Research Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2017) Volume 7, Issue 60
Non-Invasive Glucose Estimation Based on Near Infrared Laser Diode Spectroscopy
Mercy Adusei Boatemaa1* and Srinath Doss2
1Department of Biomedical Engineering, Faculty of All Nations University College, Ghana
2Faculty of Computing, Botho University, Botswana
- *Corresponding Author:
- Mercy Adusei Boatemaa
Faculty of All Nations University College
Department of Biomedical Engineering, Ghana
E-mail: abmercy14@gmail.com
Accepted on February 10, 2017
Abstract
Diabetes mellitus (DM) is a serious disease that affects not only the patient’s internal organs, circulation system and eyesight, but also their entire body. There are reportedly more than 120 million diabetic patients in the world at the moment and this figure is expected to double within the next ten years. India is the country with the highest rateof diabetes patient, with a current figure of 50.8 million. Modern laser diode spectroscopy is becoming important in medicine. The aim of this paper is to design a finger plethysmograph to measure (estimate) blood resistivity which relate to the amount of glucose level in the blood. The device construction consist of: laser Diode around 650 nm wavelength, Laser Driver, Voltage regulator (2), stepdown transformer (9v), Bridged rectifier circuit, photodetector (2), amplifier, ADC, microcontroller (Arduino Uno) and LCD to display the signal intensity. The device has been constructed in such a way to insert right index finger of the subject in-between the laser diode source and the photodetector. The signal intensity (V) were measured and different known glucose concentration as well as the in vivo calibration and the regression equations was obtained to help estimate the best fitting model (linear curve) and estimated values were correlated in validating the device with the biochemistry method. About 30 subjects aged 10 to 50 years were participated in FBS (fasting blood sugar) clinical study so far. The result of this new approach really shows a promising method for noninvasive measurement of blood glucose level to aid diabetic patients more painless, comfortable and bloodless life style
Keywords
Glucose, Photodetector, Diabetic mellitus, Non-invasive
Introduction
Diabetes mellitus (DM) is a serious disease caused by diminished effectiveness endogenous insulin characterized by hyperglycaemia, deranged metabolism and unhealthy life activities. It has a gradual onset of developing stage and is caused by impaired insulin secretion and insulin resistance so those with type 2 diabetes need insulin treatment and management [1,2]. The DM is associated with excess body weight and physical inactivity. They affect not only the patient’s internal organs, circulation system and eyesight, but also his entire body. It has been reported that more than 120 million diabetic patients are in the world at the moment and this figure is expected to double within the next ten years [3-5]. The most important thing for diabetes management is to monitor the patient's blood glucose level within 24 h a day and knowing the glucose level assists in determining the right diet and medical treatment. The current method available is invasive and liable to afflict some degree of pain and causes some skin injury [6,7].
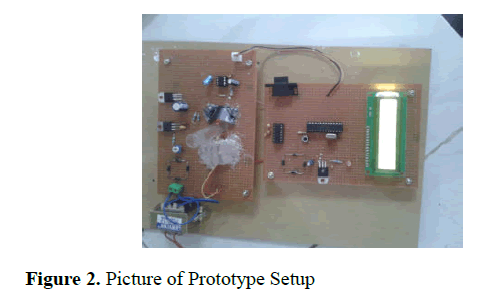
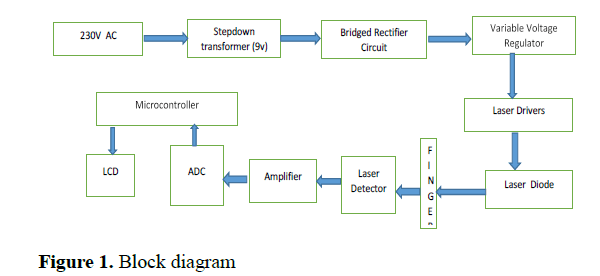
The type 2 diabetes drug market has increased in value by 145% in just 10 years, while prevalence of the condition across India and China is likely to increase to worrying levels, predicted by research and consulting firm Global Data [8]. Some people in the world are affected by this disease not neglecting racism however there is an increased prevalence in the people of South Asia, Africa and American-Indian ancestry. India is the country with the most people with diabetes, with a current figure of 50.8 million, followed by China with 43.2 million [6,8-10] (Figures 1and 2).
