Case Report - Journal of Medical Oncology and Therapeutics (2017) Volume 2, Issue 2
New adnexal masses in a patient with a history of chronic myelogenous leukemia: a case report
Therese E Gadomski1, Katherine Rogg1, Laura Kidd2, William R Robinson3*
1School of Medicine, Tulane University, USA
2Department of Pathology and Laboratory Medicine, Tulane University, USA
3Tulane Cancer Center, USA
- *Corresponding Author:
- William R Robinson
Section Chief
Gynecologic Oncology
Tulane Cancer Center
1430 Tulane Avenue
SL-68 New Orleans
LA 70112
USA
E-mail: wrobinso@tulane.edu
Accepted date: May 08, 2017
Citation: Gadomski TE, Rogg K, Kidd L, et al. New adnexal masses in a patient with a history of chronic myelogenous leukemia: a case report. J Med Oncl Ther. 2017;2(1):24-26.
DOI: 10.35841/medical-oncology.2.2.24-26
Visit for more related articles at Journal of Medical Oncology and TherapeuticsAbstract
Chronic myelogenous leukemia (CML) is a myeloproliferative neoplasm characterized by abnormal hyperplasia of granulocytes. Though not one of the common signs and symptoms, extramedullary hematopoiesis (EMH) can be associated with CML. Here we report a rare case of extramedullary hematopoietic infiltration of the ovaries in a patient with known CML who presented with rapidly developing adnexal masses.
Keywords
Adnexal mass, Chronic myelogenous leukemia, Extramedullary hematopoiesis.
Introduction
Chronic myelogenous leukemia (CML) is a myeloproliferative neoplasm characterized by abnormal hyperplasia of granulocytes, which in most cases is secondary to the reciprocal translocation of chromosomes 9 and 22 and the consequent function of the BCR/ABL fusion gene [1]. CML is a disease of the bone marrow with semi-sequential phases delineated the chronic phase, accelerated phase and blast phase. Most patients present in the chronic phase [2]. Regularly observed signs and symptoms of the chronic phase include anemia, splenomegaly, fatigue, weight loss, malaise, and left upper quadrant fullness or pain [3]. Transition to the accelerated phase may be subtle or may be characterized by worsening anemia, splenomegaly and organ infiltration by hematopoietic elements. CML blast phase presents as an acute leukemia [3].
Extramedullary hematopoiesis (EMH) is the proliferation of myeloid, erythroid, and megakaryocytic cells in non-bone marrow sites [4]. EMH has been associated with CML, with the lymph node as the most commonly involved site for the extramedullary disease [5]. EMH has been documented throughout the abdomen (liver, spleen) and thorax (bone, mediastinum) but rarely in the gynecological tract [6-8]. Here we report a rare case of extramedullary hematopoietic infiltration of the ovaries in a patient with known CML who presented with rapidly developing adnexal masses.
Case Presentation
A 31 year old African-American female with a personal history of CML diagnosed at age 17 presented to the Emergency Department (ED) with two days of severe, progressive epigastric abdominal pain, radiating to her back. She also complained of nausea, vomiting and fatigue. Physical exam was significant for moderate abdominal distension and minimal tenderness. Complete blood count (CBC) showed a white blood cell count of 49.6 thousand/ml, hemoglobin of 6.4 g/dL and platelet count of 96,000. The patient was transfused four units of packed red blood cells to reach hemoglobin of 10.3 g/dL and discharged from the ED with instructions to follow up in the Hematology/Oncology clinic.
She returned to the ED two days later complaining of severe back pain. Notable findings included continued abdominal distension but with minimal tenderness. CBC was significant for hemoglobin of 5.4 g/dL. Computerized tomography (CT) scan of abdomen and pelvis was performed, which showed a large amount of hyper dense, free fluid in the abdomen concerning for hemoperitoneum of unknown etiology, as well as evidence of a 6.5 × 5.9 cm heterogenous mass in the left pelvis and a 4.5 × 2.7 cm heterogenous mass in the right pelvis, including a right ovarian cyst measuring 2.0 × 1.4 cm. Abdominal and trans-vaginal ultrasonography demonstrated positive arterial flow to both masses, which confirmed the CT findings and suggested ovarian etiology.
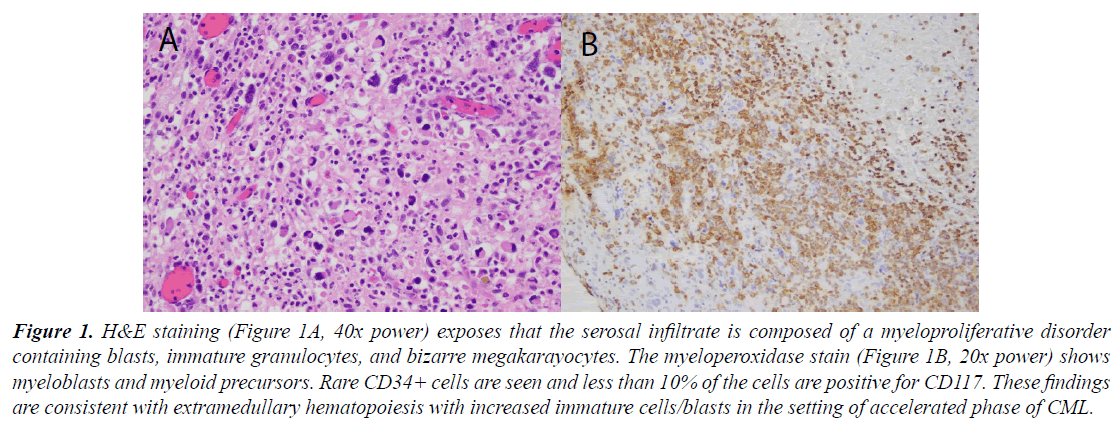
Gynecologic oncology was consulted for these findings, and subsequently recommended laparoscopic bilateral salpingo-oophorectomy and evacuation of ascitic fluid. Before surgery could be performed, the patient was hospitalized multiple times for symptomatic anemia and blood transfusions. It was eventually decided that surgery was the only remaining option that might stabilize the patient, and the procedure was therefore performed despite the presence of severe anemia. Both adnexa, including the masses seen on CT, were removed without complication. The left and right ovaries and serosal lymphovascular spaces were found to contain serosal myeloproliferative disease, as indicated by the presence of blasts, immature granulocytes and bizarre immature megakaryocytic precursors (Figure 1A).
