Case Report - Journal of Clinical Dentistry and Oral Health (2023) Volume 7, Issue 2
Management of invasive cervical resorption with Biodentine and fiber post using gutta percha for initial canal preservation: A case report
Geo TD1*, Saurabh Gupta1, Nilima Pagare1, Harsh Chansoria21Department of Conservative Dentistry and Endodontics, Government College of Dentistry, Madhya Pradesh, India
2Department of Prosthodontics and Crown & bridge, Government College of Dentistry, Madhya Pradesh, India
- *Corresponding Author:
- Geo TD
Department of Conservative Dentistry and Endodontics
Government College of Dentistry
Madhya Pradesh, India
E-mail: drgeotd@gmail.com
Received: 01-Feb-2023, Manuscript No. AACDOH-23-88921; Editor assigned: 03-Feb-2023, PreQC No. AACDOH-23-88921(PQ); Reviewed: 17-Feb-2023, QC No. AACDOH-23-88921; Revised: 25-Feb-2023, Manuscript No. AACDOH-23-88921(R); Published: 02-Mar-2023, DOI:10.35841/aacdoh-7.2.139
Citation: Geo TD. Management of invasive cervical resorption with biodentine and fiber post using gutta percha for initial canal preservation: A case report. J Clin Dentistry Oral Health. 2023;7(2):139
Abstract
Tooth resorption can be internal or external. Invasive Cervical Resorption (ICR) is an inflammatory external resorption, which shows clinical and two-dimensional radio graphically resemblance to internal resorption. ICR is defined as “a localized resorptive process that commences on the surface of the root below the epithelial attachment and above the coronal aspect of the supporting alveolar process, namely, the zone of the connective tissue attachment. The present clinical case report describes the surgical management of invasive external cervical resorption with bioactive restorative material; Biodentine, along with reinforcement of weakened crown by fiber post in relation to upper right central incisor using gutta percha as a temporary material for initial canal preservation.
Keywords
Invasive cervical resorption, External cervical resorption, Internal resorption, Biodentine.
Introduction
Root resorption is one of the most common sequelae of dental trauma. It can also be due to irritation or injury to the periodontal ligament or tooth pulp. Various effector cells and molecules are involved in the process of root resorption; osteoclast like odontoclast cells, fibroblast, matrix metalloproteinase is some of them [1]. Root resorption in deciduous dentition can be considered as physiological process but the resorption in permanent dentition is always because of a pathological reason and in untreated cases it may leads to eventual tooth loss. But at the same time resorption defects are challenging and complicated to diagnose correctly which may end up in inappropriate treatment being carried out [2]. An early and accurate diagnosis followed by appropriate management with bioactive restorative material could give favorable result.
External and internal resorptions are the two important kinds tooth resorption. Radiographically internal resorption resembles ‘ballooning out’ smooth well defined radiolucency in the root canal with intact mesial and distal borders of the root [2].The radiographic appearance of external resorptions varies according to the severity and location of the lesion, beginning from cloudy radiolucency with ill-defined margins and un-interfered root canal walls which is passing through the defect, till complete loss of the tooth structure [3]. Generally external resorptions are four types; external surface resorption, external inflammatory root resorption, replacement resorption, and ankylosis. Invasive Cervical Resorption (ICR) is a type of external inflammatory root resorption [4].
Invasive cervical resorption is a different entity, which shows clinical and two dimensional radiographs resemblance to internal resorption. It is defined as “a localized resorptive process that commences on the surface of the root below the epithelial attachment and above the coronal aspect of the supporting alveolar process, namely the zone of the connective tissue attachment” [5]. Pinkish color might be associated with the crown of resorbed tooth because of dentine replaced with fibro-vascular tissue under the thin shelter of enamel. The lesions are usually asymptomatic and identified accidently in routine radiographic examination but sometimes clinical examination reveals proliferative tissue, which occupies the resorption defect and very rarely patient complaints of bleeding from the inflamed tissue related to involved tooth. There is progressive loss of cementum, dentin, and enamel with replacement by fibro-vascular tissue derived from the periodontal ligament with sometimes deposition of cementum-like hard tissue. Secondary infections could lead to inflammation and swelling [6].
