Research Article - Current Pediatric Research (2022) Volume 26, Issue 6
Multidisciplinary hospital management of child sexual abuse in a tertiary care hospital.
Chandrika Rao1*, Nimrat Sandhu1, Gayatri Devi Sivasambu2, Shailaja Avinash1, Girishchandra YP1, Aashika Maria Naidu1
1Department of Pediatric, MS Ramaiah Medical College, Bengaluru, India
2Department of Ob-Gyn, MS Ramaiah Medical College, Bengaluru, India
- *Corresponding Author:
- Dr. Chandrika Rao, Department of Pediatric, MS Ramaiah Medical College, New BEL road, Mathikere, 560054, Bengaluru, E-mail: chandrikadoc@gmail.com
Received: 08 June, 2022, Manuscript No. AAJCP-22-66161; Editor assigned: 09 June, 2022, PreQC No. AAJCP-22-66161 (PQ); Reviewed: 14 June, 2022, QC No. AAJCP-22-66161; Revised: 15 June, 2022, Manuscript No. AAJCP-22-66161(R); Published: 29 June, 2022, DOI:10.35841/0971-9032.26.6.1458-1462.
Abstract
Introduction: The introduction of the POCSO act in India has provided clarity on the definitions of child sexual abuse. Studies on child abuse cases are sensitive and less in India. Hence, this study was conducted to determine the correlates of child sexual abuse cases presenting to the hospital and review the multidisciplinary approach present in the institution for the management of adolescent sexual abuse. Methods: A retrospective study conducted by the pediatric department in a tertiary hospital, Bangalore, where 70 adolescent case files of sexual abuse in adolescents over 2 years were analyzed. Study was approved by the institutional ethics committee. Assent and consent was obtained for all the cases. All cases were registered as medico legal and confidentiality was maintained. Results: 70 adolescent case files with sexual abuse were enrolled, of which 68 were females. 62%were aged between 13-15 years, 31% were 10-13 years. 88% were brought by the police, 20% by parents and 2% by relatives. The perpetrator was a member of the family in 48%, 2% by their father and 4% by their brothers. In 46%, the perpetrator was a stranger. 4% sustained genital injuries as bruises, vaginal tears and laceration on inner thigh and gluteal region. 2% received eye injuries. 65% were abused forcefully. Conclusion: Risk factors were urban, poor socioeconomic background, mid and late adolescence. 48% perpetrators were from family. 65% were abused forcefully. Our study highlights the fact that management by multi-disciplinary team (CCRU) is feasible and enables an organized approach by giving care in single step.
Introduction
WHO defines sexual abuse as “involvement of a child, less than 18 years in sexual activity, that he or she does not fully comprehend, is unable to give informed consent to, or for which the child is not developmentally prepared and cannot give consent, or that violates the laws or social taboos of society” [1].
Studies on child abuse cases are sensitive and less in India. The victims of CSA or their parents have to disclose their suspicions to the authorities. Many reports of child abuse are never passed on. It is difficult for the child and families to disclose and is influenced by several factors, like implicit or explicit pressure for secrecy, feelings of responsibility or blame, feelings of shame or embarrassment, or fear of negative consequences. Mandatory reporting which has been introduced may increase the reported abuse in India.
Management of sexual abuse cases require a holistic approach by the treating team and the forensic team, because apart from physical injuries, sexually abused adolescents are also seen to have long term effects such as mental health disturbances. Adolescents who are sexually abused face risks of posttraumatic stress disorder, anxiety disorder, sleep disorders, depression including thoughts of suicide and self-harm. They are likely to engage in unsafe-sex, drug abuse and misuse of alcohol leading to higher risk for STIs and HIV. These cause negative health outcomes that last into adulthood. A recent study done in Canada by Gagnon et al. [4], states that children subjected to sexual abuse have higher chances of symptoms of genital or urinary health. Various challenges take place during the management, one of the biggest challenges remain- timely examination, and lost to follow up cases.
