- Biomedical Research (2013) Volume 24, Issue 1
Microproteinuria in chronic cigarette smokers as a predictor of renal diseases: A case control study.
Shah Trushna1*, and Purohit Geetanjali2
2Department of Physiology, SBKS MI & RC, Sumandeep Vidyapeeth, Piparia, 391760,Vadodara, Gujarat, India
- *Corresponding Author:
- Trushna Shah
Department of Biochemistry
SBKS MI & RC, SumandeepVidyapeeth
Piparia, 391760
Gujarat
India
Accepted date: November 03 2012
Abstract
It was a case control study of 60 subjects. The aim of this study was to compare the microproteinuria and other kidney functions between tobacco smokers and non-smokers, determining whether smoking is associated with an increased risk for chronic renal failure (CRF) overall and by type of renal disease. 60 subjects, in two different groups (30 in each) were studied in SSG hospital, Vadodara. 30 subjects were participated as a study group (Group II), with chronic tobacco smoking habits. 30 healthy participants, who had never used tobacco, were studied as control group (Group I). The assessment consisted of urine analysis for microproteinuria, creatinine clearance test and blood analysis for urea and creatinine level. Blood pressure and BMI were also evaluated. Both the groups were compared using the unpaired Student's t-test for significance. Both the groups did not differ significantly in sex structure and body mass index, but the blood pressure values were significantly higher in group II (SBP=120.6±8.6 vs 140.6±6.6 and DBP=76.8±4 vs 86±4.4). Group II participants were characterized by higher microproteinurea (61.53±12.9mg% vs. 241±20.3mg%; p<.0001), though there were no significant changes in other kidney functions. The smokers were significantly younger, which may points to the earlier origin of microproteinuria in smokers (42.1 +/- 11.0 years). We concluded that chronic tobacco consumption causes kidney damage in various manner, produces microproteinuria as an early predictor of renal diseases.
Keywords
Microproteinuria, Serum creatinine, Blood Urea, Creatinine clearance
Introduction
Tobacco chewing and smoking are the leading causes of cancer and death globally. It was recently suggested that smoking, in addition to its well-known cardiovascular consequences, could accelerate the progression of renal diseases.[1]Cigarette smoking is considered to be the most common identifiable cause of adult death in developed countries[2] and further increasing evidences suggest that chronic smoking is a risk factor for the progression of nephropathies[3]. Tobacco smoking has a similar influence on the progression of nephropathies in patients with type 2 diabetes mellitus [4] and polycystic kidney disease,[5] but studies regarding the effect of smoking on renal function in subjects without renal disease are scarce.
Further it is unknown whether chronic smoking affects renal function or represents a cause of renal damage in subjects without pre-existing renal diseases, so study of the renal effect of smoking in normal subjects could provide valuable information regarding the relationship between smoking and the progression of nephropathies. Microproteinuria is defined as, small quantity of protein (30- 300 mg %) excreted in urine per day. It is an early indicator for the progressive kidney damage. This study was carried out in chronic cigarette smokers to evaluate the relation of nicotine to the renal functions like level of proteins in urine, serum creatinine level, blood urea level and creatinine clearance test.
Material and Method
This study was carried out in S.S.G. Hospital, Vadodara, during the period of 2007-2009, after ethical committee clearance. It was conducted in 60 subjects, in two different groups, each contain 30 participants. Subjects with tobacco smoking were included in experimental group (Group II) and further compared with control group (Group I). A face-to-face interview and a selfadministered questionnaire provided information about smoking habits and other lifestyle factors. Never smokers were defined as individuals who had never used tobacco. Those participants, who were taking 2 packets per week, since last 10 years or more, were included in group II. This questionnaire also included information about alcohol consumption, anthropometric measures, dietary habits, and education, medical history, use of analgesics, and occupations etc. A physician recorded clinical parameters including age, weight, and height, systolic and diastolic arterial pressure.
Inclusion criterias;
1. Age between 30-50 years for both groups.
2. Selection was irrespective to sex.
3. Group II, having smoking habit for more than 10 years.
Exclusion criterias;
1. Patients of any systemic or metabolic disease like diabetes mellitus and renal diseases.
2. Patients of vascular disease like renal artery stenosis
3. Alcoholic and those who were taking any medication
4. Pregnant female
Collection of sample:
Urine sample: For both groups 24 hr. urine sample was collected and store in the refrigerator at 4°C. Thymol was used as preservative for urine sample.
Blood sample
5 ml venous fasting blood sample was collected in a syringe under aseptic precautions. The sample was allowed to clot at room temperature and serum was separated for further analysis.
Biochemical investigations
Following methods were used for the biochemical investigations
➢ Urine protein – Colorimeter end point method (Pyrogallol reagent)[6]
➢ Serum creatinine – Jaffe’s method (without deproteinisation method) [7]
➢Blood urea – Berthelot method[8]
➢Creatinine clearance – by the standards procedure and calculation (UV/P)[9]
Data analysis
Statistical analysis involved quantitative variables summarized through mean± SD. Difference between means of the two groups was analyzed for significance, using student’s unpaired t- test. α error was set at 5% level (p < 0.05).
