Research Article - Current Pediatric Research (2017) Volume 21, Issue 4
Noise in a university operating theatre during the course of pediatric surgical procedures.
Dheidan Alshammari, Samah Osailan, Marina Sica*, Vu Hong Tuan, Pierre Kuhn, Claire Zores, Isabelle Talon, Anne Schneider, Francois BecmeurDivision of Pediatric Surgery, Department of Medical Science, Surgery and Neuroscience, University of Siena, Italy.
- *Corresponding Author:
- Marina Sica
Division of Pediatric Surgery
Department of Medical Science
Surgery and Neuroscience
University of Siena, Italy.
Tel: 0577/586501
E-mail: sicamarina121@gmail.com
Accepted date: September 27, 2017
Abstract
Objective: To measure the level of noise in our university operating room and to identify different phases during the course of surgical procedures in which noise level exceeding 40 decibels (National Recommendation). Method: This was a prospective randomized single blinded study for a period of 5 months starting from January 2016. A sonometer was placed randomly in the different operating theatres. Its presence did not mean that it should work. Recording started from the patient’s entry to the operating theatre and ended upon his/her exit. We divided our period in three different types: P1 (from the entry of the patient until the start of surgical procedure); P2 (from the surgical incision to the end of the procedure); P3 (from the completion of closure till the exit from the OR). Strict inclusion criteria (general pediatric surgery case, elective surgery, during normal working hours, operations performed by board certified surgeons) and exclusion criteria (non-general pediatric surgery cases, emergency case, after hours, resident performing the procedure as first surgeon) were applied. Results: The sonometer was present in a total of 64 operations. It was recording in 26 operations. The surgical procedures were: 54% open surgery, 34% laparoscopic surgery and 12% were endoscopic procedures. The total recorded time was 2419 minutes, around 40.4 hours. The average P1 time was 25’, P2 65’ and P3 7’. T test was performed and found the average to be significantly P value <0.0001 from the 40 dBA recommended limit. LEQ noise level was 56.48 dBA during P1, 53.14 dBA during P2 and 55.50 dBA during P3. We registered 813 incidents or sudden noise peaks >70 dBA during P1, 912 incidents during P2 and 293 incidents during P3. Most often the incidents were due to conversations within the staff at the level >75 dBA. Only 1.5% incidents were more than 80 dBA. More rarely we registered sounds of bells from cellular phones sometimes more than 90 dBA. Conclusion: It is as if there is a first period with excited staff before the beginning of surgery. Then, a second period follows, where the staff is quitter due to required concentration: it looks like the major period of the surgical procedure. The third period, at the end of the surgical act, looks like a moment of relaxation with a noisy ambiance. By this point of view, noisy distractions, considered to be a main cause of perioperative incidents, appear to be related to the level of staff seriousness.
Keywords
Noise in the operating room, Sonometer, Noise level, Pediatric surgery.
Introduction
Noise level in the operating room has been associated with lower performance of surgeon and staff [1]. Sudden noise peaks during surgery, may be considered as undesirable events or distractions that could impair surgical and team performance [2-4]. Noise in the operating rooms is mostly due to air conditioning systems, modern equipment with positive alarms when they work and negative alarms when something becomes wrong. Monitoring of the patient is noisy but essential and often limited to the patient’s pulse. Conversations within the staff may be useful as for checklist formulation. Irrelevant conversations or conversations with people out of the staff are associated with lower team performance due to distraction [5]. But many students (future nurses, anesthesiologists, surgeons, medical doctors) are present in a university operating theatre. Formerly, due to ancient pedagogical concepts, these students only had to see what happened. They could stay behind a window pane. But learning-by-doing requires the physical presence of these students in the operating room.
We wanted:
- To measure the level of noise in our university operating room in order to reduce it, if necessary. We aimed to assess our compliance with the national recommendation of not exceeding 40 decibels (dBA) in the operating theatres.
- To identify different phases during the course of surgical procedures in order to secure each period.