Hence, this study was conducted to determine the correlates of child sexual abuse cases presenting to the hospital and review the multidisciplinary approach present in the institution for the management of adolescent sexual abuse. The analyzed information will help pediatricians and physicians to manage the child abuse cases in a holistic manner.
Methodology
Ethics statement
This study was approved by the Institutional ethics committee in MS Ramaiah medical college, Bangalore, and Karnataka, India. Assent was obtained from individual’s above12 years and consent was obtained for all the cases from the parents. All cases were registered as medico legal and ethical clearance was taken and confidentiality was maintained. Written and informed consent taken for history, recording of injuries on examination were noted. Confidentiality of records and identity has been maintained throughout.
Study design: A retrospective was conducted on case files of adolescents with alleged sexual abuse to determine demographic, clinical characteristics and related factors.
Subjects and study setting: It was a retrospective study conducted by the department of pediatrics in a tertiary hospital, Bangalore, where case files of sexual abuse in adolescents (10-18 years) over a span of 2 years were analyzed.
Selection criteria: All case files of adolescents (10-18 years age) with history of alleged sexual abuse reporting to the hospital were included in the study.
Exclusion criteria: If Caregivers had not consented to children giving history or examined.
Sample size: A total of 70 adolescent case files were examined.
Sampling method: Convenience sampling.
Measurements and data collection: Data of epidemiological details like age, gender, geography, alleged perpetrator details, clinical characteristics, details of investigation and timing of physician`s response were collected.
Once the child abuse case reported to the hospital, pediatricians recorded the history, did a general physical examination, gynecologists examined for any genital injuries and psychiatry did a mental state examination. Psychiatric evaluation of the individuals was done. Females were examined in the presence of a female doctor or a nurse. Vitals and anthropometry was recorded for all cases. Relevant investigations were done such as the routine blood work up, urine examination, swabs from genital area and from injury marks. HIV and Urine pregnancy test was performed. Data of children who did not give history was not included.
Data from all these cases was recorded age group, demographic details such as residence: Urban or rural, socio economic background. Information about the perpetrator was recorded like age, background and occupation. General physical examination was done, anthropometry was recorded. Time taken for examination by each part of the CCRU team of pediatricians, gynecologists and psychiatrists was noted. The type of abuse, associated morbidities and the treatment offered (in terms of NSAIDS, Retroviral and counseling) were also recorded.
Results
A total of 70 adolescent cases with sexual abuse were enrolled, of which 68 were females. Of the 70 cases, 62% were aged between 13-15 years, studying in classes 9th and 10th respectively. 31% were in the age bracket of 10-13 years and 5% of the individuals belonged to late adolescents. 88% was brought by the police, 20% by parents and 2% by relatives. 84% of the children were residents of Bangalore, 7% from construction sites, mining sites and 8% from rural background. Caregiver demographics in Table 1.
|
|
Characteristics |
Percentage |
|---|---|---|
|
Socioeconomic background (as per Kuppuswammy scale ) |
upper class |
2% |
|
upper middle class |
75% |
|
|
lower middle class |
15% |
|
|
upper lower class |
5% |
|
|
lower class |
2% |
|
|
Primary caregivers |
Parents |
91% |
|
Single parent |
6% |
|
|
Grandparents |
4% |
|
|
Education level |
Illiterate |
12% |
|
Educated below 10th std |
51.50% |
|
|
Educated above10th std |
36.50% |
|
|
Employment |
Employed |
76.30% |
|
Not employed 23.7 |
Table 1. Characteristics of caregivers for adolescents.
65% adolescents were found to be calm and cooperative describing the scene clearly. 25% were fearful of the genital examination, 10% of the adolescent children were crying, scared and 2% remained silent upon asking history and while examining. Care was taken to provide privacy and support to the children in the hospital. Counseling and psychological assistance was provided to the children who were scared or crying.