Modern diode laser spectroscopy is becoming very important in medicine. Previously the application of diode laser was used in the field of Process Control, Fire Detection, Space Missions, Petrochemistry and non-invasive breath test which is used to detect Helicobacter pylori infections in humans [11,12]. The medical application of diode laser is driven by the recent advances in diode laser technology and it unique characteristics; monochromaticity, coherence, directionality, wavelength is directly proportional to operating temperature and has an excess lifetime, sensitivity, miniaturization, and low cost have yielded fine applications related to blood glucose concentration measurement [13-15]. Recently diode laser has been an entrenched technique for detection and measurement of substance. The type of laser diode implemented in this paper was He-Ne red diode laser at 650nm wavelength.
The major technical principle behind this work is to implement the existing photoplethysmography principle of pulse oximeter to estimate glucose concentration where a patients percentage of oxygen saturation is measured using a device with two LEDs sensors and a detector placed on the fingertip or earlobe of a patient to measure the light absorbance rate of the two light source due to the pulsing of arterial blood flow. There is an electronic processor fitted in the device capable of calculating the ratio of the red and infrared light measured based on Beer- Lambert Law and the ratio finally converted into saturation of peripheral oxygen (SpO2) which literally shows the hemoglobin concentration level in a patient. With the same principle and with a specify components listed below a prototype of noninvasive glucometer has been proposed and designed. The aim of this paper is to design a finger plethysmograph to measure (estimate) blood resistivity which relate to the amount of glucose level in the blood (Figures 3 and 4).
Problem statement of the research
The diabetes mellitus is a major cause of mortality and morbidity globally. However the current method for monitoring blood glucose is biochemistry method (GOD and POD method) and finger pricking which have become discomfort, fear and pain to patients since they have to monitor their blood glucose level severally within a day. The current device of blood glucose monitor requires a sample of patient’s blood in order to determine glucose level each time which usually arrived at blood collection or self-induced finger pricking using lancet. The sampled blood is placed on a small test strip and inserted into the glucometer say Accu-chek which provides an electronic pulse to the device showing the reaction on the strip that finally display a digital readout of the amount of glucose in the blood in mg/dL. Because of the associated inconvenience and pain of this method, a more user-friendly non-invasive method is desired and hence a proposed prototype has been designed.
This research is to study and design a prototype of a device capable to provide an innovative idea to solve the existing problems using diode laser spectroscopy to help diabetic patient overcome the current glucose meter technique. To be able to implement this, a simple finger plethysmograph device has been designed to predict blood glucose concentration as a means for type 2 diabetes management.
Materials and Methodology
Materials, laser output and absorption field
The materials used in implementing this idea are: laser Diode around 650nm wavelength, Laser Driver, Voltage regulator (2), stepdown transformer (9v), Bridged rectifier circuit, photodetector (2), amplifier, ADC, microcontroller (Arduino Uno) and LCD. The laser beam is directed towards the tissue which is under study and where absorption and scattering occurs during measurement. A portion of the total scattered radiation was brought to impinge on the surface of a photodetector. Since an effective radiation penetration depth is approximately 1 millimeter in soft tissue [2], scattering and absorption takes place primarily in the papilla region and the underlying corium of two dermal layers contain many complex interrelating capillary network of the skin.
Brief method implemented: A noninvasive glucose measurement has been proposed through a process of signal intensities transmitted through or reflected by the stratum Cornea, dermis layer, epidermis layer, subcutaneous tissue, interstitial fluid and blood vessel of which both arterial and venous blood are taken into account. We overcame this problem by means of the following steps: (a) A known glucose concentration was used to estimate regression equation to plot the best fitting curve for estimation of glucose concentration in vitro.
(b) Collecting non-invasive signal intensity from non-diabetic individuals and diabetic patients using the proposed kit.
