Original Article - Current Pediatric Research (2023) Volume 27, Issue 8
Meta-analysis on prevalence of pediatric community acquired pneumonia in India.
Vidhi Arora, Sangeeta Choudhary, Manita Bambha*
Department of Pediatrics, Kalpana Chawla Government Medical College, Karnal, Haryana, India
- Corresponding Author:
- Manita Bambha
Department of Pediatrics,
Kalpana Chawla Government Medical College,
Karnal, Haryana,
India
E-mail: rinky.nikky@gmail.com
Received: 07-Apr-2023, Manuscript No. AAJCP-23-94639; Editor assigned: 10-Apr-2023, AAJCP-23-94639 (PQ); Reviewed: 24-Apr-2023, QC No. AAJCP-23-94639; Revised: 01-Aug-2023, Manuscript No. AAJCP-23-94639 (R); Published: 08-Aug-2023, DOI:10.35841/0971-9032.27.8.1976-1981
Abstract
Introduction: A severe inflammation of the parenchymal tissue of the lungs is known as pneumonia. According to the location of acquisition, it can be categorized as community or hospital acquired; according to the etiological agents or mechanisms, it can be categorized as bacterial, viral, fungal, aspiration or ventilator associated; according to the involved lung anatomy, it can be categorized as lobar pneumonia, bronchial pneumonia or acute interstitial and according to the clinical severity, it can be categorized.
Aims and objective: To determine the pooled prevalence of Community Acquired Pneumonia (CAP) from the included studies.
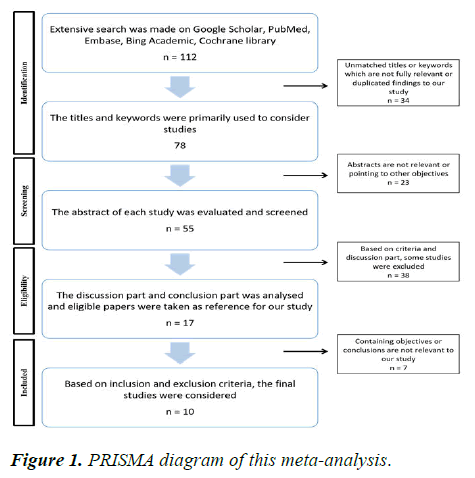
Methods: The literature search was made by using MeSH keywords from Science Direct, Google Scholar, Cochrane library, PubMed and Scopus. PRISMA diagram has been represented to show the steps of inclusion of studies. The statistical analysis has been done by Meta XL for the effective determination of pooled prevalence.
Results: The meta-analysis showed the detailed statistical findings of the included studies and p=.000 implies that the pooled prevalence by fixed effect and random effects is significant in the population.
Conclusion: The meta-analysis has concluded that the prevalence of CAP among the pediatric population in India is significant and this finding would help clinicians to make an early diagnosis of CAP by effective tests for the suspected individuals.
Keywords
CAP, Pneumonia, Prevalence, Diagnosis, Ventilator
Introduction
Pneumonia is a severe inflammation of the lungs’ parenchymal tissue. According to the place of acquisition, it can be classified as community or hospital acquired; according to the etiological agents or mechanisms, it can be classified as bacterial, viral, fungal, aspiration or ventilator associated; according to the lung anatomy involved, it can be classified as lobar pneumonia, bronchial pneumonia or acute interstitial and according to the clinical severity, it can be classified as “no pneumonia,” “pneumonia” or “very severe pneumonia” [1-3].
Children under the age of five are more likely to develop pneumonia, which continues to be the leading cause of morbidity and mortality in this age group [4]. A global estimate from 2000 states that pneumonia affects more than 156 million children under the age of five every year, 151 million of whom live in developing countries, and causes roughly 1.2 million fatalities. South-east Asia and Africa were the two continents with the highest frequency of pediatric pneumonia, with an estimated 61 million and 35 million cases of pneumonia in children under the age of five per year, respectively [5]. Pneumonia affected 102 million children under the age of five globally in 2015, down from 120 million in 2010 (with 0.88 million deaths). These decreases were a result of a lessening of the severity of the primary risk factors, enhanced socioeconomic development and preventive measures, improved access to care and higher hospital care standards. Despite these developments, pneumonia remains a significant public health issue for children, particularly in developing countries.
