Research Article - Current Trends in Cardiology (2021) Volume 5, Issue 6
National Heart Institute registry for ST segment elevation myocardial infarction patients managed by primary PCI.
Ahmad M. Alkonaiesy*, Mohamed A. Elbordy, Abdel-Rahman G. Abdelaleem, Abdrabo A. Hassaan, Medhat M. Elsayed, Khaled M. El-Tohamy, Layla I. Shalaby, Osama M. Taha, Gamal M. Shaban
1Department of Cardiology, National Heart Institute, Cairo, Egypt
- Corresponding Author:
- Ahmad Mohammad Nooreldeen Alkonaiesy
Department of Cardiology,
National Heart Institute,
Cairo, Egypt
E-mail: ahmadalkonaissi@hotmail.com
Accepted date: 16 September, 2021
Citation: Alkonaiesy AM, Elbordy MA, Abdelaleem ARG, et al. National Heart Institute registry for ST segment elevation myocardial infarction patients managed by primary PCI. Curr Trend Cardiol. 2021; 5(6):74-81.
Abstract
Background: Little investigations addressed the results of STEMI patients managed by primary PCI in Egyptian population, especially in high volume tertiary cardiac hospital centers. The aim of the current study was to assess cardiovascular risk factors, angiographic and interventional characteristics, short term mortality and morbidity of STEMI patients undergoing PPCI presenting to our hospital.
Methods: We include all the patients admitted to our STEMI unite managed by primary PCI since November 2018 till 6 months afterwards (n=1354). We excluded patients presenting to ER with STEMI more than 48 hours, and patients with contraindication for primary PCI. We utilized angiographic characteristics, in-hospital mortality, and rates of procedural complications in all patients, being analyzed with appropriate statistical tests. Media of time to first medical contact in our ER and time to wire crossing of culprit artery were recorded and analyzed as well.
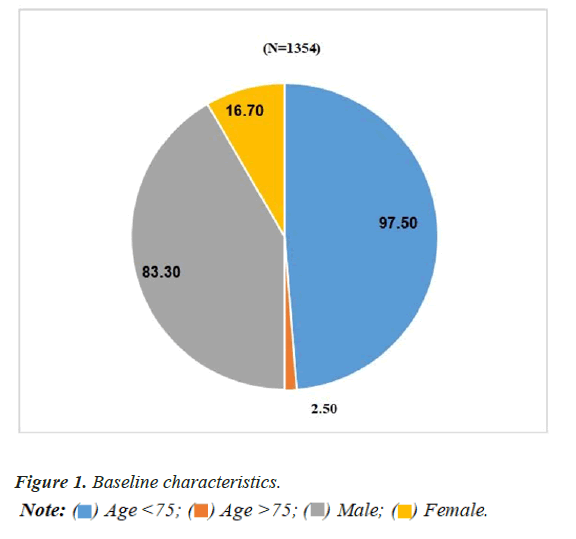
Results: Patients were young with a mean age of 54.45 and SD of 11.04, 97.5% were less than 75 years old while only 2.5% were more than 75 years old, 83.3% males and 16.7% females. The period elapsed from the onset of symptoms and the contact for medical help was longer for our patients: 120.0 (60.0; 240.0) minutes, and longer median time to wire crossing to culprit artery 95 (20.0; 170) minutes. The staff of ER was the first medical help (85% of patients). The admission mode was on the basis of individual presentation in 89% of patients. Anterior MI was found in 67.0% of cases presenting ECG. Reperfusion therapy was performed by PPCI to culprit artery in 90% of cases. In-hospital mortality was 3.9%.
Conclusion: Most of STEMI patients in our study were young males, current smokers, diabetics, showed higher prevalence of premature CAD, had significant time delays from the onset of symptoms to the contact for medical help, and more individual presenting rather than EMS presenting. Femoral access was the dominantly used access for PPCI. All stents used were drug eluting stents. Culprit only revascularization was the mainly used strategy, multi vessel disease staging intervention was done after hospital discharge. In-hospital mortality was comparable to other national registries.
Keywords
Acute coronary syndrome, Acute myocardial infarction, ST-Elevated Myocardial Infarction (STEMI), Primary percutaneous coronary intervention.
