) (Table 2 and Figure 1). LCI intervention group had significantly higher polyp detection rate than WL intervention group (P<0.05).
| WL group (n=50) | LCI group (n=50) | WL intervention group (n=50) | LCI intervention group (n=50) | P value | |
|---|---|---|---|---|---|
| No. of patients with colonic polyp, n | 22 | 29 | 25 | 33 | |
| Polyp detection rate, % | 50 | 58 | 54 | 64 | 0.004 |
Table 2: Polyp detection rate.
Endoscopic features of polyps
The left and right colonic polyp detection rate in intervention groups were both higher than those in non-intervention groups (Table 3). LCI had better differentiation for size and location of polyps and the intervention from nurses also contribute to the improvement of endoscopic diagnostic efficacy.
| WL group (n=50) | LCI group (n=50) | WL intervention group (n=50) | LCI intervention group (n=50) | |
|---|---|---|---|---|
| Pathological diagnosis, n | ||||
| Neoplastic polyp | 3 | 5 | 4 | 5 |
| Inflammatory polyp | 8 | 9 | 12 | 16 |
| Hyperplastic polyp | 10 | 11 | 7 | 6 |
| Cancer | 1 | 4 | 2 | 6 |
| Diameter, n | ||||
| <5 mm | 13 | 17 | 14 | 20 |
| 5-9 mm | 7 | 9 | 9 | 11 |
| ≥ 10 mm | 2 | 3 | 2 | 2 |
| Location of polyp, n | ||||
| Left colon | 14 | 16 | 12 | 19 |
| Right colon | 8 | 13 | 13 | 14 |
Table 3: Characteristics of polyp.
Discussion
In recent years, the prevalence and mortality of gastrointestinal tumors have been on the increase all over the world [8]. Although great progress has been made on the conservative therapy, surgical resection remains to be the main treatment for such malignancies. Endoscopic resection can be used to detect and treat early cancer and precancerous lesions in gastrointestinal tract, which may play an important role in reducing the occurrence and mortality [9]. The changes of mucosal color and morphology provide valuable evidence for the endoscopic diagnosis of gastrointestinal diseases, and image enhancement endoscopy techniques including NBI, FICE, BLI and LCI greatly improve the diagnosis of early cancer and precancerous lesions [10,11]. WL could not observe the mucosal surface vessels clearly. LASEREO system, as a newly developed endoscopic system, combines the laser and unique image processing to obtain a clear observation of mucosal surface vessels and ultrastructure [12]. LCI is a color enhancement technique added to LASEREO system. LCI makes the red areas redder and the white areas whiter and minor color changes can be identified under LCI mode [13,14].
In this study, the data proved that polyp detection rate in LCI intervention group was higher than that in LCI group, and polyp detection rate in WL intervention group was higher than that in WL group, indicating that nurses assisted colonoscopy can improve the detection rate of polyp and adenoma, which was consistent with the previous report [15,16]. Polyp detection rate in LCI group was higher than those in WL group and WL intervention group, suggesting that LCI combines narrow band laser and white light to increase the brightness of the images. This can improve the differentiation of flat colonic adenoma by emphasizing the color changes. Compared with WL intervention group, LCI intervention group had higher polyp detection rate. These data showed that nurses assisted LCI colonoscopy may be an optimal strategy for diagnosing gastrointestinal mucosal lesions. What’s more, the intervention can improve the detection of left colonic polyp more significantly than right colonic polyp. The possible reason may be that the complex structure of sigmoid colon makes the polyp prone to be neglected. Thus, close observation of left colon is highly recommended.
The advancement of endoscopic technique promotes the development of endoscopic nursing. The application of LCI in clinical practice needs to be further validated. The optimization of the current endoscopic technique will maximally improve the polyp detection rate, which is the key to guarantee the colonoscopy quality, improve the endoscopic diagnosis and prevent colorectal cancer.
References
- Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJ. Colorectal cancer screening: a global overview of existing programmes. Gut 2015; 64: 1637-1649.
- Sano Y, Byeon JS, Li XB, Wong MC, Chiu HM5. Colorectal cancer screening of the general population in East Asia. Dig Endosc 2016; 28: 243-249.
- Robertson DJ, Kaminski MF, Bretthauer M. Effectiveness, training and quality assurance of colonoscopy screening for colorectal cancer. Gut 2015; 64: 982-990.
- Fukuda H, Miura Y, Hayashi Y. Linked color imaging technology facilitates early detection of flat gastric cancers. Clin J Gastroenterol 2015; 8: 385-389.
- Dohi O, Yagi N, Onozawa Y. Linked color imaging improves endoscopic diagnosis of active Helicobacter pylori infection. Endosc Int Open 2016; 4: 800-805.
- Min M, Deng P, Zhang W. Comparison of linked color imaging and white-light colonoscopy for colorectal polyp detection: a multicenter, randomized, crossover trial. Gastrointest Endosc 2017.
- Sun X, Dong T, Bi Y. Linked color imaging application for improving the endoscopic diagnosis accuracy: a pilot study. Sci Rep 2016; 6: 33473.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016; 66: 7-30.
- Garborg K. Colorectal cancer screening. Surg Clin North Am 2015; 95: 979-989.
- Cho JH. Advanced imaging technology other than narrow band imaging. Clin Endosc 2015; 48: 503-510.
- Subramanian V, Ragunath K. Advanced endoscopic imaging: a review of commercially available technologies. Clin Gastroenterol Hepatol 2014; 12: 368-376.
- Okada M, Sakamoto H, Takezawa T. Laterally spreading tumor of the rectum delineated with linked color imaging technology. Clin Endosc 2016; 49: 207-208.
- Ono S, Abiko S, Kato M. Linked color imaging enhances gastric cancer in gastric intestinal metaplasia. Dig Endosc 2016.
- Suzuki T, Hara T, Kitagawa Y. Magnified endoscopic observation of early colorectal cancer by linked color imaging with crystal violet staining (with video). Gastrointest Endosc 2016; 84: 726-729.
- White S. Interventional ERCP: techniques and nursing care. Aust J Adv Nurs 1990; 8: 22-29.
- Dokoutsidou H, Karagiannis S, Giannakoulopoulou E. A study comparing an endoscopy nurse and an endoscopy physician in capsule endoscopy interpretation. Eur J Gastroenterol Hepatol 2011; 23: 166-170.