Research Article - Biomedical Research (2017) Volume 28, Issue 1
Low energy fractures: what is the difference? specific features and clinical outcomes by minimally invasive locking plates
Je-hyun Yoo1, Seok-woo Kim1, Yoon-hae Kwak1, Hong-kyun Kim2, Ji-hyo Hwang2*, Jung-uk Kim2 and Sung-in Hong21Department of Orthopaedic Surgery, Hallym University Sacred Heart Hospital, Hallym University School of Medicine, Anyang, Republic of Korea
2Department of Orthopaedic Surgery, Gangnam Sacred Heart Hospital, Hallym University School of Medicine, Seoul, Republic of Korea
- *Corresponding Author:
- Ji-hyo Hwang
Department of Orthopaedic Surgery
Gangnam Sacred Heart Hospital
Hallym University College of Medicine
Seoul, Republic of Korea
Accepted on June 30, 2016
Abstract
Hypothesis: We hypothesized a locking compression plate was in favor of the treatment of high energy related fracture. Low energy fracture can obtain different outcomes by minimally invasive locked plating. We predict the different clinical features and outcomes compared with previous osteoporosis patients group.
Methods: 34 patients with low-energy distal femoral fractures (mean age 69.6 years) treated with minimally invasive locked plating were enrolled. Fracture pattern at trauma, clinical and radiological evaluations during the follow-up period were analyzed. All patients were followed for a minimum of 12 months postoperatively.
Results: The majority of fractures (76.3%) were extraarticular type and the comminuted fracture configuration was in 19 patients (55.8%), biomechanical fracture pattern was spiral in 10 patients (71.4%) among 14 linear fractures. The mean time to union was 19.1 weeks (range 14-30). Eight patients (23.5%) were shown as delayed union. Four patients (11.7%) developed implant failure. The mean knee range of motion was 116.7 degrees (range 50-140) and the Oxford knee scores averaged 34.4 (range 16-48).
Conclusion: Low energy fracture showed extraarticular communited fracture and noncommunited linear fracture was spiral which looks simple. But the minimally invasive locked plating in these group result in significant delayed union and metal failure. The use of low screw density in the proximal fragment, long plates, a proximal uppermost cortical screw can lower the risk of implant failure in the low energy fractures.
Keywords
Distal femoral fracture, Low-energy trauma, Minimally invasive, Locked plating.
Introduction
Low energy trauma, elderly, osteoporosis is not always closely correlated. Even though young patients, normal bones can be fractured by low energy trauma. We want to focus on only the injury mechanism regardless of age and bone quality. And we analyzed low energy fracture pattern in the distal femur and how much affect the result of minimally invasive locked plating. Distal femoral fractures constitute only 4%-7% of all femur fractures, these fractures are caused by low energy in elderly and high-energy trauma in young adults, but the incidence of low energy fracture has increased due to an increase in the elderly population [1-3]. Low energy fractures can be challenging to treat due to weakened bone strength and low healing potential. Therefore, these fractures must be accurately reduced and fixed with enough stability to obtain favorable outcomes through the maintenance of appropriate alignment and early rehabilitation [2-5]. An angularly stable locking compression plate (LCP) and minimally invasive plate osteosynthesis (MIPO) technique is an integral tool that leads to improved biomechanical performance and has resulted in favorable outcomes especially in the treatment of unstable or communited fractures [5-10]. However, distal femoral fractures caused by indirect low-energy trauma are different from those results from direct high-energy trauma, and deserve more attention than they have been given in the literature. Therefore, this study assessed the patterns of low-energy distal femoral fractures and delineated outcomes and problems associated with minimally invasive locked plating as a form of treatment.
Materials and Methods
There is general consensus that low-energy trauma can be defined as a fall from a standing height or low height of less than 1 m [11]. We gathered our cases between March 2009 and March 2013. A total of 34 patients who underwent minimally invasive locked plating were followed up at least one year. The age, gender, injury mechanism, comorbidity, Bone Mineral Density (BMD), fracture classification and configuration were recorded. About the fracture classification, we used the Arbeitsgemeinschaft für Osteosynthesefragen and Orthopaedic Trauma Association (AO/OTA) classification.