Methods
We planned a prospective randomized single blinded study for a period of 5 months starting from January 2016. All personnel working in the pediatric surgical unit were informed that a sonometer is to be placed randomly in the different operating theatres. Its presence does not mean that it will be recording and this was made very clear to all the surgical staff. The choice of theatre and the day to place the sonometer were also randomized. When placed in theatres, the sonometer was always placed centrally at a level of surgeon’s ears on a nonmoving object. Recording an operation was also randomized and the staff was not aware of it. Recording started from the patient’s entry to the operating theatre and ended upon his/her exit.
The surgical course was divided into three periods:
- P1, period 1, from the entry of the patient, installation, induction of anesthesia, preparation of the surgical field, till start of the surgical act,
- P2, period 2, from the incision till the completion of closure and dressing application.
- P3, period 3, from the completion of closure and dressing application till the exit of the patient.
Moreover, patient’s demographics, kind of surgery, the equipment used, the number of people present, amongst many other details were recorded.
Strict inclusion criteria (general pediatric surgery case, elective surgery, during normal working hours, operations performed by board certified surgeons) and exclusion criteria (non-general pediatric surgery cases, emergency case, after hours, resident performing the procedure as first surgeon) were applied.
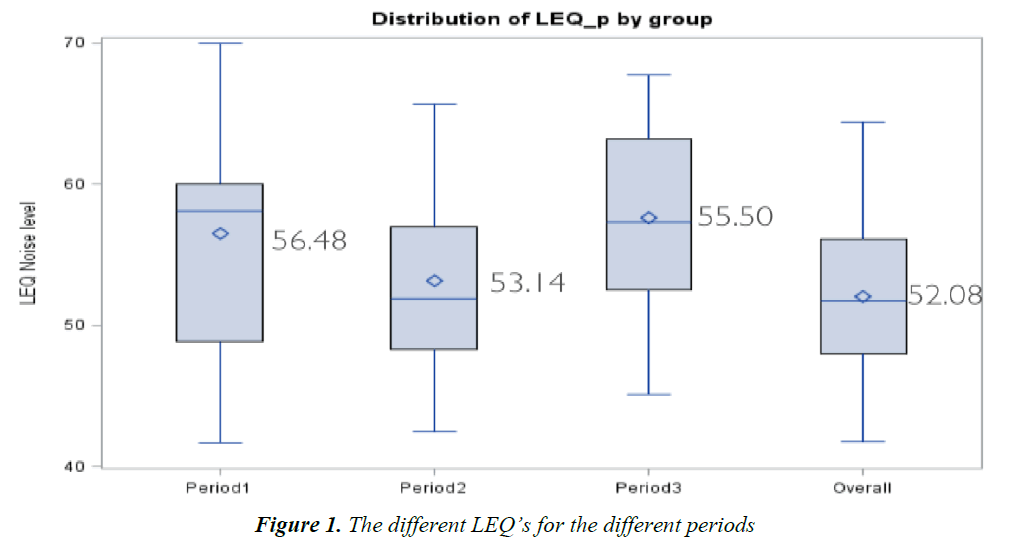
We used the equivalent continuous noise level (Leq level) for the assessment of noise dose or sound exposure in the workplace. Leq level is used by most countries as the metric of choice for measuring the exposure of workers to noise, as there is no time constant and it correlates reasonably well to the effect of hearing damage risk (Figures 1 and 2).
Results
As we are in a university hospital, our operating theatres are usually busy with a high presence of both students and observers. The usual surgical team is made up of 6 members (surgeon, assistant, anesthetist, anesthetic nurse, scrub nurse and theatre nurse) however our average recorded presence is of 10 individuals in the three mentioned periods (range 9-16).
In total the sonometer was present in a total of 64 operations where 26 operations from the 64 the sonometer was recorded. The total recorded time was 2419 min around 40.4 h. The average operating time was 97 minutes with a range of 23-304 min). The average P1 time was 25’, P2 65’ and P3 7’.
When the sonometer was recorded, 54% of the operations were open surgery while 34% were laparoscopic surgery and 12% were endoscopic procedures.