Figure 1. H&E staining (Figure 1A, 40x power) exposes that the serosal infiltrate is composed of a myeloproliferative disorder containing blasts, immature granulocytes, and bizarre megakarayocytes. The myeloperoxidase stain (Figure 1B, 20x power) shows myeloblasts and myeloid precursors. Rare CD34+ cells are seen and less than 10% of the cells are positive for CD117. These findings are consistent with extramedullary hematopoiesis with increased immature cells/blasts in the setting of accelerated phase of CML.
Atypical mononuclear cells expressed myeloperoxidase, which suggested immature myeloid precursors. Multinucleated cells expressed CD61and were suggestive of immature megakaryoyctes. Cells expressing CD117 accounted for less than 10% of the cellular infiltrate in small to intermediate cell clusters, which suggested myeloid blasts or immature myeloid precursors. Rare CD34+ cells were identified, suggesting hematopoietic progenitor cells. Morphology and immunohistochemical stains, therefore, best supported extramedullary hematopoiesis with increased immature cells/blasts in a CML patient known to be in the accelerated phase of the disease (Figure 1B). These findings are suggestive of leukemic infiltration of the ovary manifesting as a solid tumor of blood forming elements.
Although the ascites (hemoperitoneum), anemia and thrombocytopenia were initially stabilized after surgery, the disease persisted and eventually progressed despite multiple chemotherapy regimens. The patient developed hemorrhagic pleural effusions, peritoneal hemorrhagic ascites and multiple blast crises. The spleen became massively enlarged due to invasive myelofibrosis and the patient was treated with palliative radiation therapy. Paracentesis was performed frequently, with aspiration of hemorrhagic peritoneal fluid. Ultimately, the patient contracted Prevotella oralis fungemia of the lungs and was referred for hospice care. She died approximately 3 weeks later.
Discussion
This case demonstrates that the differential diagnosis for women with CML who develop rapidly enlarging adnexal masses should include extramedullary hematopoietic infiltration of the ovaries. It is recommended that early operative intervention be considered to prevent recurrent drops in hemoglobin and/or platelets. Severe anemia may be an indication, rather than a contraindication, to surgery. The management of such patients, however, requires the efforts of and close cooperation between both the hematologistoncologist and gynecologist-oncologist.
Surgery, in the form of debulking, must be carefully timed with the appropriate replacement of blood factors to ensure optimal outcomes, particularly management of recurrent hemoperitoneum. Post-operative treatment should focus on relieving symptoms, including adequate pain management. If the disease progresses (which is likely in this advanced stage), ascites may recur, requiring serial paracentesis. This disease setting is a rare example of a hematopoetic malignancy that may require surgical in addition to medical management.
References
- Soni A, Paluri R, Deal T, et al. Extramedullary Involvement by chronic myelogeneous leukemia in five patients with unusual clinicopathologic features: A review of the effectiveness of tyrosine kinase inhibitors. J Clin Med Res. 2016;8(6):480-5.
- Mohd Ridzuan MS, Yap E, Wan Fariza WJ, et al. A case of chronic myeloid leukemia in blast transformation with leukemic ascites. Med J Malay. 2016;71(2):85-7.
- Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2016 update on diagnosis, therapy and monitoring. Am J Hematol. 2016;91:252-65.
- Sakakura M, Ohishi K, Nomura K, et al. Case of chronic-phase chronic myelogenous leukemia with an abdominal hematopoietic tumor of leukemic clone origin. Am J Hematol. 2004;77:167-70.
- Gao X, Li J, Wang L, et al. Bilineal extramedullary blast crisis as an initial presentation of chronic myeloid leukemia: A case report and literature review. Am J Case Rep. 2016;17:793-8.
- Palatnik A, Narayan R, Walters M. Extramedullary hematopoiesis involving uterus, fallopian tubes and ovaries, mimicking bilateral tuboovarian abscesses. Int J Gynecol Pathol. 2010;31:584-7.
- Rabischong B, Larrain D, Charpy C, et al. Extramedullary Hematopoiesis and myeloid metaplasia of the ovaries and tubes in a patient with myelofibrosis: Case report and concise review of the reported cases. J Clin Oncol. 2010;28:511-2.
- Sahu KK, Malhotra P, Uthamalingam P, et al. Chronic myeloid leukemia with extramedullary blast crisis: Two unusual sites with review of literature. Indian J Hematol Blood Transfus. 2016;32:89-95.