On taking history from the individuals, the perpetrator was a member of the family in 48%, 2% was abused by their father and 4% by their brothers. In 46%, the perpetrator was a stranger as per the disclosure. 12% of the cases did not given consent for the examination. These were all above the age of 16 years. 42% of the cases had low BMI and were malnourished. 70% of the adolescents had SMR stage [4]. No developmental delay cases were seen (Table 2).
| Offence | Result |
|---|---|
| Sexual harassment | 4% |
| Sexual assault | 78% |
| Aggravated sexual assault | 1% |
| Penetrative sexual assault | 10% |
| Aggravated penetrative sexual assault | 8% |
Table 2. Classification after a genital examination.
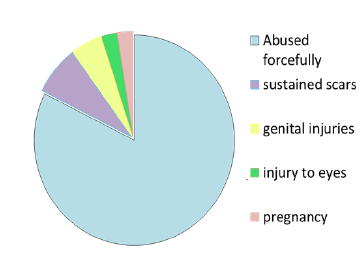
Injuries: 65% were abused forcefully, 6% sustained deep scars on face and over the breasts, for which medical attention was given. 4% sustained genital injuries as bruises, vaginal tears and laceration on inner thigh and gluteal region. 2% received superficial injury over the eye; however vision was noted to be normal (Figure 1).
Analyzing the response of the team
78% were examined by obstetricians. All the cases were counselled by pediatrician, gynecologist and 17% by psychiatrist. The average time taken for the team to complete management was 45-60 mins. 11 cases took more than one hour due to factors like doctor being busy with another case (3 cases), referral to other specialists (4 cases), cases requiring surgical management (2 cases), child waiting for one relative to come to hospital before giving history (2 cases).
Following genital examination, all children were subjected to blood test–HIV, HbSAg, HCV and urine pregnancy test. 2 adolescent girls were pregnant. Out of which the 1st was detected at 8 weeks when the adolescent was brought to A and E. and the 2nd case was detected at 16 weeks. Both were admitted in the hospital and were managed. 11% adolescents were admitted, out of which 65% were counselled and 4% received retro viral therapy and 3% were given NSAIDS and a due course of antibiotics. Hbs Ag and HCV were negative in all cases.
Discussion
Sexual abuse is evidenced by activity between a minor child and an adult or another child who by age or development is in a relationship of responsibility, trust or power, the activity being intended to gratify or satisfy the needs of the other person”, as stated by the WHO.
The incidence of such cases in India have increased great folds posing great challenges to manage, treat and prevent these incidents altogether. We as a country have seen unnerving cases like Nirbhaya, Shakti Mill case or Asifa bano or widely known as the Kathua rape case. Following these stringent laws has been brought into action which not only requires a positive medical evidence and strict punishments of imprisonment and life sentence under section 375,354,377. In our study we studied 70 adolescents who were abused in a study period of 2 years.
Role of a pediatrician comes to play in treating the physical as well as the mental problems such as shame, guilt, isolation, building boundaries which contribute to sleep and eating disorders hence leading to bad school performance. On admission the emergency 17% of the adolescents were examined by the psychiatrist and a mental state examination was done. The CCRU (Collaborative Child Response Unit) of our hospital continues to follow these adolescents. Goldenring et al. [5], described the ideal psychosocial screen of interviewing called HEEADSSS, focusing on assessment of the home environment, education and employment, eating, peerrelated activities, drugs, sexuality, suicide/depression, and safety from injury and violence.
Sexual abuse can have both immediate and long term effects. Management of both are required for a more holistic approach [5,6]. Physical injuries such as genital injuries, eye injuries, scars over breasts, bite and scratch marks require immediate medical attention. In the emergency the protocol is to first provide aid following by registering a medico legal file. Both history and examination play an imperative role in furnishing the case. In our study we found 65% adolescents were abused forcefully and 12% sustained injuries. Nina et al. [7] studied Narrative Exposure Therapy (NET), using the lifeline method of question “what happens next”. It was seen that it helped the child to open up and talk about the incidence and gradually give away feelings of guilt with a long term effect of better performance at school.
Casler et al. [8], did an informative study targeting college teens in division of adolescent hospital of Pittsburgh and found students who experienced rape, before entering college were more likely to experience the same in college. He then developed a trauma-based approach leading to a safe environment using the same model and targeting those children who experience rape before college. It was noted that 8%-11% of women experienced rape in each semester. In our study, higher risk was noted in the mid adolescent age group (64%), suggesting vulnerability and the ability of being easily over powered.
Flaherty et al. [9] in their analysis of 41 children, hospitalized due to the injuries of victimization, revealed that 76% of the perpetrators were males. Biological fathers of the victims seem to have a higher preponderance to other close male relatives like adoptive fathers, mother`s boyfriends, stepfathers, other relatives, day care providers, or even friends. 90% of children who were physically assaulted or both physically and sexually assaulted were exposed to similar incidents at home, usually against their mothers. Associations with socio demographic background, experience of abuse, relation to parents, health and risk behaviours have been studied by Linda et al. [10], where 9.7% of adolescents felt that they had been persuaded, pressed or coerced on at least one occasion. Sexual interaction under pressure was seen as constituting sexual abuse. Various incarcerated experiences quoted by the perpetrators were studied by Morris et al. [11], such as drugs, exposure to parents who were violent in the, being a victim of physical or sexual assault, having parents who encouraged gang membership exerted an important influence. Studies by Mathur et al. [12,13], Chimdessa et al., show that strangers were the main perpetrators in abuse of street children, working children, and children in institutional care.
An important socio cultural factor studied by Choudary et al. [14], in child sexual abuse was family secrecy. Because of which sexual abuse is considered inappropriate or a taboo causing lesser number of cases to be reported and long term leading to depression, shame and guilt in the adolescents. This is one of the most common reasons why male sexual abuse is under reported. A study by Gagnier [15] found that majority of the men in the study waited until adulthood to disclose their abuse due to the negative stereotypes like taboo which contributed to delayed disclosures as they got both positive and negative responses on disclosure. Out of the 18% population adolescents contribute to in the world, only 1% can seek help from professionals for mental health disorders, making suicide the third leading cause of their mortality as explained by Kommu et al., in their study on behaviour of adolescents [16].
64% witnessed the abuse by 3 years and 46% between 12 to 18 years. Psychiatric evaluation revealed 46% showed more depression and more behavioural problems. We observed in our study that 48% of the perpetrators were known to the adolescent. 6% were abused by their family members be it fathers or brothers. This proves that they misused the vulnerability of the adolescents and took undue advantage of being closer in proximity.
A study done by Vrolijk on the difficulties faced during sexual abuse examination highlights the importance of working of Collaborative Child abuse Unit (CCRU) and also elaborates that video graphic documentation is preferred above photographic documentation for ano genital examination also that observations of children’s behavioural reactions during examinations might be valuable in the evaluation of suspected sexual abuse specially for long term follow up. CCRU is an example of such a setup which provides medical care, gynaecological check-up and a psychiatric evaluation and long term follow up. To assess the trauma symptoms in children CRIES-13 and the CAPS-CA can be used .The assessment should always be done multidisciplinary by experienced professionals because not only do they care for children, they also know how child protective agencies and law enforcement are organized [16,17].
Psychiatric role in treating the trauma aspect of abuse is emerging. Studies show trauma causes alterations in neural structure and methods such as dissociation of trauma types and of trauma versus chronic stress, acknowledging the importance of hypo and hyper responsiveness caused due to decreased engagement of components of the basal ganglia require long term follow up [18]. In a study done in Assam by Tamuli et al. [19], they found that in majority cases there was no evidence of forceful sexual intercourse at the time of examination due to long time interval between the act and medical examination. They reinforce the need of a CCRU unit for such cases and training for prompt reporting starting from the victim to the legal authority. Our study highlights the importance of social patterns of abuse among adolescents. It also highlights the importance of a multi-disciplinary medical team approach towards cases of abuse. Limitation of the study was that cases included were from one centre, lesser number of cases was seen in emergency by psychiatrist and follow up of the cases were not included.
Conclusion
In this study, risk factors were urban and poor socioeconomic background. The age group of mid and late adolescence had higher number of cases. 48% perpetrators were known to family and 75% belonged to upper middle class. 65% was abused forcefully. Our study highlights the fact that management by Multi-disciplinary team (CCRU) is feasible and enables an organized approach by giving care in single step.