Subgingival probing is a reliable indication and sensibility test gives a positive vitality test result because of the presence of neuro-vascular tissue within the root canal. An Intra oral peri apical radiograph gives uniform radiolucency, having a smooth, regular outline. However, a nonuniform preferential spread is also possible and may result from extensions of resorptive tissue extending in different directions, often with little lateral spread from the site of initiation. The resorption may also involve adjacent alveolar bone, simulating an intrabony defect [7]. However, intraoral radiographs do not provide an indication of the true dimensions of such lesion. The resorption defect may spread within the root in all directions, this may not be reflected in the size and position of the radiolucency detected on the radiograph. Intraoral radiographs only reveal limited diagnostic information in diagnosing external root resorptions [8]. CBCT is effective and reliable in detecting the presence of resorption lesions and its superior diagnostic accuracy results in an increased likelihood of correct management of resorption lesions [2].
Because of the recent advancements in restorative dentistry; the management of root resorption could give hopeful outcome. Calcium hydroxide, glass ionomer cements, resin modified glass ionomer cement, mineral trioxide aggregate are some of the material commonly using for the management of resorption. Biodentine is a restorative material with proven bioactive property; which can also be used for the management of resorptive lesions.
Case report
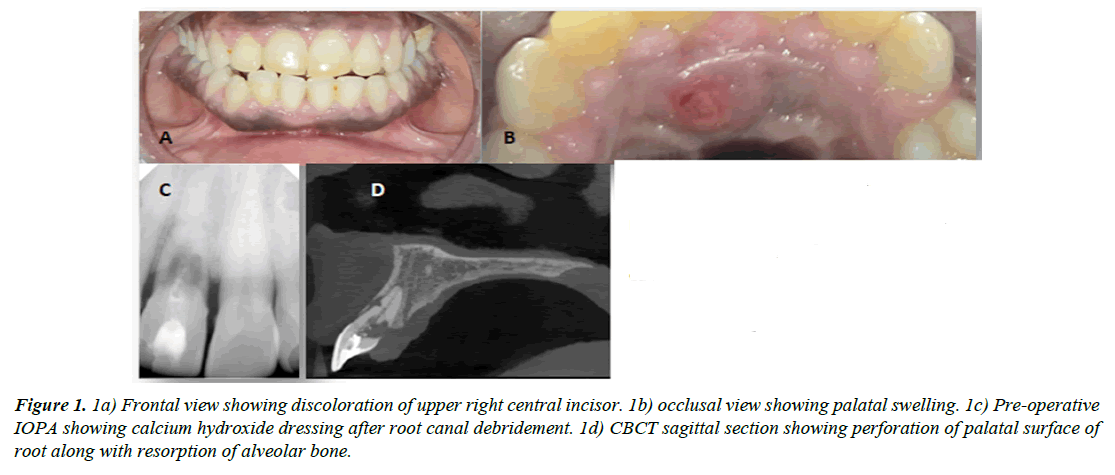
A 45-year-old male patient presented to the Department of Conservative Dentistry and Endodontics with a localized swelling, bleeding gums, pus drainage and yellow discolouration of maxillary right central incisor. The patient had noticed the color change over a period of 6-7 years and recurring swelling for the past 1 year. And now the patient felt that the lesion had increased in size (Figure 1A). There was no known history of trauma, orthodontic treatment, or bleaching.
Figure 1: 1a) Frontal view showing discoloration of upper right central incisor. 1b) occlusal view showing palatal swelling. 1c) Pre-operative IOPA showing calcium hydroxide dressing after root canal debridement. 1d) CBCT sagittal section showing perforation of palatal surface of root along with resorption of alveolar bone.
The patient has been under medication for hypertension for the past 10 years, and this was the patient’s second dental visit. The patient informed that one year ago he visited a dentist because of pain, was prescribed antibiotics and analgesics for five days and the symptoms got subsided. One month ago the pain and swelling again started to progress continuously.
He had moderate oral hygiene and generalized hyperplastic gingiva along with swelling on the palatal surface of tooth 11 (tooth numbering according to FDI system). The marginal gingiva of right central incisor was slightly erythematous. The crown showed a yellowish-brown discoloration in the cervical and middle third of labial surface. The tooth was unresponsive to thermal and electric vitality tests and was tender to percussion. Periodontal probing revealed pocket depths of 5 mm at the palatal gingival sulcus. A periapical radiograph revealed an irregular but well demarcated area of radiolucency at the Cemento Enamel Junction (CEJ) encompassing coronal third of root. The pulp canal and chamber spaces were well defined, ballooned-out and asymmetric with the adjacent central incisor. There was no interdental bone loss, the lamina dura was intact, and the periodontal ligament space was slightly increased in the apical area (Figure 1B). A provisional diagnosis of external root resorption associated with 11 was made.
Early Management
As an emergency procedure, access opening was done. Continuous fresh bleeding from the canal lead to suspicion of perforation. So calcium hydroxide was given as an intracanal medicament, along with the temporary restoration of the access cavity and the patient advised for CBCT in relation to concerned tooth.