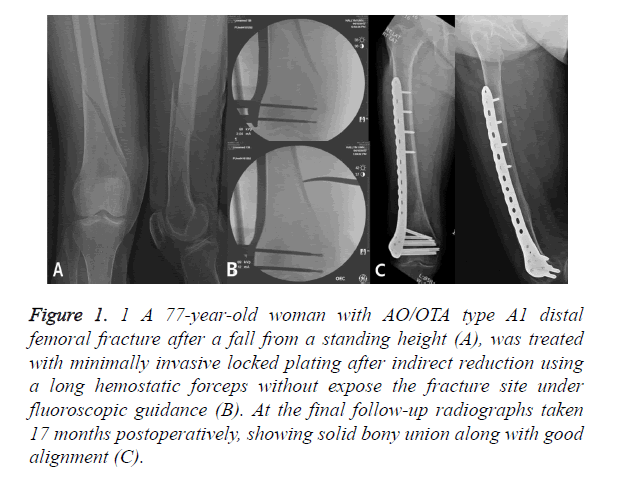
A 4-5 cm skin incision was made on the lateral side of the thigh. A anatomical stainless steel locking plate (Zimmer Periarticular Plate, Warsaw, Indiana) assembled with the Less Invasive Stabilization System (LISS) was introduced submuscularly. The plate was temporarily held with K-wires or drill bits and confirmed coronal and sagittal alignment under fluoroscope. Distal fixation was performed with the LISS, and reduction of the proximal fragment was done, as accurately as possible, with manual traction and percutaneous reduction techniques using long Kelly forceps (Figure 1) or a collinear reduction clamp. After satisfactory length and rotation were achieved, the plate was secured to the bone with a locking or cortical screw. Conventional cortical screws were used when necessary to reduce the gap between the plate and bone and locking screws were mainly used. A cortical or locking screw was randomly used as the proximal uppermost screw in all cases except two, in which cerclage wirings were needed due to the overlap of the proximal plate and the preexisting hip nail or stem. The operation time, plate length, plate-screw density, and type of the proximal uppermost screw were recorded.
Figure 1. 1 A 77-year-old woman with AO/OTA type A1 distal femoral fracture after a fall from a standing height (A), was treated with minimally invasive locked plating after indirect reduction using a long hemostatic forceps without expose the fracture site under fluoroscopic guidance (B). At the final follow-up radiographs taken 17 months postoperatively, showing solid bony union along with good alignment (C).
The mean duration of hospital stay was 15 days (range 7-35). After discharge, protected weight-bearing with the use of a walker or crutches was recommended until the fracture was clinically and radiographically judged to be united. Follow-up evaluations were performed at 6 weeks; 3, 6, and 9 months; and then annually. The range of motion of knee joint, the Oxford knee score (excellent ≥ 40, good ≥ 30, moderate ≥ 20, poor <20), radiological evidence of union, and any complications were checked. Delayed union was considered to be present if bony union of the fracture had not taken place within 24 weeks after index surgery. The mean follow-up period was 23 months (range 12-34). We used Wilcoxon rank-sum test and Fisher’s exact test for the statistical analysis. We got the approval of IRB in our hospital. No external funding was received for our study.
Results
The mean age was 69.6 years (range 50-87) and twenty seven patients (79.4%) were ≥ 60 years. 30 patients (88.2%) were female. The mechanism of injury was fall from a standing height in 19 patients (55.8%) and from a low height of less than 1 m in 11. Four patients with post-poliomyelitis related fractures without significant trauma (rotating in bed, moving from a wheelchair to a bed, and lifting one leg over the other). The average BMD (T-score) is -2.2 (ranged -4.6~ -0.8). The patients’ demographic characteristics are presented (Table 1). 32 patients (94.12%) showed weakened bone or osteoporosis which is predisposed to a low-energy distal femoral fracture. Four patients with post-poliomyelitis had subsequent osteopenia in the ipsilateral lower limb, and three patients had hemiparesis on the ipsilateral side due to previous cerebrovascular accidents. One patient had stiffness and disuse osteopenia in the ipsilateral knee joint after prior arthroscopic knee surgery.