Regarding our first objective we found that our average LEQ level was 52.08 dBA with a standard deviation of 5.89. T test was performed and found the average to be significantly P value <0.0001 from the 40 dBA recommended limit. LEQ Noise level was 56.48 dBA during period 1, 53.14 dBA during period 2 and 55.50 dBA during period 3.
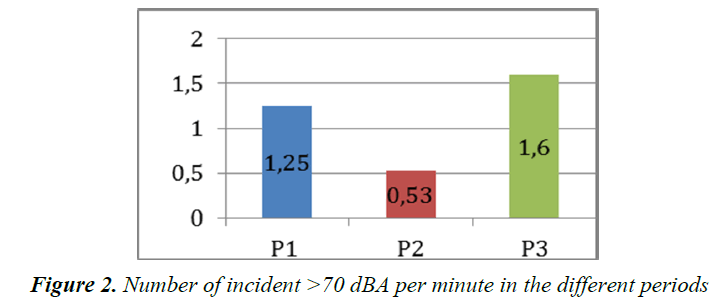
We registered 813 incidents or sudden noise peaks >70 dBA during P1, 912 incidents during P2 and 293 incidents during P3. We reached an average of 31 incidents for the period P1, 35 for P2 and 11.26 for P3. That is to say, 1.25 incidents/min during the period P1, 0.53 incidents/ min during the period P2 and 1.6 incidents/min during the period P3.
Most often the incidents were due to conversations within the staff at the level >75 dBA. Only 1.5% incidents were more than 80 dBA. More rarely we registered sounds of bells from cellular phones sometimes more than 90 dBA.
Within our study the different surgical teams involved did use one of or a combination of the following: monopolar diathermy, bipolar diathermy, suction. A multivariable linear regression of average noise levels with the different instruments did not show any significant relationship.
Discussion
Noise is defined as unwanted sound, therefore its recognition and assessment is highly subjective and user dependent [6]. In an operating theatre noise can originate from human-human interaction, human-machine interaction, or machine itself. Conversation amongst staff or staff related activity can produce noise levels as high as 78 dBA, whereas equipment related noise can go up to 120 dBA [1,7]. Conversation amongst staff, as reported in one study, especially if medically irrelevant, can be a very potent cause of distraction [8]. The modern operating theatre is well equipped, and patients are very well monitored. Given this outstanding surveillance, many alarms and sounds go off during an intervention. A team, that studied the frequency of alarms and their therapeutic significance during cardiac surgery, reported that 80% of the alarms sounded during their study had no therapeutic consequences [9].
Moreover, it has been shown that noise exposure increases the risk of developing noise induced hearing loss amongst 50% of theatre staff [10]. This occupational risk can be further explained by the fact that repeated loud noise exposure can shift the sensory neural threshold permanently hence potentially causing deafness [11]. A study reported that both theatre staff and patients are exposed to noise level above the recommended daily safe limits (80 and 85 dBA) [10]. The stapedius muscle which normally attenuates loud sounds is likely to be paralyzed by anesthetic products hence posing an additional concern for patients [10].
Surgery is a complex task that demands both high levels of concentration and fine motor skills in order to be able to coordinate hand movement and perform with high level of precision. Given the complexity of surgery, and the need to be able to process high degree of information, surgical performance is highly susceptible to the adverse effect of noise [1]. Not only surgeons can be affected, in one study 84% of anesthetists reported a negative effect on their performance because of noise levels in the operating theatre [12]. Moreover, to further aggravate, it is a known fact that the operating theatre is full of distractions [13]. We hypothesize that such distractions and noise levels would be greater in a university teaching hospital if no measure is applied to control them [2]. Noise decreases concentration and distracting noise decreases dexterity in simulated video surgery [2].
Noise level can vary during the procedure and can vary amongst the different types of operations; some interventions are particularly noisy [1]. Given the previous, due to high capacity air condition systems, operating theatres are also considered noisy when unoccupied [1]. A study reported that up to 52% patients undergoing elective surgery found it noisy during induction and 16% of the patients felt that the noise was distressing [14].