Sagittal section of CBCT revealed perforation at the coronal third of root, extending apically along with resorption of palatal bone (Figure 1C) One another external resorptive lesion also evident at the junction of middle and apical third of root approaching the root canal (Figure 1D). Diagnosis confirmed as Heithersay’s invasive cervical resorption Class IV.
Late Management
Working length determined by apex locator and peri-apical radiograph. Root canal debridement was done with smaller diameter hand files to avoid further weakening of tooth structure. Apical preparation of the canal was done with 2%, number 40 hands K-file (Mani, Inc.8-3 Kiyohara Industrial Park Utsunomiya, Tochigi 321-3231 Japan). Calcium hydroxide dressing was given as an intermediate intra-canal medicament. The access cavity was temporary filled with Cavit (3 MESPE, St Paul, MN, USA). After one week the patient was recalled for surgical repair of external cervical resorption.
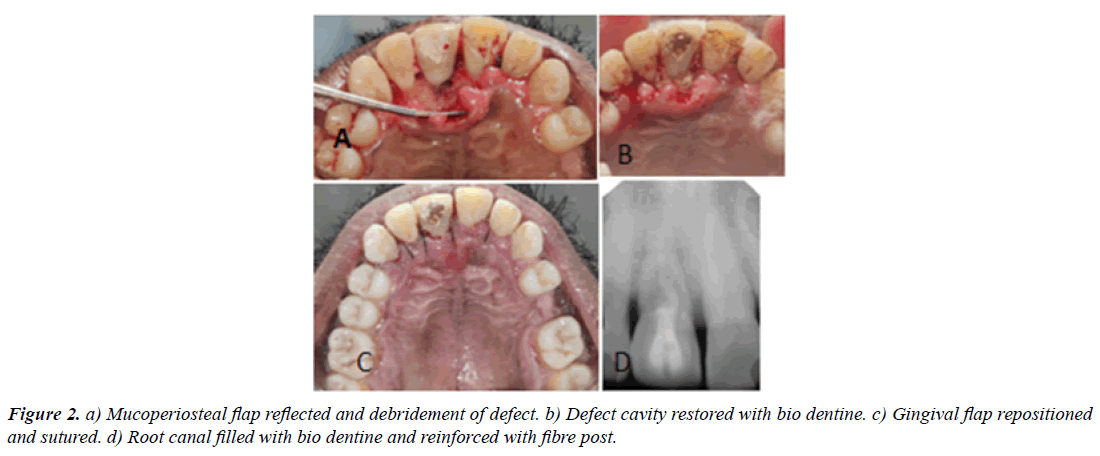
For periodontal surgery, initially, local anesthesia was administered in the maxillary anterior region and intra sulcular incisions were made on the palatal regions involving canine regions on either side. The mucoperiosteal flaps were elevated which allowed the visualization of the defect (Figure 2A). For the complete removal of granulation tissue, small amount of palatal alveolar bone removed using slow speed micro motor. Complete debridement of the resorptive area performed with curette and ultrasonic instrument. Probing of the resorption lacunae showed hardened walls. It was decided to restore the cavity with the Biodentine (Septodont, St. Maur. des. Fosses, France).
A 2% number 40 gutta percha cones (Dentsply, Maillefer, Tulsa, OK, USA) placed in the root canal to prevent the blockage of the canal by restorative material. Biodentine was placed inside the cavity, contoured and allowed to set (Figure 2B). After this the gingival flap was repositioned and sutured (Figure 2C). Gutta percha cone was later removed from the canal and the access cavity sealed with temporary restorative material. The patient was instructed on oral hygiene practices including mouthwash twice a day with chlorhexidine solution 0.12% and was prescribed antibiotic therapy amoxicillin 500 mg, thrice a day, for seven days. After one week sutures were removed.