Introduction
Coronary Artery Disease (CAD) is currently one of the most common origins of death with increasing prevalence. European studies, however, demonstrated a general trend for a decreased CAD mortality in the last three decades [1]. Despite of the large variations between countries, CAD now is responsible for almost more than one million deaths/year (representing 20% of different types of deaths in Europe) [2].
The mortality of STEMI patients is affected by several factors like advanced age, Killip class at presentation, delayed treatment, the existence of well-structured STEMI dedicated networks of Emergency Medical System (EMS), strategy of management, MI history, renal insufficiency, diabetes mellitus, number of diseased coronaries, and Left Ventricular Ejection Fraction (LVEF) [3].
Many current investigations demonstrated decrements in the acute and long- term mortality in STEMI patients having more utilization of reperfusion therapy, primary Percutaneous Coronary Intervention (PCI), newer antithrombotics, as well as secondary preventive measures [4,5]. However, mortality is still concerning; the in- hospital mortality of STEMI patients in the national clinical registries of the ESC countries differed from 4 to 12% [6], and 10% for while the 1-year mortality among STEMI patients in angiography registries [7,8].
Primary Percutaneous Coronary Intervention (PPCI) is considered the best reperfusion strategy in STEMI patients within 12 h of the symptoms onset, provided it is carried out promptly (i.e., in less or equal to 120 min from STEMI diagnosis) by a competent team. A competent team contains not only interventional cardiologists but also proficient nurses, cardiovascular technician.
Studies demonstrated that the mortality rates were low among patients undergoing primary PCI in centers with a high volume of PCI procedures being performed [9]. Actual data proved that when primary PCI is carried out promptly and in high-volume centers, it leads to lower mortality [10]. Randomized clinical trials in high-volume, competent centers showed that if time delayed to treatment is comparable, primary PCI is superior to fibrinolysis in the reduction of Major Adverse Cardiac Events (MACE); namely, re-infarction, mortality, or stroke [11-14].
National Heart Institute (NHI) hospital center is the largest tertiary cardiovascular disease center in Egypt. About 3000 patients annually are admitted to NHI by myocardial infarction. Primary PCI is now the main reperfusion therapy for STEMI patients in NHI center.
This study aimed to explain the attributes of such patients, to assess STEMI management patterns with reference to the present usage of the reperfusion therapies, to evaluate the outcome of the in-hospital patients, and to compare Egyptian STEMI patients presenting to NHI center with other national Egyptian registries.
Methodology
STEMI unite observational registry approach
STEMI unite is a highly specialized coronary care unit in national heart institute center where only STEMI patients are admitted. We enrolled all patients presenting with unequivocal STEMI in their initial qualifying ECG since 20 October 2018 till 6 months afterwards. Patients were eligible for enrollment in the registry if they presented within 48 hours of symptom onset of STEMI defined as at least 1 chest pain episode lasting at least 20 minutes, demonstrated acute STEMI on their qualifying ECG with unequivocal changes (≥ 0.1 mV of ST-segment elevation in ≥ 2 adjacent limb leads or ≥ 0.2 mV in ≥ 2 contiguous precordial leads or new pathological Q waves) on surface electrocardiogram on admission, with no contraindication to primary PCI, and intended to be managed with primary PCI.
We excluded patients presenting to ER with STEMI more than 48 hours, patients with contraindication for primary PCI, and patients with concomitant valvular disease.
Data collection in the form of demographic characteristics including; age, sex, family history, cardiovascular risk factors, history of chronic illness, previous MI, onset of chest pain, duration before admission, and initial management of AMI.
Time from First Medical Contact (FMC) till wire crossing (reperfusion).
Findings of general and local examinations, ECG findings, angiographic characteristics and procedural complications were recorded [15-18].