Numerous investigations have been conducted across the globe to identify pneumonia risk factors. Despite the conflicting findings, low birth weight, malnutrition, indoor air pollution, parental smoking, lack of immunizations, crowding, a shared kitchen, not exclusively breastfeeding and maternal education were discovered to be risk factors for pneumonia in children under the age of five [6-9].
Community Acquired Pneumonia (CAP) is a common infectious disease throughout the world. The illness has a significant impact on healthcare in poor countries like India. India alone is responsible for around one-fourth of the global burden of pneumonia, with a Case Fatality Rate (CFR) of 14%-30% [10]. Due to the significant effects that comorbidities and risk factors have on the incidence, complications, mortality and management of CAP, clinicians face significant challenges. A European study found that the incidence of CAP is increased by two to four times by concurrent diseases such as dementia, cerebrovascular disease, HIV, chronic renal and liver disease and chronic respiratory and cardiovascular problems. Alcoholism and smoking were also identified as common risk factors for the disease in the same analysis [11].
Similar investigations out in the US identified ageing as a common risk factor for increased incidence and related death [12,13]. In India, the concomitant illnesses and risk factors connected to a higher risk of CAP are not well-known. Although a few studies have reported these findings, the evidence is scattered and there isn’t a complete study accessible right now. Before our study, the risk factors and concomitant diseases that increase the risk of CAP in the Indian population had never been in-depth evaluated and analyzed. The results of this study would help physicians implement particular risk reduction measures to minimize the burden of CAP disease on the country [14].
MaterialsandMethods
Search strategy
The literature search was made by using MeSH keywords from Science Direct, Google Scholar, Cochrane library, PubMed and Scopus. The search terms used included (prevalence) and (pediatric or children) and (community acquired or community) and (pneumonia or lung infection). An independent search was made by using the combination of terms (prevalence and CAP or community acquired pneumonia or pneumonia). The search was made from 2005 to 2023 on the prevalence of CAP in pediatric population [15-17].
Data extraction
The study found 10 eligible studies for final inclusion. The search was made and likely studies were sorted. The unmatched titles, unmatched keywords and duplicated studies were excluded to obtain 78 studies. Irrelevant abstracts and studies with unmatched objectives were excluded. Based on the discussion and conclusion, this meta-analysis finally included 10 studies and they are summarized in Table 1. Figure 1 shows the PRISMA diagram of the inclusion steps [18].
Inclusion and exclusion criteria
This meta-analysis included those studies that are being conducted in India with the Indian population between 2005 and 2023 on the pediatric population. Studies including suspected individuals with pneumonia were considered for this analysis.
The studies which contain the non-Indian population or adult population were excluded. Again, the studies on pediatric pneumonia prevalence which covered types of pneumonia other than community-acquired were also excluded.
Statistical analysis
This analysis used Meta XL for effective analysis. It was done both by using fixed effects and random effects. Funnel plot and statistical findings were calculated using Meta XL. I2, Cochran's Q and X2 with p-value were also determined.
Results
The meta-analysis has listed the included studies in Table 1 with number of subjects and their respective CAP patients.
| Name of the authors | Type of study | Age | Number of patients | Patients with CAP | Percentage |
|---|---|---|---|---|---|
| Pernica JM, et al. 2021 | Prospective study | <5 years | 281 | 208 | 74.02 |
| Greenberg D, et al. 2014 | RCT | <5 years | 115 | 25 | 21.74 |
| Moses JM, et al. 2009 | Retrospective | 5.5 months to 20 years | 62 | 12 | 19.35 |
| Meyer Sauteur PM, et al. 2020 | Prospective cohort | 3 years to 18 years | 63 | 29 | 46.03 |
| Mathew JL, et al. 2015 | Prospective study | <12 months | 2345 | 1145 | 48.83 |
| Shah AS, et al. 2009 | Retrospective | <5 years | 1,50,945 | 967 | 0.64 |
| Spuesens EBM, et al. 2013 | Prospective study | 3 months to 16 years | 726 | 321 | 44.21 |
| Lin LJ, et al. 2020 | Prospective study | <5 years | 61 | 56 | 91.8 |
| Kumar S, et al. 2019 | Prospective study | 1 month to 5 years | 75 | 26 | 34.67 |
| Gowraiah V, et al. 2014 | Prospective observational study | <5 years | 516 | 185 | 35.85 |
Table 1. The final studies that is included in this meta-analysis.
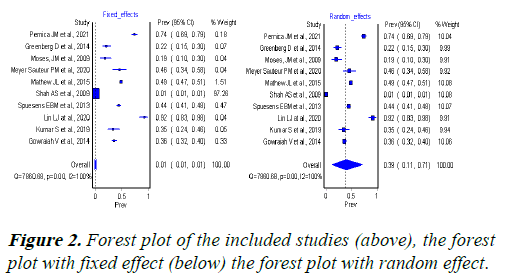
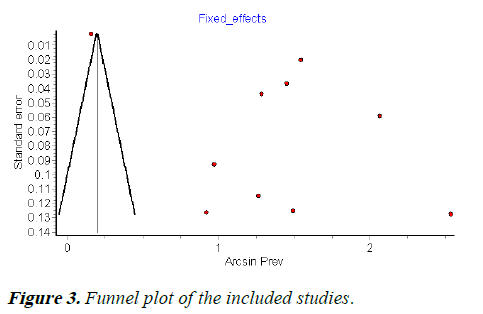
Figures 2 and 3 respectively show the funnel plots of the included studies.
Tables 2 and 3 show the detailed statistical findings of the included studies and p=.000 implies that the pooled prevalence by fixed effect and random effects is significant in the population.
| Study | Prevalence | LCI 95% | HCI 95% | Weight (%) |
|---|---|---|---|---|
| Pernica JM et al., 2021 | 0.740213523131673 | 0.687229365267613 | 0.789920156798124 | 0.181385878320038 |
| Greenberg D et al., 2014 | 0.217391304347826 | 0.146343022655727 | 0.297838102235736 | 0.0744229802698558 |
| Moses, JM et al., 2009 | 0.193548387096774 | 0.10360710667629 | 0.302341419874906 | 0.0402721754707012 |
| Meyer Sauteur PM et al., 2020 | 0.46031746031746 | 0.338251336627928 | 0.584783288924308 | 0.0409165302782324 |
| Mathew JL et al., 2015 | 0.488272921108742 | 0.468050118640595 | 0.508514929699144 | 1.51133420106447 |
| Shah AS et al., 2009 | 0.00640630693298884 | 0.00601000293653348 | 0.00681517254593728 | 97.2624586002036 |
| Spuesens EBM et al., 2013 | 0.442148760330579 | 0.406169368973588 | 0.478434023405664 | 0.468123767671431 |
| Lin LJ at al., 2020 | 0.918032786885246 | 0.833674357978926 | 0.97605364882475 | 0.03962782066317 |
| Kumar S et al., 2019 | 0.346666666666667 | 0.242583384534425 | 0.458549344699055 | 0.048648787968607 |
| Gowraiah V et al., 2014 | 0.358527131782946 | 0.317659258495953 | 0.400447095571728 | 0.332809258089875 |
| Pooled | 0.00971267640846202 | 0.00923073109698858 | 0.010206757594006 | 100 |
| Statistics | ||||
| I2 | 99.8855060997628 | 99.8722615912419 | 99.8973773564351 | |
| Cochran's Q | 7860.6807710753 | |||
| X2, p | 0.000 | |||
Table 2. Main statistical findings of the study (fixed effect).
| Study | Prevalence | LCI 95% | HCI 95% | Weight (%) | |
|---|---|---|---|---|---|
| Pernica JM et al., 2021 | 0.740213523131673 | 0.687229365267613 | 0.789920156798124 | 0.181385878320038 | |
| Greenberg D et al., 2014 | 0.217391304347826 | 0.146343022655727 | 0.297838102235736 | 0.0744229802698558 | |
| Moses, JM et al., 2009 | 0.193548387096774 | 0.10360710667629 | 0.302341419874906 | 0.0402721754707012 | |
| Meyer Sauteur PM et al., 2020 | 0.46031746031746 | 0.338251336627928 | 0.584783288924308 | 0.0409165302782324 | |
| Mathew JL et al., 2015 | 0.488272921108742 | 0.468050118640595 | 0.508514929699144 | 1.51133420106447 | |
| Shah AS et al., 2009 | 0.00640630693298884 | 0.00601000293653348 | 0.00681517254593728 | 97.2624586002036 | |
| Spuesens EBM et al., 2013 | 0.442148760330579 | 0.406169368973588 | 0.478434023405664 | 0.468123767671431 | |
| Lin LJ at al., 2020 | 0.918032786885246 | 0.833674357978926 | 0.97605364882475 | 0.03962782066317 | |
| Kumar S et al., 2019 | 0.346666666666667 | 0.242583384534425 | 0.458549344699055 | 0.048648787968607 | |
| Gowraiah V et al., 2014 | 0.358527131782946 | 0.317659258495953 | 0.400447095571728 | 0.332809258089875 | |
| Pooled | 0.00971267640846202 | 0.00923073109698858 | 0.010206757594006 | 100 | |
| Statistics | |||||
| I2 | 99.8855060997628 | 99.8722615912419 | 99.8973773564351 | ||
| Cochran's Q | 7860.6807710753 | ||||
| X2, p | 0.000 | ||||
Table 3. Main statistical findings of the study (random effect).
Discussion
The incidence, mortality, complications and management of community acquired pneumonia problems and treatment results are significantly impacted by comorbidities and risk factors. A study uses a systematic review and meta-analysis to try to find the same in the Indian population. According to the study’s findings, the Indian population was particularly vulnerable to community acquired pneumonia due to comorbid illnesses like hypertension, chronic obstructive pulmonary disease and diabetes mellitus as well as variables like advanced age and a history of smoking [19-22].
An acute inflammation of the parenchymal tissue of the lungs is known as pneumonia. It is a significant issue for public health and the main cause of sickness and mortality in children under five, particularly in underdeveloped nations. According to estimates, there were 102 million episodes of pneumonia in children under the age of five in 2015 and 0.7 million of those instances resulted in fatalities. Pneumonia’s prevalence in eastern Africa was revealed by many primary investigations. However, there was a discrepancy between those investigations and no study was done to report the combined magnitude and related factors. To determine the national prevalence of pneumonia and its contributing factors in Eastern Africa, a review was conducted. According to the report, pneumonia is still widely prevalent in Eastern Africa. Policymakers and program managers will benefit from the review as they develop strategies to avoid pneumonia.
Approximately two million children under the age of five die from pneumonia each year, accounting for approximately one in five child fatalities worldwide. To accomplish MDG4 in poor countries, it is essential to pinpoint its prevalence in children under the age of five and the contributing variables [23]. An earlier study’s major goal was to determine the prevalence and risk factors for pneumonia in children under the age of five in Este town and the nearby rural kebeles in northwest Ethiopia. Pneumonia prevalence in children under the age of five over the past two weeks was 16.6% overall. The most significant factors related to pneumonia in children under five were stunting, living in a crowded house, carrying the child on the back while cooking, using charcoal for cooking, and having cattle inside the main home according to the study. According to the study, pneumonia was common among children under five in the study area [24].
One-third of the overall WHO South East Asia burden of under-five mortality is borne by India. Epidemiological studies revealing the true burden of pneumonia are few and far between. The ability to successfully design and implement preventative actions for pneumonia reduction will be aided by the identification of the risk factors connected with the disease [25]. The findings of a study revealed that it was linked to partial immunization rather than any of the home environment characteristics. Mothers were found to have poor feeding habits, poor knowledge of the signs and symptoms of pneumonia and poor hand hygiene. According to the study’s findings, Maharashtra’s Pune and Sangli districts had exceptionally low rates of pneumonia. The most significant risk factor was discovered to be partial vaccination. A higher literacy rate among mothers and higher immunization coverage may be contributing reasons to the low incidence of pneumonia and its lack of connection with established risk factors [26].
To determine the prevalence of Community Acquired Pneumonia (CAP) in children (2-59 months) in four areas of Northern India, a prospective study was conducted. According to the study’s findings, CAP incidence was nearly five to 10 times greater in new-borns (2-11 months) than in people aged 12-59 months. According to the report, there is a high frequency of CAP in Uttar Pradesh and Bihar, with new-born rates being significantly higher. Therefore, it is necessary to implement preventative measures, enhance health seeking behaviour and improve the standard of care for CAP [27,28].
Conclusion
The meta-analysis has concluded that the prevalence of CAP among the pediatric population in India is significant and this finding would help clinicians to make an early diagnosis of CAP by effective tests for the suspected individuals. This meta-analysis showed a very specific prevalence among the Indian pediatric population. Although this meta-analysis has included a smaller number of studies, the specification of each study met the eligibility criteria, due to which, the specific finding and conclusion could be obtained. However, it can be highlighted that there is a lack of original studies on CAP among the Indian pediatric population. The authors suggest conducting more survey based studies all over India to bring out the larger picture of CAP prevalence in the varied population. However, this meta-analysis has successfully highlighted the detailed statistical metrics of CAP and the epidemiological status of CAP in India among the pediatric population suggesting we conduct more studies on management in coming years.
References
- Mackenzie G. The definition and classification of pneumonia. Pneumonia. 2016;8(1):14.
[Crossref] [Google Scholar] [PubMed]
- WHO. Revised WHO classification and treatment of childhood pneumonia at health facilities. World Health Organization. 2014.
- Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital acquired and ventilator associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of America and the American thoracic society. Clin Infect Dis. 2016;63(5):e61-111.
[Crossref] [Google Scholar] [PubMed]
- McAllister DA, Liu L, Shi T, et al. Global, regional and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: A systematic analysis. Lancet Glob Health. 2019;7(1):e47-57.
[Crossref] [Google Scholar] [PubMed]
- Rudan I, Boschi-Pinto C, Biloglav Z, et al. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(5):408-16.
[Crossref] [Google Scholar] [PubMed]
- Ramezani M, Aemmi SZ, Emami MZ. Factors affecting the rate of pediatric pneumonia in developing countries: A review and literature study. Int J Pediatr. 2015;3(6):1173-81.
- Hemagiri K, Sameena A, Aravind K, et al. Risk factors for severe pneumonia in under five children-a hospital based study. Int J Res Health Sci. 2014;2(1):47-57.
- Htar MTT, Stuurman AL, Ferreira G, et al. Effectiveness of pneumococcal vaccines in preventing pneumonia in adults, a systematic review and meta-analyses of observational studies. PLoS One. 2017;12(5):e0177985.
[Crossref] [Google Scholar] [PubMed]
- Nirmolia N, Mahanta TG, Boruah M, et al. Prevalence and risk factors of pneumonia in under five children living in slums of Dibrugarh town. Clin Epidemiol Glob Health. 2018;6(1):1-4.
- Eshwara VK, Mukhopadhyay C, Rello J. Community acquired bacterial pneumonia in adults: An update. Indian J Med Res. 2020;151(4):287-302.
[Crossref] [Google Scholar] [PubMed]
- Torres A, Peetermans WE, Viegi G, et al. Risk factors for community acquired pneumonia in adults in Europe: A literature review. Thorax. 2013;68(11):1057-65.
[Crossref] [Google Scholar] [PubMed]
- Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community acquired pneumonia in seniors: Results of a population based study. Clin Infect Dis. 2004;39(11): 1642-50.
[Crossref] [Google Scholar] [PubMed]
- Buzzo AR, Roberts C, Mollinedo LG, et al. Morbidity and mortality of pneumonia in adults in six Latin American countries. Int J Infect Dis. 2013;17(9):e673-7.
[Crossref] [Google Scholar] [PubMed]
- Pernica JM, Harman S, Kam AJ, et al. Short course antimicrobial therapy for pediatric community acquired pneumonia: The SAFER randomized clinical trial. JAMA Pediatr. 2021;175(5):475-82.
[Crossref] [Google Scholar] [PubMed]
- Greenberg D, Givon-Lavi N, Sadaka Y, et al. Short course antibiotic treatment for community acquired alveolar pneumonia in ambulatory children: A double blind, randomized, placebo controlled trial. Pediatr Infect Dis J. 2014;33(2):136-42.
[Crossref] [Google Scholar] [PubMed]
- Moses JM, Alexander JL, Agus MS. The correlation and level of agreement between end tidal and blood gas pCO2 in children with respiratory distress: A retrospective analysis. BMC Pediatr. 2009;9:20
[Crossref] [Google Scholar] [PubMed]
- Meyer Sauteur PM, Krautter S, Ambroggio L, et al. Improved diagnostics help to identify clinical features and biomarkers that predict Mycoplasma pneumoniae community acquired pneumonia in children. Clin Infect Dis. 2020;71(7):1645-54.
[Crossref] [Google Scholar] [PubMed]
- Mathew JL, Singhi S, Ray P, et al. Etiology of community acquired pneumonia among children in India: Prospective, cohort study. J Glob Health. 2015;5(2):050418.
[Crossref] [Google Scholar] [PubMed]
- Shah AS, Nisarga R, Ravi Kumar KL, et al. Establishment of population based surveillance for invasive pneumococcal disease in Bangalore, India. Indian J Med Sci. 2009;63(11):498-507.
[Google Scholar] [PubMed]
- Spuesens EBM, Fraaij PLA, Visser EG, et al. Carriage of Mycoplasma pneumoniae in the upper respiratory tract of symptomatic and asymptomatic children: An observational study. PLoS Med. 2013;10(5):e1001444.
[Crossref] [Google Scholar] [PubMed]
- Lin LJ, Chang FC, Chi H, et al. The diagnostic value of serological studies in pediatric patients with acute Mycoplasma pneumoniae infection. J Microbiol Immunol Infect. 2020;53(2):351-6.
[Crossref] [Google Scholar] [PubMed]
- Kumar S, Chakravarti A, Kumar S, et al. Detection of respiratory syncytial virus and Mycoplasma pneumoniae in paediatric lower respiratory tract infections. Indian J Med Res. 2019;150(3):306-9.
[Crossref] [Google Scholar] [PubMed]
- Gowraiah V, Awasthi S, Kapoor R. Can we distinguish pneumonia from wheezy diseases in tachypnoeic children under low resource conditions? A prospective observational study in four Indian hospitals. Arch Dis Child. 2014;99(10):899-906.
[Crossref] [Google Scholar] [PubMed]
- Ghia CJ, Rambhad GS. Systematic review and meta-analysis of comorbidities and associated risk factors in Indian patients of community acquired pneumonia. SAGE Open Med. 2022;10.
[Crossref] [Google Scholar] [PubMed]
- Beletew B, Bimerew M, Mengesha A, et al. Prevalence of pneumonia and its associated factors among under-five children in East Africa: A systematic review and meta-analysis. BMC Pediatr. (2020);20(1):1-13.
- Abeje Fekadu G. Prevalence of pneumonia among under-five children in Este town and the surrounding rural Kebeles, Northwest Ethiopia; A community based cross sectional study. Sci J Pub Health. (2014);2(3):150.
- Gothankar J, Doke P, Dhumale G, et al. Reported incidence and risk factors of childhood pneumonia in India: A community-based cross-sectional study. BMC Pub Health. (2018);18(1).
- Awasthi S, Pandey CM, Verma T, et al. Incidence of community acquired pneumonia in children aged 2-59 months of age in Uttar Pradesh and Bihar, India, in 2016: An indirect estimation. PLoS ONE. (2018);14(3).