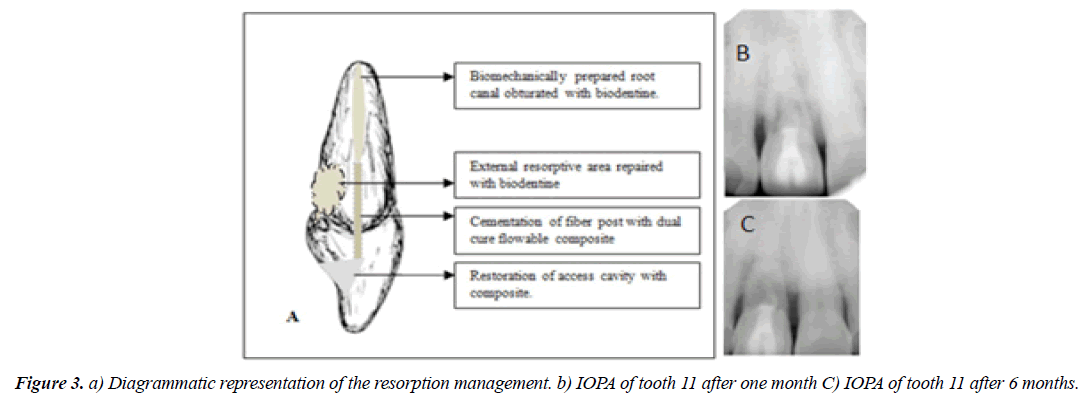
On the next visit biomechanical preparation of the root canal completed with 2% tapered K-files and irrigant used was 5.25% sodium hypochlorite. The root canal filled with Biodentine up to middle third of root canal and a glass fiber post (Mailyard fiber post, India) cemented with flowable dual cure resin cement( Fusion core DC flo, Prevest DenPro, USA) to strengthen the weakened crown structure (Figure 2D). The access cavity restored with composite (Kulzer Charisma smart composite, Heraeus Kulzer, USA). Diagrammatic representation is given in (Figure 3A). Post-operative intra oral peri apical radiograph took to confirm the adequate sealing of the resorptive defect.
Follow-up
At 6 months follow up the patient was completely asymptomatic. Periodontal status of the tooth 11 was good and periodontal probing depth was within normal limits. The peri apical radiograph of the tooth showed maintained adequate sealing of the resorptive defect with stable intra radicular bone height and no changes in peri apical osseous tissue (Figure 3B). There was no further progression of the resorptive lesion.
Discussion
Root resorption is common sequelae of dental trauma, but most of the times resorption lesions are left unidentified because of the absence of clinical symptoms. In the current case the patient complained of pain and swelling associated with the tooth. Super infection of inflamed connective tissue in resorptive area may be the reason for continuous pain and swelling. The infectious inflammation process associated with the production and release of the macrophage-chemotactic factor, osteoclast-activating factor, and prostaglandins, which are known stimulators of hard tissue resorption [5]. Many times the external resorption is misdiagnosed as internal resorption due to lack of clinical evidences and limitations of two dimensional radiography. Evolution of CBCT improved the diagnosis and management of resorption by revealing the exact anatomical location, shape, size extent and severity of the lesions (Figure 3C).
Clinical findings of invasive cervical resorption sometimes may be mimicking with internal resorption, like the so called “pink tooth” which is caused by inflamed pulp tissue in the case of internal resorption and inflamed periodontal granulation tissue in case of invasive cervical resorption. In symptomatic cases of internal resorption, pulpal symptoms predominate of because the pathogenesis originates from the vital pulp tissue. If pulp succumbs completely and periradicular tissues become inflamed, symptoms of periodontitis may be seen. In cases of invasive cervical resorption, the periodontal tissues are inflamed first and may cause vague gnawing discomfort [9]. In the present case the periodontal findings are predominated, but there wasn’t pink discolouration, instead of mild yellowishbrown discolouration was there.
Generalized gingival hyperplasia of the patient was due to the side effect of antihypertensive drug, amlodipine. Thorough scaling, root planning, drug substitution or surgical interventions are the treatment of choice for such conditions. Good oral hygiene maintenance instructions were given to diminish oral bacterial load, which reduces the chances of further super infection at the surgical site and resorption repaired area. But gingival over growth impair the oral hygiene. So scaling and root planning was done before the repair of resorptive lesion and advised to use chlorhexidine 0.2% mouth wash three times per day.
Percolation of sodium hypochlorite through the perforation site of the root frequently causes injury of the soft tissues. To prevent such an accident; the perforation site needs to be repaired initially without losing the patency of root canal. Management of resorption was carried out in two phases; in first phase minimal biomechanical preparation of the root canal was carried out to prevent further weakening of tooth structure followed by gutta percha cone placed in the canal to preserve the patency and the external resorption was repaired with Biodentine by reflecting mucoperiosteal flap; and in the second phase the root canal obturation with Biodentine after removal of gutta percha along with fiber post cementation was done.