(c) Blood sample was taken from the same subjects invasively and the glucose oxidase method (GOD and POD method) of estimation of glucose concentration was done.
(d) Computing the values based on the correlation between measured blood glucose values and non-invasive signal intensities and a graph is plotted.
Brief Biochemistry method of glucose level estimation: Glucose Oxidase method (GOD and POD method)
This method is the current method employ in the clinical estimation of blood glucose concentration by an auto analyzer machine which has the working principle of photocolorimeter. The glucose oxidase is a glucose enzyme which catalyzes the oxidation of Beta D-glucose present in the plasma to D glucono- 1, 5-lactone with the formation of hydrogen peroxide and the lactone is slowly hydrolysed to D-gluconic acid. The hydrogen peroxide is broken down into oxygen and water by a peroxidase enzyme. The oxygen is the reacted with oxygen accepter (ortho toluidine) which gives out a colored compound that is measured as glucose concentration in the blood serum.
After the blood sample collected is centrifuged, the heaviest blood particles settle down in the test tube in accordance of the sizes. Blood serum which settles at the topmost of the centrifuged blood is taken about 50ml of it and the glucose oxidase and perioxidase enzymes are reacted with the blood serum which contains most of the glucose in the blood composite [7,16].
Biological theory behind the principle implemented
When there is high blood flow in the body the blood pulses through the finger and the red blood cells align themselves and as current passes through in such condition, there is always less resistance of current as compared to when there is lower blood flow in the body. However, when there is a lower blood flow the red blood cells misalign themselves. They tend to clumps together and become difficult for current to pass through with ease. Hence the resistance to current in blood flow determines electrical impedance of the laser in near infrared spectrum to the skin (finger) which relate to the signal intensity of blood glucose. Higher levels of blood glucose would result in greater misalignment or clumping of the red blood cells and there will be a higher resistivity. This paper aims at correlating the differences in the impedances and resistivity measurements with the varying glucose level taking into account of the arterial changes in volume of blood vessel during a blood pulse.
Block diagram
2
Skin light properties and NIR laser interaction on human skin
The human skin is a multilayered organ. Basically the skin is made up of stratum coeneum, dead cells and it the outmost layer of the skin, usually 0.01 to 0.020 mm thickness, epidermis (0.6 to 3 mm thickness), dermis (papillar dermis and reticular dermis which consist of the blood vessels, connective tissueetc and hypodermis (subcutanouse tissue) which are adipose tissues. The absorption property of skin is from a melanin, a natural pigment of type’s red/yellow phaeomelanin and brown/black eumelanin. The fluence rate of blood decreases as we get deeper into the skin. Another skin chromophore called hemoglobin absorps light and gives blood it reddish colour.
Normally the hemoglobin concentration in whole blood is 134 g/L to 173 g/L [17]. The factors that influence the optical pathway in humans are the tissue type, the absorption coefficient (wavelength) and the geometry of optodes. The specified wavelength of diode laser used is 650 nm which shows the best absorption of glucose in near infrared spectrum without absorbing hemoglobin and water in human tissue. The absorption window of NIR is 650 nm to 1350 nm maximum depth of penetration in tissue (skin). The dominant light tissue interaction here is scattering. The higher the scattering, the higher the distance travelled by the photons and the higher the probability of absorbed photons increases. Absorption coefficient is defined as the probability of a photon absorbed in tissue per unit path length which differs per different tissues.
The hemoglobin concentration in the blood consists of Hb and HbO2 which both has different absorption coefficient. The scattering of Laser light is the probability of photon scattering in tissue per unit path length [2,16]. This occurs due to mismatches in the refractive index of different tissue component including cell membranes and whole body cells. The scattering occurs due to biological factors such as: aging of skin and hydration of skin. Usually about 5-7% approximate light incident on the stratum Corneumis reflected back to the environment and the rest transmitted to the internal tissues [18].