Results
Baseline characteristics
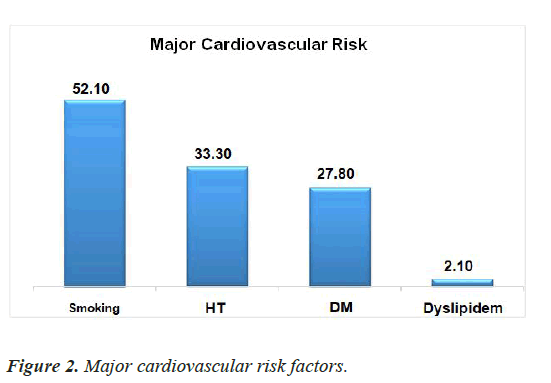
This study included a total of (n=1354) patient, mean age of 54.45 and SD of 11.04, (n=1320) 97.5% were less than 75 years old while only (n=34) 2.5% were more than 75 years old, 83.3% males (n=1129) and 16.7% (n=225) females as illustrated in Figures 1 and 2 and Table 1.
| Demographic data | All patients |
|---|---|
| N (%) | 1354 (100%) |
| Age (years) | |
| Mean ± SD | 54.45 ± 11.04 |
| Range | 14-87 |
| Gender | |
| Male | 1128 (83.3%) |
| Female | 226 (16.7%) |
| Risk factors | |
| Smoking | 705 (52.1%) |
| HTN | 451 (33.3%) |
| DM | 376 (27.8%) |
| Dyslipidemia | 28 (2.1%) |
Table 1. Demographic data.
STEMI patients with age less than or equal to 45 years old
296 patients were found, constituting 21.8% of all patients. The youngest presenting patient was 14 years old patient with a presentation of inferior wall myocardial infarction (STEMI) Killip class I and had primary PCI to an occluded PLV branch with adequate reperfusion and smooth in-hospital course. Further investigation and genetic testing revealed homozygous hereditary homocysteinaemia with significantly deficient methylene tetrahydrofolate reductase enzyme.
Further gender correlational analysis of cardiovascular risk factors revealed statistically significant findings; smoking is the most predominant risk factor in males (P-value<0.001), while diabetes and hypertension are in females (P-value<0.001 for each) as illustrated in Table 2. Dyslipidemia didn’t show gender correlation (P-value 0.209).
| Sex | Test of sig. | |||||||
|---|---|---|---|---|---|---|---|---|
| Male | female | Value | p value | sig. | ||||
| N | % | N | % | |||||
| Smoking | No | 438 | 38.80% | 210 | 93.30% | X2=223.62 | <0.001 | S |
| yes | 691 | 61.20% | 15 | 6.70% | ||||
| HTN | No | 796 | 70.50% | 107 | 47.60% | X2=44.48 | <0.001 | S |
| yes | 333 | 29.50% | 118 | 52.40% | ||||
| DM | No | 858 | 76.00% | 120 | 53.30% | X2=48.04 | <0.001 | S |
| yes | 271 | 24.00% | 105 | 46.70% | ||||
| Dyslipidemia | No | 1108 | 98.10% | 218 | 96.90% | Fisher exact test | 0.209 | NS |
| Yes | 21 | 1.90% | 7 | 3.10% | ||||
Table 2. Demographic data.
Further age correlational analysis, revealed that male patients were younger than females (P-value<0.001), smoking patients are younger than non-smokers (P- value<0.001) as illustrated in Table 3.
| Age | t-test | ||||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD | T | p value | sig. | ||
| Sex | male | 1129 | 53.41 | 10.97 | -83.3 | <0.001 | S |
| female | 225 | 59.58 | 9.91 | ||||
| Smoking | no | 649 | 57.05 | 10.5 | 8.47 | <0.001 | S |
| yes | 705 | 52.05 | 10.99 | ||||
| HTN | no | 903 | 53.27 | 11.32 | -5.63 | <0.001 | S |
| yes | 451 | 56.84 | 10.03 | ||||
| DM | no | 978 | 53.35 | 11.58 | -5.99 | <0.001 | S |
| yes | 376 | 57.35 | 8.85 | ||||
| Dyslipidemia | no | 1326 | 54.5 | 11.03 | 1.12 | 0.264 | NS |
| yes | 28 | 52.14 | 11.56 | ||||
Table 3. Demographic data.
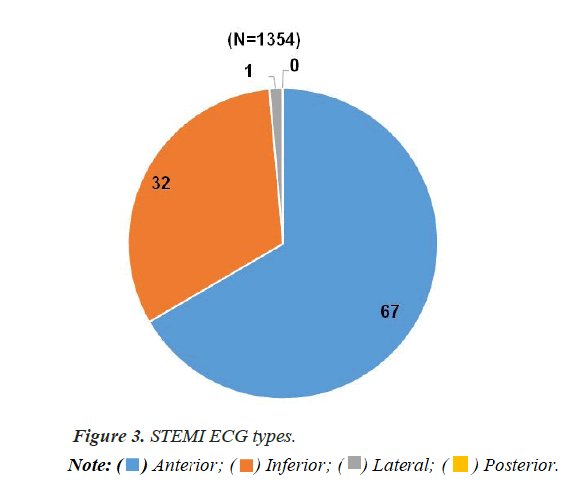
As illustrated in Table 4 and Figure 3; mean heart rate was 80.27 ± 11.59, mean systolic blood pressure of 126.93 ± 19.52, and mean diastolic blood pressure of 81.21 ± 36.1. 907 cases (67%) presented with anterior ST elevation myocardial infarction (including 8 cases presented with global ST elevation) while 436 cases (32.2%) presented with Inferior ST segment elevation m
yocardial infarction (including 8 cases presented with global ST elevation). 18 cases (1.3%) presented with lateral ST segment elevation myocardial infarction. 1 case (0.1%) presented with posterior ST segment elevation.
| Admission clinical and ECG data | All patients |
|---|---|
| N (%) | N=1354 (%) |
| HR (beat/min) | |
| Mean ± SD | 80.27 ± 11.59 |
| Range | 45-140 |
| SBP (mmHg) | |
| Mean ± SD | 126.93 ± 19.52 |
| Range | 80-200 |
| DBP (mmHg) | |
| Mean ± SD | 81.21 ± 36.1 |
| Range | 50-100 |
| STEMI ECG type | |
| Anterior | 907 (67.0%) |
| Inferior | 436 (32.2%) |
| Lateral | 18 (1.3%) |
| Posterior | 1 (0.1%) |
Table 4. Admission clinical and ECG data.
As illustrated in Table 5 correlational analysis of the type of myocardial infarction and cardiovascular risk factors didn’t reveal statistically significant correlations.
| MI | Chi square test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Anterior | Inferior | Lateral | ||||||||
| N | % | N | % | N | % | χ2 | p value | sig. | ||
| Smoking | No |
426 | 64.90% | 219 | 33.40% | 11 | 1.70% | 0.94 | 0.625 | NS |
Yes |
481 | 68.20% | 217 | 30.70% | 7 | 1.00% | ||||
| HTN | No |
623 | 68.50% | 275 | 30.20% | 12 | 1.30% | 4.47 | 0.107 | NS |
Yes |
284 | 63.00% | 161 | 35.70% | 6 | 1.30% | ||||
| DM | No |
664 | 67.40% | 309 | 31.40% | 12 | 1.20% | 2.65 | 0.266 | NS |
Yes |
243 | 64.60% | 127 | 33.80% | 6 | 1.60% | ||||
| Dyslipidemia | No |
890 | 67.70% | 425 | 31.90% | 18 | 1.40% | 1.08 | 0.583 | NS |
Yes |
17 | 60.70% | 11 | 39.30% | 0 | 0.00% | ||||
Table 5. Correlation of location of MI and major CV risk factors.
Characteristics of interventional management
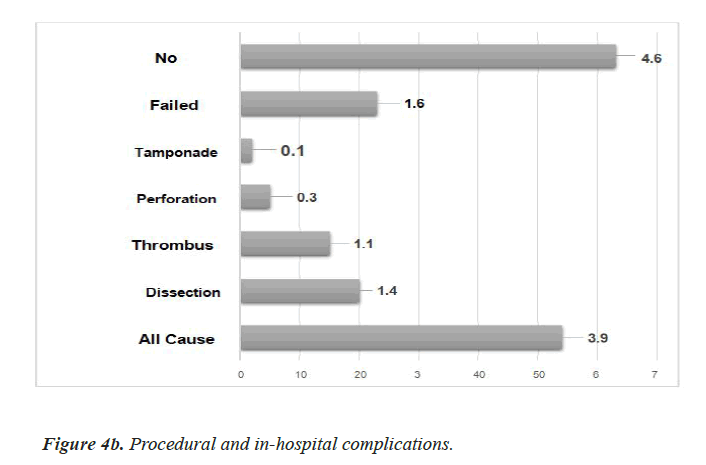
Procedural and in-hospital complications: The rates of procedural and in-hospital complications were; All-Cause Mortality 54 cases (3.9%), Dissection 20 cases (1.4%), Thrombus Propagation 15 cases (1.1%), Perforation 5 cases (0.3%), Tamponade 2 cases (0.1%), Failed PCI 23 cases (1.6%), and No Reflow 63 cases (4.6%).
Stented length: As illustrated in Table 6; mean length is 38.13 ± 17.29 and further analysis by correlation of stented length and conventional cardiovascular risk factors didn’t reveal statistically significant correlations as illustrated in Table 7.
| Parameter | All patients |
|---|---|
| N (%) | 1354 (100%) |
| Time from FMC to Wire crossing (min.) | |
| Median (Range) | 95 (20.0;170) |
| Time from Symptoms to FMC (min.) | |
| Median (Range) | 120.0 (60.0;240.0) |
| Contrast Amount (ml) | |
| Mean ± SD | 165.14 ±63.418 |
| Median (Range) | 150 (50 – 400) |
| Vascular access | |
| Radial | 96 (7.1%) |
| Femoral | 1256 (92.7%) |
| Revascularization strategy | |
| Primary PCI cases (total count) | 1354 (100%) |
| Primary PCI to Culprit artery only | 1218 (90%) |
| Total revascularization | 33 (2.4%) |
| CABG | 88 (6.5%) |
| Medical treatment | 15 (1.1%) |
| Procedural complications | |
| All-Cause Mortality | 54 (3.9%) |
| Dissection | 20 (1.4%) |
| Thrombus Propagation | 15 (1.1%) |
| Perforation | 5 (0.3%) |
| Tamponade | 2 (0.1%) |
| Failed PCI | 23 (1.6%) |
| No Reflow | 11 (0.8%) |
| Maneuvers and tools ( 1251 patients) | |
| Direct stenting / Total PCI | 813 (65%) |
| Pre-dilatation / Total PCI | 437 (34.9%) |
| Thrombectomy | 1 (0.07%) |
| Angiographic characteristics | |
| LM | 93 (6.9%) |
| LAD-D | 1095 (80.9%) |
| LCx-OM | 475 (35.1%) |
| RCA | 628 (46.4%) |
| Final TIMI flow grade | |
| TIMI 0 | 20 (1.5%) |
| TIMI I | 43 (3.2%) |
| TIMI II | 82 (6.1%) |
| TIMI III | 1209 (89.4%) |
| Stented length | |
| Mean ± SD | 38.13 ± 17.29 |
| Range | 14- 114 |
Table 6. Baseline data of interventional management of the whole registry population.
| Length | t test | ||||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD | t | p- value | sig. | ||
| Smoking | No |
601 | 38.47 | 17.63 | 0.65 | 0.519 | NS |
Yes |
650 | 37.81 | 16.98 | ||||
| HTN | No |
838 | 37.72 | 17.15 | -1.12 | 0.264 | NS |
Yes |
413 | 38.91 | 17.55 | ||||
| DM | No |
904 | 37.57 | 17.16 | -1.76 | 0.078 | NS |
Yes |
347 | 39.57 | 17.55 | ||||
| Dyslipidemia | No |
1225 | 38.07 | 17.22 | -0.88 | 0.379 | NS |
Yes |
26 | 41.5 | 20.8 | ||||
Table 7. Correlation of stented length and major CV risk factors.
Median time to FMC and median time to wire crossing: In this study the median time in minutes from symptoms onset to first medical contact in registered cases was 120.0 (60.0; 240.0). ER staff was the first medical contact (85% of patients), self and individual presentation was the mode of admission in 89% of patients. In our hospital the median time in minutes from first medical contact to wire crossing is 95 (20.0; 170).
Procedural aspects
Vascular access: Regarding vascular access in primary PCI management of cases, femoral access was utilized in 1256 cases (92.7%), while radial access was in 96 cases 7.1%. as illustrated in Table 6.
Contrast utilization: A mean of 165.14 ml and SD of 63.418 of contrast used in PPCI
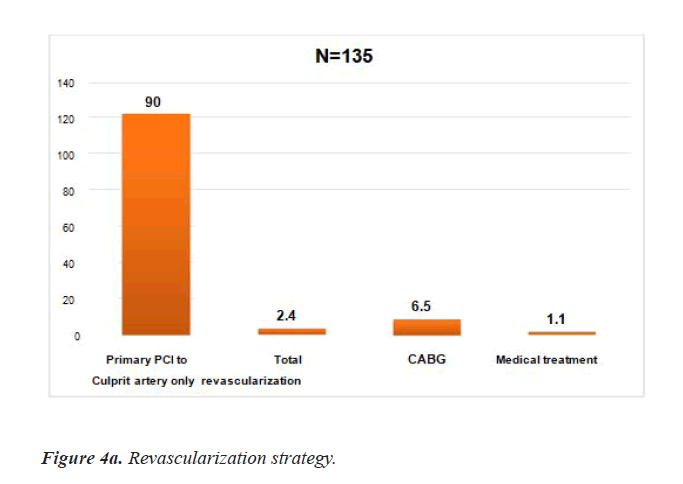
Revascularization strategy: Primary PCI of the culprit Infarct Related Artery (IRA) only strategy was the mainly utilized strategy being used in 90% of cases (1218 cases) while total revascularization was done in 2.4% of cases (33 of cases), CABG was done in 6.5% of cases, and medical management only was used in 1.1% (15 cases) as illustrated in Table 6 and Figures 4a and 4b.
Angiographic results
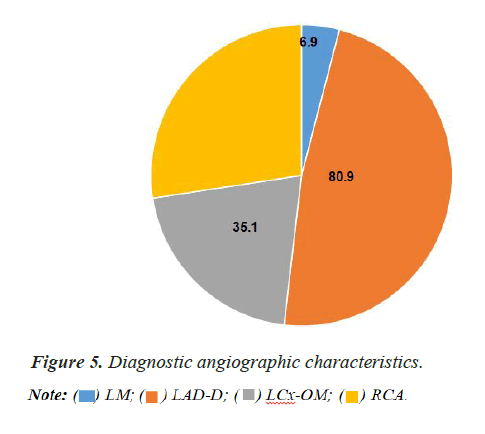
Angiographic results from this registry (single center data) showed a LM disease in 93 cases (6.9%), LAD-D disease in 1095 (80.9% cases), LCx-OM disease in 475 (35.1%), RCA in 628 (46.4%). From numeric prospective non-obstructive CAD was found in 7 cases (0.5%), single vessel CAD was found in 671 (49.6%), two vessel CAD was found in 443 (32.7%), three vessel CAD in 233 (17.2%), multi- vessel CAD in 676 cases (49.18%) (Figure 5).
Final TIMI Flow Grade (TFG)
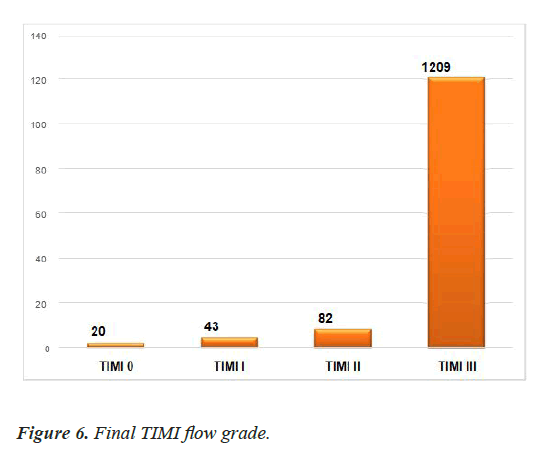
A thrombolysis in myocardial infarction flow (TIMI Flow) Grade III was achieved in 1204 cases (89.4%) identified as flow that implies a comparable flow rate of an infarct-related artery to a non- culprit artery, TIMI II in 80 cases (5.9%) identified as partial perfusion, TIMI I in 43 cases (3.2%) minimal perfusion, TIMI 0 in 20 cases (1.5%) identified as flow that signifies occlusion. Assessing No-reflow Phenomenon (NRP) after reperfusion in STEMI patients is mandatory in clinical practice. However, standardized no-reflow estimations by angiography are limited.
No-reflow is a dynamic phenomenon, and angiography can only demonstrate no-reflow early in its course in patients subjected to PPCI. General consensuses of the experts suggest assessing (NRP) at angiography with 2 major essential components; a TIMI flow grade of 0 and 1 and patent epicardial coronary artery. Moreover, coronary angiography cannot assess the microcirculation. Being at the initial point of angiography, it may not relate to Cardiac Magnetic Resonance (CMR) imaging, the ongoing gold standard for assessing Micro Vascular Obstruction (MVO). In the literature predominance of angiographic no-reflow in patients was assessed to be about 2.3% 18. In this study the no-reflow phenomenon was found in 63 cases (4.6%) (Figure 6).
Maneuvers and tools
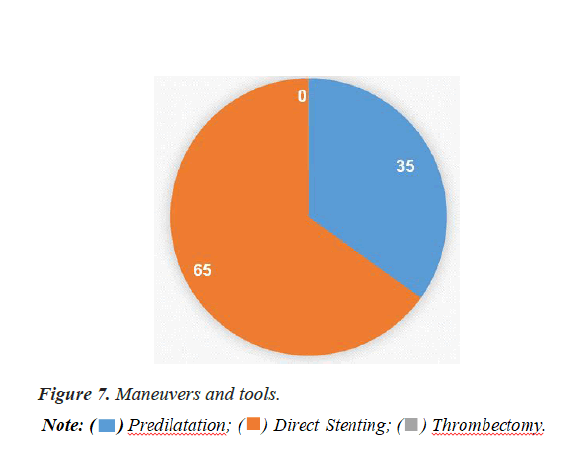
In our registry, PCI was done to 1251 patients. Pre-dilation was used in 438 cases (35%) while direct stenting was used in 813 cases (65%). Thrombectomy catheter was used in 1 case only (0.0007%) (Figure 7).

Discussion
It is well known according to data from Egyptian Society of cardiology (EgSc) and European Society Of Cardiology (ESC) that intended reperfusion treatment for STEMI in Egypt vs. different countries was primary PCI in 50.59% vs. 85.50%, thrombolysis in 43.14% vs. 5.55%, and no reperfusion in 6.05% vs. 4.72%. Taking into consideration that Egyptian contribution in this analysis was achieved through participation with 1356 patient from 19 Egyptian centers (multicenter data) [1].
As national heart institute is one of the largest cardiac centers in Egypt, our aim was to apply such type of reperfusion modality in Egyptian STEMI patients presenting to our center.
In our registry, mean patients’ age was 54.45 ± 11.04. Our patients were younger than EU countries (62.9 ± 12.4). Only 2.5% were more than 75 years, compared to 19.41% in EU countries.17 Patients with age less than 45 years represent 21.8%.
In our study we have fewer females (18.44%) as compared to female patients in EU countries (25.63%1), this may be due to youthfulness of the Egyptian population, poor control of risk factors, as well as non-adherence to medical treatment. Smoking is the most predominant risk factor (52.1%). Hypertensive patients represent 33.3% of our patients, while diabetic patients were only 27.8%.
The high incidence of smoking in Egypt was also detected by other studies such as that done by Shaheen et al. in which smoker represent 59.05% of the Egyptian patients, while hypertensive and diabetic patients represent 37.23% and 40.79% respectively. On the contrary, in EU countries hypertensive patients represent the majority (52.65%), and incidence of smoking (42.81%) was less than our registry 17. This raises the importance of increasing awareness of smoking cessation benefits.
Median time to FMC and median time to wire crossing
In the current study, the median time (min.) from symptoms onset to first medical contact in registered cases was 120.0 vs. 100 minutes in EU countries. The long time in may be due defect in the medical awareness of patients, reluctance in seeking medical attention and lack of well-organized referring emergency medical system with sufficient infrastructural support.
In this study the median time in minutes from symptoms onset to first medical contact in registered cases was 120.0 vs. 100 minutes in EU countries. The long time in may be due defect in the medical awareness of patients, reluctance in seeking medical attention and lack of well-organized referring emergency medical system with sufficient infrastructural support. In this study the median time in minutes from first medical contact to wire crossing is 95 minutes. In the guidelines, the ideal time should be less than 60 minutes [3]. Time delays may be related to logistics, the availability of 24 hour/7 day a week catheterization laboratory, availability of supplies.
On the controversy of that ESC guidelines recommendation that prefer radial access in primary PCI, our operators used femoral access in the majority of patients. This may be explained by defect in the supplies.
Culprit artery PCI only was done in the majority of the patients compared to total revascularization (90% vs. 2.4%). The latter technique was used by fewer operators in the presence of simple lesions in other arteries. Other patients who required PCI to other arteries were done after hospital discharge, and not before discharge as mentioned in the guidelines.
A TIMI Flow Grade III was accomplished in 1204 cases (89.4%). In another Egyptian study, TIMI flow grade III was completed in 80% of the patients with PCI within 3-10 hours after thrombolytic therapy. This may be due to earlier time of PCI. Mortality rate in this study was 3.9%. In another Egyptian multi-center study, where overall mortality rate in multiple hospital centers was 2.1% in patients with 1 ry PCI. The mortality rate of the Egyptian primary PCI patients is suggestive of better outcome compared to another study in which the in- hospital mortality rate among STEMI patients treated with primary PCI was 6.5% 17, while the rate of procedural complications was 5.3%.
Limitation of the study
Despite we try to restrict to the guidelines in our registry, the availability of the supplies may affect our decision in PCI. Absence of long term follow up is another limitation of our study.
Conclusion
Our single center experience suggests that STEMI patients in Egyptian population are likely to be younger, more current male smokers, diabetics, had higher prevalence of premature CAD, had significant time delays between symptoms onset to first medical contact, and more individual presenting rather than EMS presenting. Femoral access was the dominantly used access for PPCI. All stents used were drug eluting stents. Culprit only revascularization was the mainly used strategy, multi vessel disease staging intervention was done after hospital discharge. In-hospital mortality was comparable to other national registries.
Acknowledgment
All the authors contributed equally to this manuscript.
References
- Hartley A, Marshall DC, Salciccioli JD, et al. Trends in mortality from ischemic heart disease and cerebrovascular disease in Europe: 1980 to 2009. Circulation 2016;133(20):1916-26.
- Townsend N, Wilson L, Bhatnagar P, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37(42):3232-45.
- Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(07):119-77
- Puymirat E, Simon T, Danchin N, et al. USIK USIC 2000 Investigators, FAST MI Investigators. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. JAMA. 2012;308(10):998-1006.
- Gale CP, Allan V, Cattle BA, et al. Trends in hospital treatments, including revascularization, following acute myocardial infarction, 2003-2010: A multilevel and relative survival analysis for the National Institute for Cardiovascular Outcomes Research (NICOR). Heart. 2014;100(7):582-9.
- Kristensen SD, Laut KG, Fajadet J, et al. European association for percutaneous cardiovascular interventions. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: current status in 37 ESC countries. Eur Heart J. 2014;35(29):1957-70.
- Pedersen F, Butrymovich V, Kelbaek H, et al. Short- and long-term cause of death in patients treated with primary PCI for STEMI. J Am Coll Cardiol. 2014;64(20):2101-08.
- Fokkema ML, James SK, Albertsson P, et al. Population trends in percutaneous coronary intervention: 20-year results from the SCAAR (Swedish Coronary Angiography and Angioplasty Registry). J Am Coll Cardiol. 2013; 61(12):1222-30.
- Thiemann DR, Coresh J, Oetgen WJ, et al. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med. 1999;340(21):1640-48.
- West RM, Cattle BA, Bouyssie M, et al. Impact of hospital proportion and volume on primary percutaneous coronary intervention performance in England and Wales. Eur Heart J. 2011;32(6):706-11.
- Zijlstra F, Hoorntje JC, de Boer MJ, et al. Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med. 1999;341(19):1413-19.
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13-20.
- Widimsky P, Budesinsky T, Vorac D, et al. ‘PRAGUE’ study group investigators. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Final results of the randomized national multicentre trial-PRAGUE-2. Eur Heart J. 2003;24(1):94-104.
- Andersen HR, Nielsen TT, Rasmussen K, et al. DANAMI-2 Investigators. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349(8):733-42.
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018), Euro Heart J. 2019;40(3):237-69.
- Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Euro Heart J. 2018;39:119-77.
- Shaheen S, Wafa A, Mokarrab M, et al. Presentation, management, and outcomes of STEMI in Egypt: results from the European society of cardiology registry on ST elevation myocardial infarction. The Egyptian Heart J. 2020;72(1):35.
- Allencherril J, Jneid H, Atar D, et al. Pathophysiology, diagnosis, and management of the no-reflow phenomenon. Cardiovasc Drugs Ther. 2019;33(5):589-97.