| Age (years) | 69.6 (50 ~ 87) |
| Gender (male : female) | 4:30 |
| Involved side (number) | |
| Right : Left | 17:17 |
| Injury Mode (number) | |
| Fall from a standing height | 19 |
| Fall from a low height | 11 |
| No significant trauma | 4 |
| Bone mineral density (T-score) | -2.2 (-4.6 ~ -0.8) |
| AO fracture types (number) | |
| A1:A2:C1 | 15:11:8 |
| Fracture configuration (number) | |
| Communited | 19 |
| Spiral | 10 |
| Obilque | 5 |
| Duration of follow-up (months) | 23 (12 ~ 35) |
| Values are presented as mean (range). | |
Table 1. Demographic data of a total of 34 patients.
All fractures were closed, and none of the patients had significant concurrent injuries. Using the AO/OTA classification, 76.3% of the patients had extraarticular fractures. Type (A1) in 15 (44.1%) was the most common subtype. The most common biomechanical fracture pattern was a spiral pattern in 10 cases (71.4%) among the 14 simple linear fractures (Figure 1).
The mean operation time was 85 minutes (range 60-110). Locking plates’ average length was 12 holes (range 8-18 holes), and the total plate-screw density averaged 0.60 (range 0.50-1.00), and densities for the proximal fragment, fracture site, and distal fragment averaged 0.50, 0.11, and 0.95, respectively (Table 2). A conventional cortical screw was used as the proximal uppermost screw in 17 cases, and a locking screw was used in 17 cases, randomly.
| Length of plate | 12 (8 ~ 18) |
| Plate-screw density | |
| Total | 0.60 (0.50 ~ 1.00) |
| Proximal | 0.50 (0.30 ~ 1.00) |
| Fracture site | 0.11 (0 ~ 1.00) |
| Distal | 0.95 (0.71 ~ 1.00) |
| Type of screw inserted at the proximal uppermost hole | |
| Cortical : Locking (number) | 17:17 |
| Radiographic evaluation | |
| Varus(-) / Valgus(+) | -0.35 (-5 ~ +4) |
| Anterior(+)/Posterior(-) angulation | 0.35 (-5 ~ 7) |
| Leg-length discrepancy (mm) | 3.5 (0 ~ 8.3) |
| Union period (weeks) | 19.1 (14 ~ 30) |
| Values are presented as mean (range). | |
Table 2. Surgical and radiographic outcomes of 34 patients.
Osseous union was achieved in all cases, including three patients who underwent reoperation due to implant failure, with an average union time of 19.1 weeks (range 14-30). Although union was delayed in 8 cases (23.5%), these fractures finally united without need for subsequent reoperation. There were no other complications such as nonunion, malunion, infection, deep vein thrombosis, or pulmonary embolism during follow-up after surgery. Four patients, however, experienced implant failure within the zone of the proximal fragment before union. In all these patients, the locking screw was used as the proximal uppermost screw and plate-screw density in the proximal fragment was over 0.6. Also, locking plate used in these patients was relatively short with averaged 10 holes. At the final follow-up, the mean range of knee motion was 116.7 degrees (range 50-140). The Oxford knee score ranged between 16 and 48 with an average of 34.4. Twenty-nine patients (86.9%) rated their function as good or excellent. Four patients had medial knee pain caused by soft tissue irritation due to the protrusion of distal metaphyseal screws.
We compared the non-failure and failure groups. No significant differences were found in preoperative demographic and radiographic data, except for surgical data. Only total and proximal plate-screw densities were significantly higher in the failure group, with p-values of 0.013 and 0.011, respectively (Table 3). Shorter plates and locking screws as the proximal uppermost screw tended to be used in the failure group, although there was no statistical significance (p=0.075 and 0.063, respectively).