Biodentine (Septodont, Saint-Maur-des-Fosses, France) is a tricalcium silicate-based restorative material that has been introduced. Tricalcium silicate is the main ingredient of powder part of Biodentine along with minor contents of calcium carbonate and zirconium oxide. Calcium chloride in the liquid reduces the setting time [10]. Biocompatibility, bioactivity and biomineralization properties makes the Biodentine one of the most successful material in restorative field [11].Comparing and evaluating the microleakages and compressive strengths of Fuji II LC, Riva light cure, Pro- Root white Mineral Trioxide Aggregate (MTA), Biodentine , and Well-Root PT, the lowest microleakage was observed in biodentine and compressive strength of all five materials satisfied the international requirements [12]. From the available clinical evidences Biodentine might be considered as an appropriate repair material for external resorption defects. Obturation of the root canal with Biodentine might prevent further resorptive process because of its bioactive properties [13]. At the same time Biodentine shows similar compressive strength of natural dentine [14]. Biodentine along with fiber post showed enhanced fracture resistance in simulated immature roots under aging conditions when compared with different canal-filling materials and entire root canal filled with Biodentin alone [15]. In the current case the weakened tooth structure is reinforced by fiber post and flowable dual cure resin composite was used as adhesive (Figure 3A), which is expected to increase the structural stability of tooth structure. At the same time the limitation of Biodentine is reduced radiopacity compared to other calcium silicate cements because of zirconium oxide as a radiopacifier [16].
Conclusion
A combination of surgical and nonsurgical approach might be appropriate for the management of invasive cervical resorption. A combination of materials can be used to restore ICR defects which have a coronal or radicular extent. Reinforcing the weakened tooth structure with fiber post is expected to increases the longevity of tooth. Finally, future research is needed to device more biocompatible materials with adhesive, reinforcing and esthetic properties for restoring extensive ICR defects.
Acknowledgements
Sincere thanks to department of conservative dentistry and endodontics, Government College of dentistry, Indore, Madhya Pradesh, India
Conflict of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Ethical clearance
Patient consent signed.
References
- Iglesias-Linares A, Hartsfield JK. Cellular and molecular pathways leading to external root resorption. J Dent Res. 2017;96(2):145-52.
- Patel S, Dawood A, Wilson R, et al. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography: An in vivo investigation. Int Endod J. 2009;42(9):831-8.
- Heithersay GS. Management of tooth resorption. Aust Dent J. 2007;105-121.
- Hiremath H, Yakub SS, Metgud S, et al. Invasive cervical resorption: A case report. J Endod. 2007;33(8):999-1003.
- Tronstad L. Root resorption: Etiology, terminology and clinical manifestations. Endod Dent Traumatol. 1988;4(6):241-52.
- Coyle M, Toner M, Barry H. Multiple teeth showing invasive cervical resorption: An entity with little known histologic features. J Oral Pathol Med Off Publ. 2006;35(1):55–7.
- Molven O, Halse A, Fristad I. Long‐term reliability and observer comparisons in the radiographic diagnosis of periapical disease. Int Endod J. 2002;35(2):142-7.
- Cohenca N, Simon JH, Mathur A, et al. Clinical indications for digital imaging in dento‐alveolar trauma. Part 2: Root resorption. Den Traumatol. 2007;23(2):105-13.
- Gulabivala K, Searson LJ. Clinical diagnosis of internal resorption: An exception to the rule. International endodontic journal. 1995;28(5):255-60.
- Odabaş ME, Bani M, Tirali RE. Shear bond strengths of different adhesive systems to biodentine. Sci World J. 2013;2013:626103.
- Laurent P, Camps J, De Méo M, et al. Induction of specific cell responses to a Ca(3)SiO(5)-based posterior restorative material. Dent Mater off Publ Acad Dent Mater. 2008;24(11):148-94.
- Jang E, Lee J, Nam S, et al. Comparison of Microleakage and Compressive Strength of Different Base Materials. J Korean Acad Pediatr. 2021;48(2):168-75.
- Malkondu O, Kazandağ MK, Kazazoğlu E. A review on biodentine, a contemporary dentine replacement and repair material. BioMed Res Int. 2014;2014:160951.
- Singh H, Kaur M, Markan S, et al. Biodentine: A promising dentin substitute. J Interdiscipl Med Dent Sci. 2014;2(140):2.
- Elnaghy A, Elsaka S. Fracture resistance of simulated immature roots using Biodentine and fiber post compared with different canal-filling materials under aging conditions. Clin Oral Investig. 2020;24:1333-8.
- Bosso-Martelo R, Guerreiro-Tanomaru JM, Viapiana R, et al. Physicochemical properties of calcium silicate cements associated with microparticulate and nanoparticulate radiopacifiers. Clin Oral Investig. 2016;20(1):83-90.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref