Perspective - Hematology and Blood Disorders (2018) Volume 1, Issue 1
Myelodysplastic syndromes and elderly patients.
Roberto Castelli* and Luigi Bergamaschini
Department of Biomedical and Clinical Sciences, University of Milan, Luigi Sacco Hospital, Milan, Italy
- *Corresponding Author:
- Roberto Castelli, MD, Ph.D.
Luigi Sacco Department of Biomedical and Clinical Sciences
University of Milan, Luigi Sacco Hospital,Via G.B Grassi 74 20157 Milano, Italy
Tel: +39/02/50319830
E-mail: roberto.castelli@unimi.it
Accepted date: September 08, 2017
Citation: Castelli R, Bergamaschini L. Myelodysplastic syndromes and elderly patients. Hematol Blood Disord 2018;1(1):3.
DOI: 10.35841/hematology.1.1.1-2
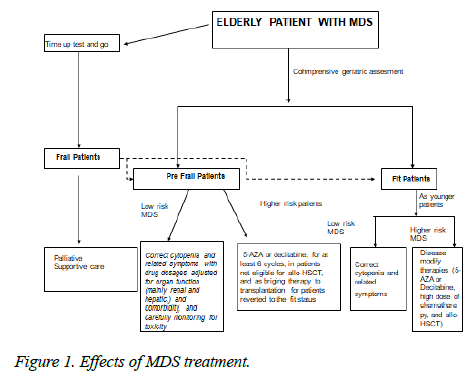
Visit for more related articles at Hematology and Blood DisordersMyelodysplastic syndromes (MDS) are a heterogeneous group of clonal hematopoietic stem cell disorders characterised by ineffective haematopoiesis, peripheral cytopenia, and possible transformation into acute myeloid leukemia (AML) [1]. On the phenotypic plane MDS range from indolent disease with a near-normal life expectancy to forms similar to AML. The incidence of MDS in the general population is 5/100,000, but it increases to 22-45/100,000 among subjects aged >70 years and continues to increases with advancing age, thus making it the most frequent hematological disease in the elderly [2]. Establishing the prognosis of these patients is a key step in disease management because treatment strategies depend on both the individual risk and their health status [3]. The primary aim of treating low-risk patients is to control symptoms; whereas high-risk patients may warrant potentially modifying therapies in an attempt to achieve a cure or prolong their survival. Advanced age is a major factor indicating a poor prognosis. Multiple comorbidities, a poor performance status at the time of diagnosis, decreased functional reserves, and limited social support all contribute to poor survival in elderly MDS patients [4]. Elderly may be under-treated because they may be considered too frail to tolerate potentially life-saving interventions such as antineoplastic treatment. On the other hand, due to their frailty, they are often prone to developing high-grade toxicities. The available therapies for MDS range from treating symptomatic cytopenia in low-risk patients [5] to immunomodulatory agents [6], chemotherapy or allogeneic stem cell transplantation [7]. However, although advanced age is often an a priori factor limiting the choice and/or aggressiveness of treatment options, chronological age correlates poorly with frailty and is therefore insufficient when deciding on specific treatment for individual patients. It is therefore highly recommended to assess the functional ability of elderly MDS patients further in order to ascertain their medical and bio-psychosocial background. For those reasons the decisional algorithm for treating myelodysplastic elderly patients reasonably should include diagnosing the subtype of MDS (WHO classification) and assessing their prognosis on the basis of risk, as well as a comprehensive geriatric assessment (CGA) that allows an estimate of life expectancy and treatment tolerance, and the identification of reversible conditions that may interfere with treatment choice. By integrating chronological age with life expectancy, and the MDS classification with a geriatric assessment (CGA), it should be possible to achieve a personalised treatment. We suggest that all elderly MDS patients should undergo a timed up and go test (TUGT) [8] as a preliminary means of identifying frail patients, and that all non-frail patients should then undergo a comprehensive geriatric assessment (CGA) in order to distinguish frail and pre-frail patients. Non frail (fit patients) should receive standard dose treatment according to risk assessment like younger patients. Pre-frail patients should receive individualized therapy and should be re valuated periodically in order to asses if they should reverse to fit status. If not, tailored therapy include in low risk patients treatment of anemia with Erythroid stimulating agents which are generally well tolerated by pre-frail patients, in higher risks patients 5 AZA and Decitabine is generally better tolerated than AML like chemotherapies. If they turn in fit status, they became candidates to BMT. Frail patients (non-fit patients) should receive symptom-related therapy which generally consist of transfusion supportive care. In the follow-up, a repeated CGA may be useful to evaluate the haematological, cognitive and socio-relational effects of MDS treatment (Figure 1).
References
- Tefferi A, Vardiman JW. Myelodysplastic syndromes. N Engl J Med. 2009;361:1872?85.
- Germing U, Aul C, Niemeyer CM, et al. Epidemiology, classification and prognosis of adults and children with myelodysplastic syndromes. Ann Hematol. 2008;691?99.
- Gidaro A, Deliliers GL, Gallipoli P, et al. Laboratory and clinical risk assessment to treat myelodysplatic syndromes. Clin Chem Lab Med 2016;54.
- Stauder R, Nösslinger T, Pfeilstöcker M, et al. Impact of age and comorbidity in Myelodysplastic syndromes. JNCCN J Natl Compr Cancer Netw 2008;6:927?934.
- Killick SB, Carter C, Culligan D, et al. Guidelines for the diagnosis and management of adult myelodysplastic syndromes. Br J Haematol. 2014;164:503?525.
- Castelli R, Cassin R, Cannavò A, et al. Immunomodulatory drugs: new options for the treatment of myelodysplastic syndromes. Clin Lymphoma Myeloma Leuk 2013;13:1?7.
- de Witte T, Bowen D, Robin M, et al. Allogeneic hematopoietic stem cell transplantation for MDS and CMML: recommendations from an international expert panel. Blood. 2017;129:1753?62.
- Beauchet O, Fantino B, Allali G, et al. Timed Up and Go test and risk of falls in older adults: a systematic review. J Nutr Health Aging. 2011;15:933?8.