| Non-failure group (n=30) |
Failure group (n=4) |
p-value | |
|---|---|---|---|
| Age (years) | 71 (63 ~ 77) | 70 (64 ~ 80) | 0.964 |
| Gender (male : female) | 3:27 | 1:03 | 0.409 |
| Bone mineral density (T-score) | -1.6 (-2.7 ~ -1.5) | -2.4 (-2.9 ~ -0.8) | 1 |
| Involved side (right : left) | 14:16 | 3:01 | 0.601 |
| Length of plate | 14 (12 ~ 16) | 10 (8 ~ 14) | 0.075 |
| No. of screws used | 11 (10 ~ 11) | 13 (10 ~ 14) | 0.214 |
| Plate-screw density | |||
| Total | 0.55 (0.54 ~ 0.61) | 0.71 (0.65 ~ 1.00) |
0.013 |
| Proximal | 0.44 (0.39 ~ 0.50) | 0.67 (0.63 ~ 1.00) |
0.011 |
| Fracture site | 0 (0 ~ 0.14) | 0.20 (0 ~ 1.00) |
0.119 |
| Distal | 1.00 (0.86 ~ 1.00) | 1.00 (0.86 ~ 1.00) |
1 |
| Type of screw inserted at the proximal uppermost hole | |||
| Cortical : Locking (number) | 17:13 | 0:04 | 0.063 |
| Radiographic evaluation | |||
| Varus(-) / Valgus(+) | 0 (0 ~ 0) | 0 (-3 ~ 0) | 0.554 |
| Anterior(+)/Posterior(-) angulation | 0 (0 ~ 0) | 0 (-3 ~ 7) | 0.876 |
| Values are presented as median (interquartile range). | |||
Table 3. Comparison data between non-failure and failure groups.
Discussion
Distal femoral fracture in older adults is an injury associated with low-energy trauma due to a preexisting condition that can weaken bone strength [1-3]. Due to flimsy bone and soft tissue, and low healing potential, this type of fracture may present many clinical challenges. A locking plate and the MIPO technique have helped to address these challenges and have widely been used as integral tools for achieving firm fixation in older adults [5-10]. However, complications such as implant failure, nonunion, and malunion have occurred owing to controversy over the efficacy of locked plating and the optimal mechanical environment [12-16]. No previous study has focused on the specific features of distal femoral fractures caused by low-energy trauma. Therefore, this study was conducted to identify the patterns of distal femoral fractures caused by low-energy trauma and to delineate outcomes and problems associated with minimally invasive locked plating in these types of fractures.
In our series, all fractures had a relatively simple configuration, with minimal comminution and soft tissue injury secondary to low-energy trauma. The most common simple linear fracture pattern was a spiral type. This fracture pattern results from indirect, torsional, low-energy injury [17]. All fractures occurred in patients with preexisting conditions that were likely to weakened the bone except for two patients who did not have a predisposing condition except old age greater than 60 years. A previous study of cadaver femora and tibia showed a consistent decrease with age of all mechanical properties except plastic modulus in femoral but not tibial specimens [18]. Accordingly, weakening of the mechanical strength of the femora might have occurred in these two patients.
A simple fracture pattern with less comminution and a broad contact area at the fracture site may induce indirect reduction more easily and accurately, and subsequently lower the risk of malunion and nonunion. However, a broad fracture area and general or local conditions that weaken the mechanical strength of the femur are likely to make internal fixation technically demanding, and bony union may take longer than expected. Therefore, thorough preoperative analysis of these main points should be conducted [11,16]. In our series, there was no nonunion, malunion, or infection. These results might have been caused by more accurate reduction using percutaneous reduction techniques, careful tissue handling, and stable biologic fixation using the MIPO technique [14,19]. Despite these findings, the rate of delayed union (23.5%) was relatively high compared with previously reported rates [20-22]. In patients with delayed healing, it is known that implants are subject to prolonged load cycling, thereby increasing the chance of implant failure through plate breakage or loosening [23]. However, all fractures with delayed union in our study finally united without the need for an additional operation. We attributed this to a relatively accurate reduction and the use of a long spanning plate in a locking mode without lag screws, which allowed proper tension at the fracture gap to promote callus formation. The use of long plates theoretically increases the plate’s working length and hence increased the number of cycles it can withstand load until failure [15]. These fixation principles, which were used in 8 patients with delayed union, allowed full weight-bearing as tolerated, even in the presence of delayed union without implant failure or screw loosening.