The effects of noise have over performance depended on a number of factors [6]:
Level of noise, Type of noise, predictable, controllable, level of stress tolerance of the individual, complexity of task being performed.
Continuous or periodic noises are considered to be predictable whereas discontinuous or episodic are nonpredictable noises [6]. Moreover controllable noises are those noises by which we can terminate at will [6]. It has been documented that noises when unpredictable or uncontrollable or both, even of lesser amplitude, can interfere substantially on complex tasks whereas high level continuous noise does not have significant effects of simple motor or mental tasks [6]. Moreover, an unpredicted sudden impact of noise that is at least 30dBA above the background noise level can cause what is known as a “startle response” [6]. The startle reaction will subsequently cause a stress reaction which is better described physiologically by increased adrenaline secretion, pupil dilation, elevation of blood pressure which can have a serious important effects especially when the task in hand requires vigilance and concentration [6]. Moreover, conversation amongst staff has been shown to interfere with performance much more than other noises that do not appear to be conversational [6]. As mentioned in the introduction, we perceive that the impairment of communication, especially in emergency situations, is the worst consequence of noise. Reliable communication can be lost when a number of distinct auditory signals present at the same time, as it will be difficult for the human ear to discriminate or distinguish between them, a phenomenon known as masking [6]. Communication is of utmost importance amongst medical staff in order to achieve patient safety. Failure of communication during surgery has been identified to be one of the leading causes of error and poor patient outcomes [1].
As we did, Sevdalis et al. [15] and Messina et al. [16] (anesthesiologists and surgeons) distinguished 3 different phases during surgery, a preoperative phase with the arrival of the patient into the operating room and induction of anesthesia, an intraoperative phase from skin incision to skin closure and a postoperative phase with anesthesia reversal and displacement of the patient to the recovery room. Communication tasks are more frequent during the preoperative phase and the postoperative phase. If the atmosphere of the operating room is too noisy during these periods, it may become a problematic disturbance to required communication tasks. We noticed a high frequency of sudden noise peaks during these periods as if staff concentration, was not enough to make a calm labor atmosphere and was not sufficiently focused on patient care.
Based on our results we found interestingly, that 95% of our recordings in order to identify the nature of high noise incidents were chatter and irrelevant conversations amongst the staff. This chatter was in 48% of the time not medically relevant. In the other 52%, during the second period, it was very simple demands like “please hold the camera well”, “open the trocars to let some gas out”, “suction here”, “did the patient receive any antibiotics”, “I just called the radiographer”. The 53.14 dBA LEQ noise level during this second period seemed to be well tolerated. It is likely due to the fact that we got accustomed to work in such a busy environment, and work well in it.
In addition, chatter amongst staff was very high: 95% of sound events recorded above 70 dBA were chatter amongst the staff.
Furthermore, we know that we work in loud environments and this has been the case for many years now. We wonder if working in such an environment for a long time had made us become very accustomed to work noisy theatres. We adapted by speaking louder, developing higher noise tolerance, compensate automatically in our communication by speaker in a loud voice even if we talked to a person next to us and not allow our concentration to be affected. Nevertheless, according to Sevdalis et al. [15], “more intraoperative distracting communications are associated with deterioration of patient safety checks”.
A question remains: why do we record a high frequency of incidents with sudden noise peaks during the first and the third period? It is as if there is a first period with excited staff before surgery. Then, a second period follows, more quiet due to required concentration: it looks like the major period of the surgical procedure. The third period, at the end of the surgical act, looks like a moment of relaxation with a noisy ambiance. By this point of view, noisy distractions appear to be related to the staff seriousness. “More distractions of the team are linked to fewer safety checks being carried out by them” [15]. Thus, a noisy atmosphere may be a good marker of attention and capacity of concentration for the staff. By this way the team seems to forget the importance of the installation, the necessity of calm atmosphere for the patient during the induction of anesthesia and the communication talks during the checklist for the first period. Ending safety a surgical procedure is also an essential moment for the patient.
Our results are significantly different from those described by Antoniadis [4]. Procedure length was divided into quartiles respectively. In this study, intraoperative interruptions were observed more frequently during the first period and were less and less frequent along the surgical procedure. Different behavior may be observed depending of the team and its habits.
We did not find a significant relation between the uses of all the surgical equipment and measured noise levels. The use of some equipment was not shown any significant association with value to noise levels.
Given the previous statement, when we analyzed the sources of high noise level associated events, alarms from the usage of this equipment or the noise of the suction did elevate the noise level more than at least 15 dBA. We also identified other sources of noise in addition to chatter amongst staff, which was the main one, to be:
1- Mobiles ringing
2- Material falling
3- Alarms (Anesthetics, equipment related)
4- Trolleys being pushed around
5- Patients bed being pushed into or out of the operating theatre
Conclusion
The operating theatre should be a safe environment for the patient and medical personnel during the whole procedure. In order to achieve such a goal, strict guidelines should be applied and performance regularly audited. As proposed by previous work, we need to create a culture of safety by reducing noise levels in the operating room. The sound can be reduced by 50% by specific measures as demonstrated by research team. Noise even if tolerated can still harm the ears of both patients and staff therefore as we offer eye protection during an operation.
References
- Katz J. Noise in the operating room. Anesthesiology 2014; 121: 894-898.
- Engelmann C, Neis JP, Kirschbaum C, et al. A noise-reduction program in a pediatric operation theatre is associated with surgeon’s benefits and a reduced rate of complications: A prospective controlled clinical trial. Ann Surg 2014; 259: 1025-1033.
- Healey AN, Sevdalis N, Vincent CA. Measuring intra-operative interference from distraction and interruption in the operating theatre. Ergonomics 2006; 15: 589-604.
- Antoniadis S, Passauer-Baierl S, Baschnegger H, et al. Identification and interference of intraoperative distractions and interruptions in operating rooms. J Surg Research 2014; 188: 21-29.
- Wheelock A, Suliman A, Wharton R, et al. The impact of operating room distractions on stress, workload and teamwork. Ann Surg 2015; 261: 1079-1084.
- Thompson JHB. Noise pollution in the operating theatre. Lancet 1990; 335: 891-894.
- Shankar N, Malhotra KL, Ahuja S, et al. Noise pollution: A study of noise levels in the operation theatres of a general hospital during various surgical procedures. J Indian Med Assoc 2001; 99: 246-247
- Persoon MC, Broos HJHP. The effect of distractions in the operating room during endourological procedures. Surg Endosc 2011; 25: 437-443.
- Schmid F, Goepfert MS, Kuhnt D, et al. The wolf is crying in the operating room: Patient monitor and anesthesia workstation alarming patterns during cardiac surgery. Anesth Analg 2011; 112: 78-83.
- Siverdeen Z, Ali A, Lakdawala AS, McKay C. Exposure to noise in orthopaedic theatres - Do we need protection? Int J Clin Pract 2008; 62: 1720-1722.
- Ullah R, Bailie N, Crowther S, et al. Noise exposure in orthopaedic practice: Potential health risk. J Laryngol Otol 2004; 118: 413-416.
- Tsiou C, Efthymiatos G, Katostaras T. Noise in the operating rooms of Greek hospitals. J Acoust Soc Am 2008; 123: 757-765.
- Mentis HM, Chellali A, Manser K, et al. A systematic review of the effect of distraction on surgeon performance: Directions for operating room policy and surgical training. Surg Endosc 2016; 30: 1713-1724.
- Liu EH, Tan S. Patients’ perception of sound levels in the surgical suite. J Clin Anesth 2000; 12: 298-302.
- Sevdalis N, Undre S, McDermott J, et al. Impact of intraoperative distractions on patient safety: a prospective descriptive study using validated instruments. World J Surg 2014; 38: 751-758.
- Messina M, Molinaro F. Preoperative distraction in children: hand-held videogames vs. clown therapy. Pediatr Med Chir 2014; 36: 6.
- Hogan LJ, Harvey RL. Creating a culture of safety by reducing noise levels in the OR. AORN J 2015; 102: 410.