Observations & Results
This study was carried out in Department of Biochemistry, SSG hospital, Vadodara. Database was prepared in form of a master chart. Routine examination of group I showed that all of them were normotensive, but the group II subjects showed significantly higher blood pressure (SBP=120.6±8.6 vs. 140.6±6.6 and DBP=76.8±4 vs. 86±4.4). None of them were using any other medications. Clinical history was normal in recent six months. Biochemical investigations of both groups were compared and the observations were as follows.
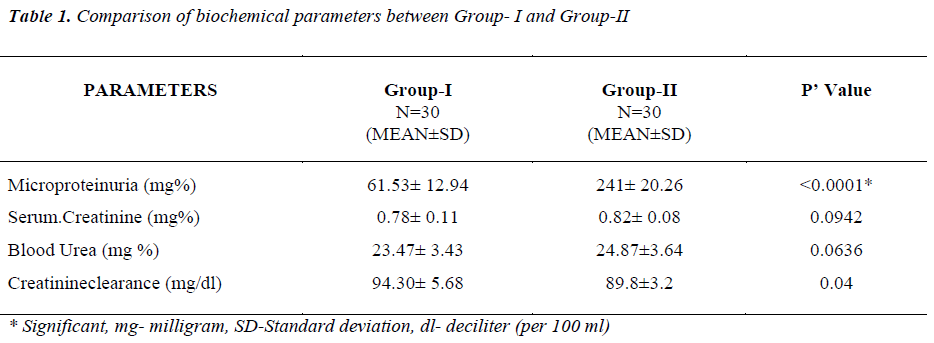
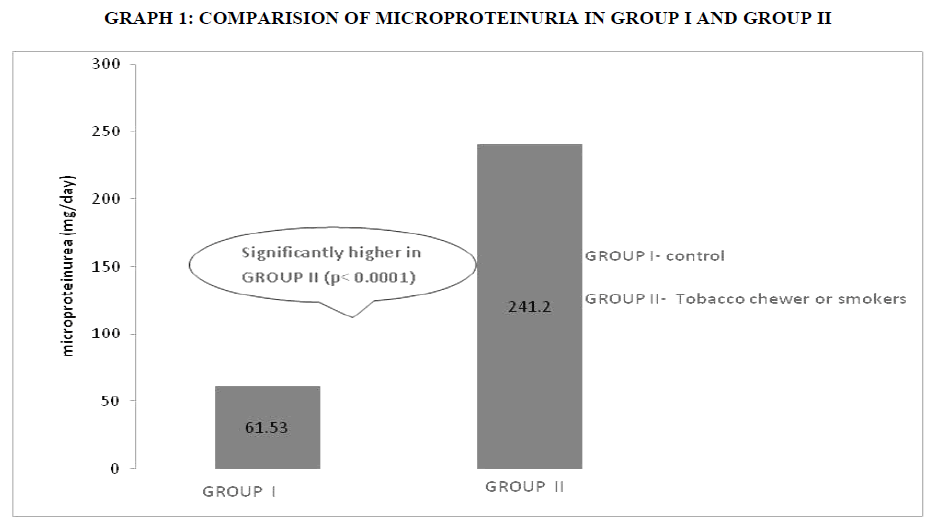
As per table1, microproteinuria is significantly higher (61.53±12.9mg%vs.241±20.3mg%; p< 0.0001) in group II, those who were, tobacco smokers as compare to nonsmokers (graph 1). Other renal functions like serum creatinine level, blood urea, creatinine clearance test were altered but within clinical limit.
Discussion
This study evaluated the effect of chronic cigarette smoking on renal functioning. Observations suggested that tobacco users were hypertensive as compare to control. Smoking increases the risk of hypertension by some 2 to 3 times, due to increase in sympathetic tone [10], the latter may interfere with the action of some hypertensive agents.[11] Microproteinuria may be due to various pathophysiological, mechanisms in smokers and tobacco chewers Nicotine increases masengial cell proliferation via activation of nicotinic receptors [12]. Nicotine increases synthesis of fibronectine, which is critical matrix component involved in the progression of chronic kidney diseases [13] Smoking induces a transient decrease in renal plasma flow and glomeruler filtration rate.[14,15] These small repeated episodes of transient renal hypoperfusion may damage some glomeruli which may result in hyperfiltration, together with capillary albumin leakage. [16,17]
Studies reported that cigarette smoke contain glycotoxins, form advance glycation end products ,which may enhanced vascular permeability causes albuminurea.[ 18,19,20] Interestingly, it was demonstrated that cigarette smoking (or nicotine) could cause plasma endothelin levels to rise.[21]
Cigarette smoking contains carbon monoxide which has affinity towards the hemoglobin and forms carboxy hemoglobin. Due to low oxygen carrying capacity of hemoglobin ischemia produce in renal glomeruli and basement membrane.[22] This minor damage likely to cause microproteinuria. Studies have demonstrated that stable compounds present in cigarette smoke produce endothelial dysfunction[22] by increasing the vascular production of reactive oxygen species (ROS).[23]
Conclusion
There is 99.9% significant (p < 0.0001) higher microproteinuria in chronic smokers in compare to control group, it is an early indicator of renal diseases. There were not any significant changes in other renal function parameters like serum creatinine level, blood urea and creatinine clearance test etc in both groups. It remains within normal range. Chronic smokers have a chance to develop renal impairment in long time addiction of tobacco smoking.