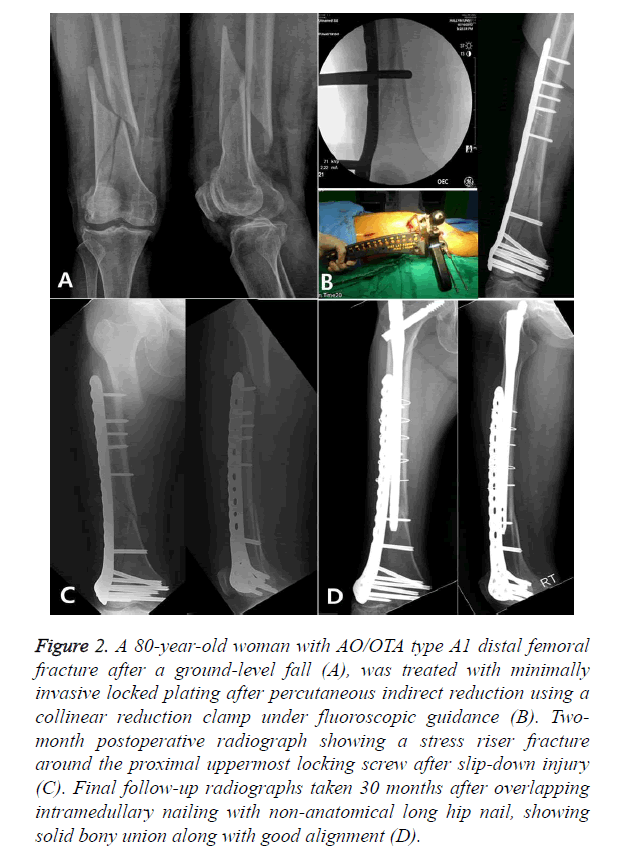
In our study, 4 implant failures occurred within 3 months after surgery, probably owing to improper implant selection and inattention to the principles of LCP [14,23]. In simple fractures, omission of 1 or 2 screw holes on each side of the fracture is recommended [24]. Moreover, the plates should have a higher plate-span ratio and lower plate-screw density than those in comminuted, high-energy fractures [14]. Of the 4 implant failures, three might have been caused by high plate-screw density and insufficient fixation of the proximal fragment owing to the use of short plates, and insufficient fixation might have been aggravated by the use of a unicortical locking screw as the proximal end screw in two of these cases. The other one failure might have been caused by stress-concentration at the junction of the plate and bone due to high plate-screw density and a bicortical locking screw used as a proximal end screw, which acted as a stress-riser (Figure 2) [13].
Figure 2. A 80-year-old woman with AO/OTA type A1 distal femoral fracture after a ground-level fall (A), was treated with minimally invasive locked plating after percutaneous indirect reduction using a collinear reduction clamp under fluoroscopic guidance (B). Two-month postoperative radiograph showing a stress riser fracture around the proximal uppermost locking screw after slip-down injury (C). Final follow-up radiographs taken 30 months after overlapping intramedullary nailing with non-anatomical long hip nail, showing solid bony union along with good alignment (D).
Total and proximal plate-screw densities were significantly higher in the failure group than in the non-failure group, and shorter plates and proximal end locking screws tended to be used in the failure group. Therefore, longer plates and fewer proximal screws should be used as much as possible to gain a high plate-span ratio and a low plate-screw density, and to lower the risk of implant failure. A longer plate than expected is demanded because distal femoral fractures caused by low-energy trauma generally have simple fracture pattern, but a long and broad fracture area [14]. Therefore, implant failures could be preventable through the thorough and careful preoperative planning by the operator. The current study has several limitations, of which small sample size is one. Another limitation is the lack of a control group with the retrospective nature. However, our study is strengthened by the first clinical study focused on low-energy distal femoral fractures treated with only one kind of locking plate at a single center and comparative analysis on implant failure.