Glucose can affect the measured transmitted or reflected signal by absorption and scattering of light at 632.8 nm wavelength. Attenuation of light in tissue is described according to light transport theory by the effective attenuation coefficient. An exact solution of the light transport equation in turbid media can be modified by following the path each individual photon and calculating the probability of scattering or absorption in a series of steps, using the Monte Carlo simulation [2,10,13,19]. In the study of rheology of blood, the electrical conductivity of blood is very paramount.
The effect of low level Laser interaction or radiation on tissue becomes a matter of fact when implementing around 650 nm wavelength of diode laser on human skin [16,20]. The laser tissue interaction enables us to obtain the optical characteristics of biological tissue and the changes that occur in the optical and electrical parameters of human blood. In this paper, He-Ne laser diode with 5 mW output power, 650 nm wavelength and 5 mm diameter of beam was used. This type of Laser diode was chosen because it has a power density of 5 mW and beam of 5 mm and has a small angular divergence and high specific power density which are able to restrict the intensity of small volume of blood under experiment.
The major reason for choosing this type of diode laser and its wavelength is that it radiate red and near infrared light spectrum on the human skin. With this fact that hemoglobin cannot be absorbed in the region and laser light can be able to penetrate deep into the living tissue. The Laser radiation of blood vessel causes immediate vasodalition of the skin [16].
Results and Discussions
Design constraints
As per any design of biomedical devices with the patient-electrical interface, the primary goal of the design is safety. Electricity is being applied across the finger which introduce a small threat of the subject, however we did our best to use a very low current (9v) of electricity here so that there will not be any direct threat of current exposure to the subject’s heart. We ensured that the electrical circuit going to and from the subject was electrically isolated from other circuit. In spite of all these factors taken into consideration the prototype design (Non-invasive measurement of blood glucose level) remains unproven technology.
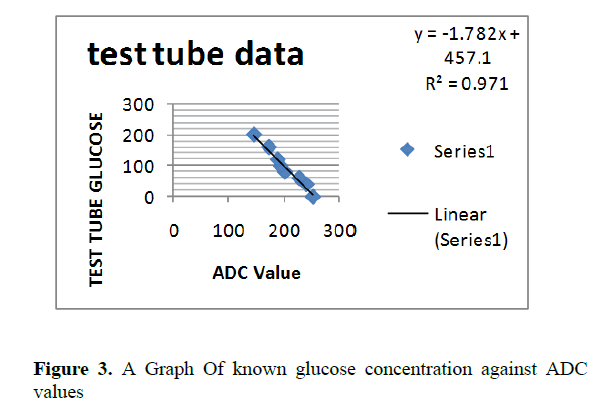
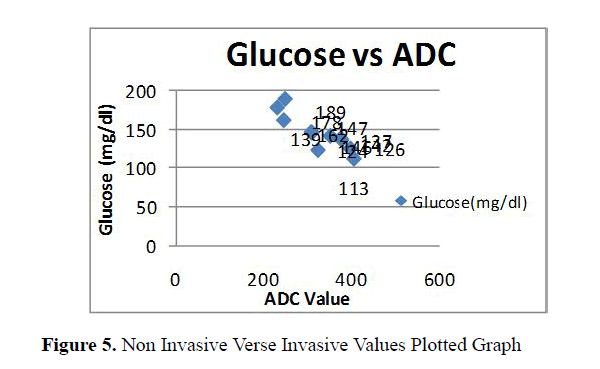
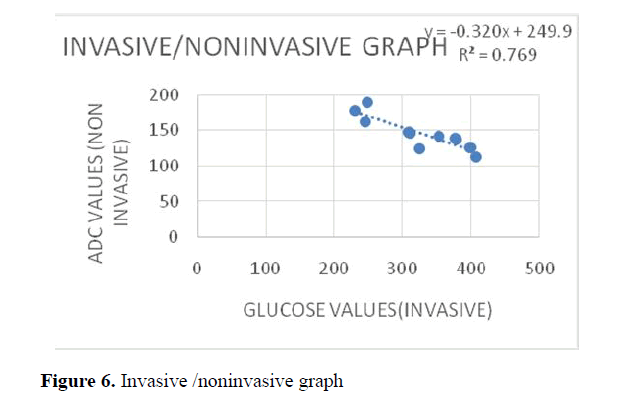
The physiological and pathological conditions changes from one person to another. The exact placement of the test-tube containing known glucose solution was very difficult to attain, precise calibration was very challenging, No standard format to compare and optimized the signal intensity obtained, financial constraint and finally Time Constraint (Figures 5 and 6).
However this paper presents a method for estimation of blood glucose level for diabetic and non-diabetic patients using finger phethysmograph principle. The He-Ne laser operating at 650 nm wavelength was used. Considering the results obtained by the biochemistry test, it can be stated that blood flow is indirectly proportional to the blood glucose level (Tables1 and 2).
Non Invasive Blood Glucose Level Monitor |
||
|---|---|---|
| Si.No | Test Tube Glucose(mg/dl) | ADC Value |
| 1 | 0 | 253 |
| 2 | 40 | 241 |
| 3 | 60 | 228 |
| 4 | 80 | 202 |
| 5 | 100 | 194 |
| 6 | 120 | 189 |
| 7 | 160 | 173 |
| 8 | 200 | 146 |
Table 1.Results- Known Glucose concentration in test tube.
| Si.No | Patient ID | Age/Sex | ADC Value | Glucose(mg/dl) | Signal Intensity(mv) |
|---|---|---|---|---|---|
| 1 | 2701 | 48/M | 310 | 146 | 1.51 |
| 2 | 2702 | 62/M | 246 | 139 | 1.2 |
| 3 | 2703 | 33/F | 376 | 139 | 1.83 |
| 4 | 2704 | 19/M | 324 | 124 | 1.58 |
| 5 | 2705 | 54/M | 352 | 142 | 1.71 |
| 6 | 2706 | 37/M | 378 | 137 | 1.84 |
| 7 | 2707 | 41/F | 249 | 189 | 1.21 |
| 8 | 2708 | 10/F | 406 | 113 | 1.98 |
| 9 | 2709 | 42/M | 309 | 147 | 1.5 |
| 10 | 2710 | 29/M | 398 | 126 | 1.94 |
| 11 | 2711 | 46/F | 231 | 178 | 1.12 |
Table 2. Non-Invasive Signal Intensity Obtained In ADC Values From Diabetic Patients
The prototype of the device was designed to provide a better correlation of the blood glucose and the biochemistry test as well as the ADC values obtains depicted promising and reliable results. The method used to measure and estimate blood glucose from the subject’s finger should be comfortable, bloodless and painless.
The device was calibrated using the signal intensity of glucose noninvasively verse the biochemistry test values to plot the best fitting curve. The device must be portable and inexpensive due to the use of diode laser. The use of diode laser should yield out a more promising, accurate and precise results. The device should be accepted for clinical usage [21-25] (Tables 3 and 4).
| Non Invasive Blood Glucose Level Monitor | |
|---|---|
| ADC Value | Glucose(mg/dl) |
| 310 | 146 |
| 246 | 162 |
| 376 | 139 |
| 324 | 124 |
| 352 | 142 |
| 378 | 137 |
| 249 | 189 |
| 406 | 113 |
| 309 | 147 |
| 398 | 126 |
| 231 | 178 |
Table 3. Non Invasive Verse Invasive Values Plotted To Obtain Regression Equation
| Si.No | Patient ID | Age/Sex | ADC Value | Glucose(mg/dl) | Estimated Glucose Values |
|---|---|---|---|---|---|
| 1 | 2812 | 53/F | 215 | 193 | 181.075 |
| 2 | 2813 | 27/M | 387 | 387 | 125.983 |
| 3 | 2814 | 14/M | 398 | 124 | 122.46 |
| 4 | 2815 | 69/M | 202 | 207 | 185.239 |
| 5 | 2816 | 57/M | 238 | 183 | 173.708 |
| 6 | 2817 | 35/F | 367 | 132 | 132.389 |
| 7 | 2818 | 29/F | 392 | 129 | 124.382 |
| 8 | 2819 | 44/F | 308 | 153 | 151.287 |
| 9 | 2820 | 32/M | 359 | 147 | 134.952 |
| 10 | 2821 | 48/M | 279 | 169 | 160.576 |
| 11 | 2822 | 19/M | 409 | 118 | 118.937 |
| 12 | 2823 | 12/F | 399 | 123 | 122.14 |
| 13 | 2824 | 58/M | 238 | 179 | 173.708 |
| 14 | 2825 | 31/F | 341 | 128 | 140.717 |
| 15 | 2826 | 63/M | 250 | 165 | 169.865 |
| 16 | 2827 | 22/M | 394 | 126 | 123.741 |
| 17 | 2828 | 49/M | 221 | 193 | 179.153 |
| 18 | 2829 | 38/M | 314 | 139 | 149.365 |
| 19 | 2830 | 51/M | 205 | 210 | 184.278 |
Table 4.The estimated values of noninvasive glucose obtained using the regression equation to solve for “Y”
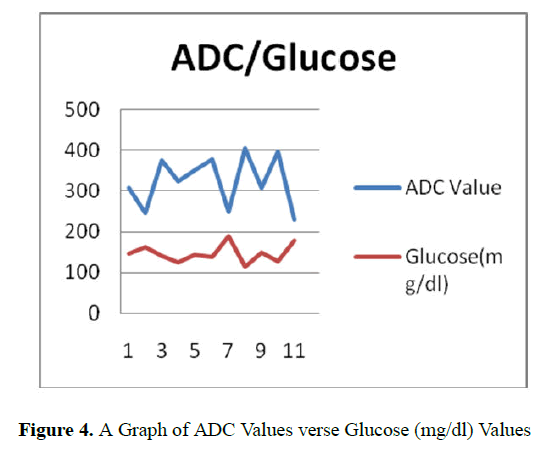
From the above graph the ADC value verses Glucose; it is evident that ADC value provides promising result than the glucose.
The regression equation obtained after the plotting the linear graph:
Y=-0.3203X+249.94
R2= 0.7695
Conclusion and Future Work
Management of diabetes mellitus is mainly based on continuous monitoring of blood glucose level of which the existing method to monitor the blood glucose level require the patient preparation (making sure you have more lancets and test strips always), piercing the skin, pricking the vein and skilled technicians. The results presented here indicate the ability of noninvasive technique to measure the resistivity of blood flow based on finger photoplethysmography to help correlate the blood glucose concentration in a diabetic patient. We demonstrated a known glucose concentration in glucose solution and the regression equation obtained was quite promising. The kit was examined on patient’s finger and the signal intensity obtained in ADC values was correlated and estimated.
The use of laser diode is remains still an unproven method to some extent in predicting and estimation of blood glucose concentration. The calibrations of the prototype were done by comparing the signal intensity obtained in ADC with the biochemistry testing method called GOD and POD method. About 30 fasting blood glucose were measured and estimated as well. However, the estimated calibration first was not correlating with the convention glucose values. The calibration was done by programing the output of the microcontroller and the glucose concentration was shown in percentage form. The clinical trials were done and the results obtained were used to validate the device. In the validation lot of challenges were proven unsolved due to time factor and technical known how in comparing with the accuracy with current glucometer on market. Despite the encouraging preliminary results, more measurements are required to further test the system and estimate the sensitive and accuracy. Moreover, further development of the theoretical model that correlates the measured optical signal is required.
The proposed kit has the potential to lead to a better noninvasive blood glucose measurement in the near future as more scholars are diving into such area of research. Hence, there is a continuing need for improved low-cost noninvasive analytical instruments and methods that would provide essentially the same accuracy as conventional invasive blood glucose test. This method and design would fulfill the need for a durable, cost-effective, and environmentally friendly and more over non-disposable kit for measuring blood glucose.
References
- Rodger W. Non-insulin-dependent (type II) diabetes mellitus. CMAJ. 1991; 145: 1571-1581.
- Ashok V, Nirmalkumar A, Jeyashanthi N. A Novel Method for Blood Glucose Measurement by Noninvasive Technique Using Laser. World Academy of Science, Engineering and Technology. 2011.
- Kanno Y, Sakai A, Miyashita M, Tsuchida K, Matsuo O. Plasminogen deficiency is associated with improved glucose tolerance, and lower DPP-4 activity. Diabetes Res Clin Pract. 2016; 120:190-3
- Sairam K, Renumadhavi CH. A Review on Non-Invasive Blood GlucometerBased on Photoacoustic Method. Int J Inn Resear Sci Tech. 2015; 1: 9.
- Zeller W, Naehle L, Fuchs P, Gerschuetz F, Hildebrandt L, Koeth J. DFB Lasers Between 760 nm and 16 µm for Sensing Applications , Sensors (Basel). 2010; 10: 2492-510.
- Zuomin Zhao. Pulsed PhotoacousticTechniques and GlucoseDetermination in HumanBlood and Tissue” Academic Dissertation to be presented with the assent of the Faculty of Technology. University of Oulu, for public discussion in the Auditorium TS 101, Linnanmaa, 2002.
- Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med. 1997; 5: S1-85.
- AkeshGovada, Renumadhavi CH, K B Ramesh KB. Non-Invasive Blood Glucose Measurement. Int J Advanced Resear in Comput Commun Eng. 2014; 3: 1.
- Pavithra AG, Karan DM, Kumar DA, Anu Shalin PS. Non-invasive technique to measure glucose and haemoglobin level in blood using nir-occlusion spectroscopy. IJSRM. 2014; 2: 756-762.
- Chi-Fuk So, Kup-Sze Choi, Thomas KS Wong, Joanne Chung WY. Recent advances in noninvasive glucose monitoring. Medical Devices: Evidence and research. 2012; 45–52.
- Wilson B. Measurement of tissue optical properties: methods and theories. In: Welch AJ, Van Gemert MCC, eds. Optical thermal response of laser-irradiated tissue. New York: Plenum Press, 1995.
- Srivastava A, Md Koushik Chowdhury, Sharma S, Sharma N. Blood Glucose Monitoring Using Non Invasive Optical Method: Design Limitations and Challenges. International Journal of Advanced Research in Electrical, Electronics and Instrumentation Engineering. 2013; 2: 1.
- Miyauchi Y, Horiguchi T, Ishizawa H, Shin-ichirou T, Hara H. Blood Glucose Level Measurement by Confocal Reflection Photodetection System. SICE Annual Conference 2011, Waseda University, Tokyo, Japan, 2011.
- Bachem A, Reed CI. The penetration of light through human skin. American Journal of Physiology. 1931; 97:86-91.
- Songlin Yu, Dachao Li. In vitro glucose measurement using tunable mid-infrared laser spectroscopy combined with fiber-optic sensor”, Biomedical optics express. 2014; 5: 1.
- Pospiech M, Liu S. Laser Diodes an introduction. University of Hannover, Germany, 2004.
- Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med 1997; 5: S1-85.
- Bashkatov AN, Genina EA, Tuchin VV, Optical Properties of Skin, Subcutaneous, And Muscle Tissues: A Review. J Inn Opt Healt Sc. 2011; 4: 1.
- Hammel HT, Hardy JD, Murgatroyd D. Spectral transmittance and reflectance of excised human skin. J Appl Physiol. 1956; 9: 257-264.
- Webster JG. Finger Plethysmograph to measure blood resistivity. 2008.
- Longini RL, R.Zdrojkowski. A note on the theory of backscattering of light by living tissue. IEEE Trans. Bio-Med Eng, 1968; 15: 4-10.
- Rothman S, Physiology and Biochemistry of the Skin. Chicago, IL: University of Chicago Press. 1954.
- Groenhuis RAJ, Ten Bosch JJ, Ferwerda HA. Scattering and absorption of turbid materials from reflection measurement. 1. Theory. Appl Opt. 1983; 22: 2456-62.
- Kohl M, Essenpreis M, Cope M. The influence of glucose concentration upon the transport of light in tissue-simulating phantoms. Phys Med Biol. 1995; 40: 1267-1287.