References
- Halimi JM , Mimran A. Renal effects of smoking: potential mechanisms and perspectives. Nephrol. Dial. Transplant. 2000;15 (7): 938-940.
- Boyle P: Cancer, cigarette smoking and premature death in Europe: A review including the Recommendations of European Cancer Experts Consensus Meeting, Helsinki, October 1996. Lung Cancer 17: 1–60, 1997
- Orth SR, Ritz E, Schrier RW. The renal risk of smoking. kidney Int.1997; 51: 1669-77.
- Olivarius, NF, Andreasen, AH, Keiding, N, Mogensen, CE: Epidemiology of renal involvement in newly diagnosed middle-aged and elderly diabetic patients: Crosssectional data from the population-based study "Diabetes Care in General Practice," Denmark. Diabetologia 1993 36:1007–1016
- Chapman, AB, Johnson, AM, Gabow, PA, Schrier, RW: Overt proteinuria and microalbuminuria in autosomal dominant polycystic kidney disease. J Am Soc Nephrol 1994 5:1349–1354,
- Walanabe N, Kamad S, Ohkubo A, Yamanake M, Oshawa S. Clin. Chem. 1986;32: 1551
- Barters M, Bohmer M. Clin. Chem. Aeta. 1972;37:193
- Ferrier D, Harvey R. Lippincotts illustrated review biochemistry. 5th ed. Walters Kluwer: Lippincott Williams and Wilkins; 2011
- Harper H. illustrated Biochemistry. 26 th ed. Lange; 2003
- Winocur PH, Miher JH,Laher MF, Alberti KG. Microalbuminuria and associated cardiovascular risk factor in community. Arterioscle Thromb Vasc Biol 1993:71- 81
- Sleight P. Smoking and hypertension.Clin Exp Hypertens. 1993;15(6):1181-92.
- Bruno G, Cavallo‐Perin P, Bargero G et al. Prevalence and risk factors for micro‐ and macroalbuminuria in an Italian population‐based cohort of NIDDM subjects. Diabetes Care1996;19: 43–47
- Halimi JM, Philippon C, Mimran A. Contrasting renal effects of nicotine in smokers and non‐smokers. Nephrol Dial Transplant 1998;13: 940–944
- Ritz E, Benck U, Frank E etal. Effect of smoking on renal hemodynamics in healthy volunteers and in patients with glomerular deseases. Jn Am Soc Nephrol 1998;9:1798-804
- Gambaro G, Verlato F, Budacovic A etal. Renal impairments in chronic smokers. Jn Am Soc Nephrol 1998; 9:562-67
- Hosteller TH, Olsom JL, Rennke HG etal. Hyperfilteration in lemnant nephrons: A potentially adverse response to renal ablation. Am Jn Physiol. 1981;241: 85- 93
- Remuzzi G. Cigarette smoking and renal function impairment. Am Jn Kidney Disorder. 1999;33:807-813
- Cerami C, Founders H, Nicholl I. Tobacco smoke is a source of toxic reactive glycation products. Proc Natl Acad Sci USA 1997;94: 915-920
- Esposito C, Gerlach H, Brett J etal. Endothelin receptor mediated binding of glucose modified albumin is associated with increased monolayer permeability and modulation of cell surface coagulant properties. Jn Exp Med. 1989;170:1387-1407.
- Viassara H, Fuh H, Makita Z etal. Exogenous advanced glycosylation end product induces complex vascular dysfunction in normal animal: A model of diabetic and ageing complication. Proc Natl Acad Sci USA.1992;89:120-43.
- Haack T, Jungmann E, Raab C, Usadel KH. Elevated endothelin‐1 levels after cigarette smoking. Metabolism 1994;43:267–69
- Mühlhauser I, Verhasselt R, Sawicki PT etal. Leucocyte count, proteinuria and smoking in type 1 diabetes mellitus. Acta Diabetologica. 1993;30(2):105-07
- Jaimes EA, DeMaster EG, Tian RX, Raij L. Stable compounds of cigarette smoke induce endothelial superoxide anion production via NADPH oxidase activation. Arterioscle Thromb Vasc Biol 2004;24: 1031- 1036