Conclusion
Distal femoral fractures caused by low-energy trauma had a relatively simple configuration and less comminution, and occurred mostly in older women. The use of minimally invasive locked plating for this type of fracture resulted in higher delayed union and metal failure than expected. Considering a relatively long and broad fracture area, simple fracture pattern, and weakened bone strength in low-energy distal femoral fractures, the use of long plates and only a few proximal screws, as well as a proximal uppermost cortical screw, is expected to lower the risk of implant failure and lead to better outcomes.
References
- Martinet O, Cordey J, Harder Y. The epidemiology of fractures of the distal femur. Injury 2000; 31: C62-63.
- Doshi HK, Wenxian P, Burgula MV, Murphy DP. Clinical outcomes of distal femoral fractures in the geriatric population using locking plates with a minimally invasive approach. Geriatr Orthop Surg Rehabil 2013; 4: 16-20.
- Schandelmaier P, Gossling T, Partenheimer A, Krettek C. Distal fractures of the femur. Chirurg 2002; 73: 1221-1233.
- Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL. Locking plates for distal femoral fracutres: Is there a problem with fracture healing? J Orthop Trauma 2011; 25: S8-14.
- Wong MK, Leung F, Chow SP. Treatment of distal femoral fractures in the elderly using a less-invasive plating technique. Int Orthop 2005; 29: 117-120.
- Kubiak EN, Fulkerson E, Strauss E, Egol KA. The evolution of locked plates. J Bone Joint Surg Am 2006; 88: 189-200.
- Markmiller M, Konrad G, Sudkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res 2004; 426: 252-257.
- Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br 2002; 84: 1093-1110.
- Wӓhnert D, Hoffmeier K, Fröber R, Hofmann GO, Mückley T. Distal femoralfracturesof the elderly-different treatment options in a biomechanical comparison. Injury 2011; 42: 655-659.
- Zlowodzki M, Williamson S, Cole PA, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femoral fracutres. J Orthop Trauma 2004; 18: 494-502.
- Sari S, Harri P, Veikko A, Antti K, Ole B. Specific features associated with femoral shaft fractures caused by low-energy trauma. J Trauma 1997; 43: 117-122.
- Bostman O, Varjonen L, Vainionpaa S, Majola A, Rokkanen P. Incidence of local complications after intramedullary nailing and after plate fixation of femoral shaft fractures. J Trauma 1989; 29: 639-645.
- Bottlang M, Doornink J, Byrd GD, Fitzpatrick DC, Madey SM. A nonlocking end screw can decrease fracture risk caused by locked plating in the osteoporotic diaphysis. J Bone Joint Surg Am 2009; 91: 620-627.
- Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury 2003; 34: 63-76.
- Hoffmeier KL, Hofmann GO, Mückley T. Choosing a proper working length can improve the lifespan of locked plates. A biomechanical study. Clin Biomech 2011; 26: 405-409.
- Ricci WM, Streubel PN, Morshed S. Risk factors for failure of locked plate fixation of distal femoral fracutres: an analysis of 335 cases. J Orthop Trauma 2014; 28: 83-89.
- Alms M. Fracture mechanics. J Bone Joint Surg Br 1961; 43: 162-166.
- Burstein AH, Reilly DT, Martens M. Aging of bone tissue: mechanical properties. J Bone Joint Surg Am 1976; 58: 82-86.
- Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma 1999; 13: 401-406.
- Henderson CE, Bottland M, Lujan T. Stabilization of distal femoral fractures with intramedullary nails and locking plates: differences in callus formation. Iowa Orthop J 2010; 30: 61-68.
- Schandelmaier P, Partenheimer A, Koenemann B. Distal femoral fractures and LISS stabilization. Injury 2001; 32: 55-63.
- Schutz M, Muller M, Krettek C. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury 2001; 32: SC48-54.
- Huang HT, Huang PJ, Su JY. Indirect reduction and bridge plating of supracondylar fractures of the femur. Injury 2003; 34: 135-140.
- Stoffel K, Dieter U, Stachowiak G, Gachter A, Kuster MS. Biomechanical testing of the LCP-how can stability in locked internal fixators be controlled? Injury 2003; 34: B11-19.