Acknowledgements
We would like to thank all medical personnel involved in this study: The physicians of the CCRU team, nurses, social workers, laboratory staff, administrative staff, adolescents and caregivers who participated in the study.
Conflict of Interest
No existing or potential conflict of interest relevant to this article was reported.
References
- https://www.who.int/news-room/fact-sheets/detail/violence-against-women
- Olafson E. Child sexual abuse: Demography, impact, and interventions. J Child Adolesc Trauma 2011; 4: 8-21.
- http://www.mapsofindia.com/my-india/government/the-protection-of-children-from-sexual-offences-act-2012-pocso
- Vézina-Gagnon P, Bergeron S, Hébert M, et al. Childhood sexual abuse, girls' genitourinary diseases, and psychiatric comorbidity: A matched-cohort study. Health Psychol. 2021; 40(2): 104-112.
- https://www.peds.arizona.edu/sites/default/files/curriculum-files/headss.pdf
- Hornor G. Child sexual abuse: Psychosocial risk factors. J Pediatr Health Care 2002; 16(4): 187-92.
[Crossref] [Google Scholar] [Indexed]
- Fávero M, Rodrigues I, Fátima F, et al. Children and adolescents indirect victims of the child sexual abuse. The Journal of Sexual Medicine 2017; 14(5): e310-e311.
- Mc Cauley Heather L, Casler Adam W. College sexual assault: A call for trauma-informed prevention. J Adolesc Health 2022; 56(6): 584–585.
[Crossref] [Google Scholar] [Indexed]
- Flaherty EG. Analysis of caretaker histories in abuse: Comparing initial histories with subsequent confessions. Child Abuse Negl 2006; 30 (7): 789-798.
[Crossref] [Google Scholar] [Indexed]
- Jonsson LS, Fredlund C, Priebe G, et al. Online sexual abuse of adolescents by a perpetrator met online: A cross-sectional study. Child Adolesc Psychiatry Ment Health 2019; 13: 32.
[Crossref] [Google Scholar] [Indexed]
- Morris RE, Anderson MM, Knox GW. Incarcerated adolescents' experiences as perpetrators of sexual assault. Arch Pediatr Adolesc Med 2002; 156(8): 831–835.
[Crossref] [Google Scholar] [Indexed]
- Mathur M, Rathore P, Mathur M. Incidence, type and intensity of abuse in street children in India. Child Abuse Neglect 2009; 33: 907-13.
[Crossref] [Google Scholar] [Indexed]
- Chimdessa A, Cheire A. Sexual and physical abuse and its determinants among street children in Addis Ababa, Ethiopia 2016. BMC Pediatr 2018; 18: 304.
- Aparajita Ch, David K, Carson Cecyle K, et al. Family life education in India: perspectives, challenges, and applications. (1st edn) Rawat Publications 2006; pp: 31–57.
- Gagnier C, Collin-Vézina D. The disclosure experiences of male child sexual abuse survivors. J Child Sex Abus 2016; 25: 221–241.
[Crossref] [Google Scholar] [Indexed]
- Kommu JVS, Jacob P. Specialty training in child and adolescent psychiatry in India. Eur Child Adolesc Psychiatry 2020; 29(1): 89-93.
[Crossref] [Google Scholar] [Indexed]
- Vrolijk-Bosschaart TF, Brilleslijper-Kater SN, Benninga MA, et al. Clinical practice: Recognizing child sexual abuse-what makes it so difficult? Eur J Pediatr 2018; 177(9): 1343-1350.
[Crossref] [Google Scholar] [Indexed]
- Thomason ME, Marusak HA. Toward understanding the impact of trauma on the early developing human brain. Neuroscience 2017; 342: 55–67.
[Crossref] [Google Scholar] [Indexed]
- Tamuli RP, Paul B, Mahanta P, et al. A statistical analysis of alleged victims of sexual assault-A retrospective study. J Punjab Acad Forensic Med Toxicol 2013; 13(1): 7.