- Biomedical Research (2012) Volume 23, Issue 3
Long-term therapeutic efficacy of daytime ambulatory peritoneal dialysis and continuous ambulatory peritoneal dialysis
Zhi-yong Zhang*, Ming-xu Li, Yong-wu Yu and Chun-hua ZhouDepartment of Nephrology, Naval General Hospital of PLA, Beijing 100048, China
- *Corresponding Author:
- Zhi-yong Zhang
Department of Nephrology
Naval General Hospital of PLA
Beijing 100048, China
Accepted date: May 07 2012
Abstract
The objective of the present study is to compare the long-term therapeutic efficacy of daytime ambulatory peritoneal dialysis (DAPD) and traditional continuous ambulatory peritoneal dialysis (CAPD) and to find an optimal method for Chinese requiring long-term peritoneal dialysis (PD). A total of 32 inpatients and outpatients receiving PD were randomized into group A (n=16) and group B (n=16). Patients in group A were treated with traditional CAPD, four 8- L exchanges were carried out, and dwelling was performed overnight. Patients in group B were treated with DAPD, 8-L exchange was performed with dwell time of 3~4 h and a dry abdomen at night. Barthel index (BI) and Hamilton Depression Rating Scale (HAMD) were employed. The urine volume and ultrafiltration volume were measured. Comparisons of means were performed with analysis of variance among groups and t test or chi square test was employed for comparisons between two groups. There were no marked differences in the residue urine volume, ultrafiltration volume, dialysis adequacy (Kt/V per week; Ccr), CO2CP, K+ and Ga2+ between two groups (P>0.05). However, in the group B, the nutrition status, Hb, P-, iPTH, mean arterial pressure, abdominal infection, number of patients continuously receiving PD, duration of PD, employment rate, BI score and HAMD score were significantly superior to those in the group A (P<0.05) (Table 2, 3). Conclusion: In the presence of same dialysis dosage, long-term DAPD is superior to CAPD in the duration of PD, dialysis adequacy, nutrition status, complication control, blood pressure, abdominal infection control, activity of daily living and depression prevention.
Keywords
Chinese; peritoneal dialysis; dialysis adequacy; quality of life
Introduction
Peritoneal dialysis (PD) has been a treatment of choice for patients with end stage renal disease (ESRD) because it is beneficial for the protection of residual kidney function and maintenance of stable hemodynamics and simple to perform. However, the regimens for PD vary among different countries and regions. In the majority of western countries and China, four 2-L exchanges are frequently carried out in continuous ambulatory peritoneal dialysis (CAPD) [1]. To explore the long-term survival rate, improve the quality of life (QOL) and attenuate the influence of PD on activity of daily living (ADL) of patients receiving PD, the traditional CAPD was modified in our department as daytime ambulatory peritoneal dialysis (DAPD) for maintenance of PD. In the present study, the clinical information and laboratory findings of patients receiving PD were collected within 5 years aiming to compare the clinical efficacy of long term DAPD and CAPD.
Patients and Methods
Patient characteristics
A total of 32 patients with renal dysfunction were recruited from our department from January 2001 to June 2006. These patients had no history of mental disorder and physical disabilities and received PD for a long time. There were 14 males and 18 females with the age range of 27~79 years. The primary disease was glomerulonephritis 9 patients, diabetic nephropathy in 14, lupus nephritis in 1, chronic pyelonephritis in 1, renal arteriosclerosis in 6 and interstitial nephritis in 1. The study has been approved by the Ethical Committee of Naval General Hospital of PLA.
Methods for dialysis
These patients were randomly divided into two groups (n=16 per group). In Group A, standard CAPD was performed and four 8-L exchanges were used at daytime followed by a dry abdomen at night. In Group B, four 8-L exchanges were also performed and each exchange was done within 3~4 h. After 4 exchanges, a dry abdomen was allowed overnight. The dialysate was purchased from Baxter, USA and glucose was used as an osmotic agent. The concentration of dialysate was 1.5%, 2.5% or 4.25%. The complications of end stage renal failure were correspondingly treated such as pressure lowing, regulation of acid-base balance and maintenance of electrolyte stability.
Observations
For patients receiving PD, routine blood test and detection of biochemical variables and dialysate were performed monthly. The body weight was measured daily. The ultrafiltration volume, urine volume and blood pressure were determined daily. The adequacy of dialysis (Kt/V per week; Ccr), nutrition state (SGA, sALB), complications (Hb, CO2CP, K+, Ga2+, P-, iPTH), blood pressure control (mean arterial pressure), abdominal infection, activity of daily living (ADL) and depression were regularly evaluated. The social activity, employment and duration of dialysis (month) were also recorded. Before study, medical information was defined as baseline level. At 5 years after PD, the study was terminated and medical information was defined as endpoint. Patients who received renal transplantation, died or were unable to receive original PD were excluded from this study and did not receive further evaluation.
Assessment of ADL
The Barthel index (BI) scale, a widely used scale internationally, was employed for the evaluation of ADL [2]. The total score was 100. The higher the score, the stronger the self-care ability.
Assessment of depression
Hamilton Depression Rating Scale (HAMD), a commonlu used scale in clinical practice, was employed to evaluate the depression of these patients. This scale is designed to observe symptoms and findings are objective and can reflect the changes in symptoms of depression. The total score presents the severity of depression. The lower the score indicates the milder the depression. Generally, score of >24 was defined as severe depression, score of 17 as moderate depression and score of <7 as absence of depression [3].
Statistical analysis
Statistical analysis was performed with SPSS version 15.0 statistics package. Quantitative data were expressed as mean ± standard deviation. Comparisons of quantitative data were done with t test and those of rate with Fisher’s exact test between two groups. A value of P<0.05 was considered statistically significant.
Results
General information
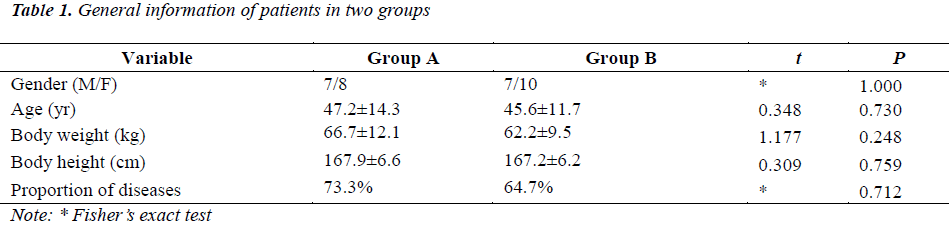
There were no marked differences in the age, gender, body weight, body height and type of diseases (proportion of diseases except for diabetes) between two groups (P>0.05) (Table 1).
Medical variables at baseline
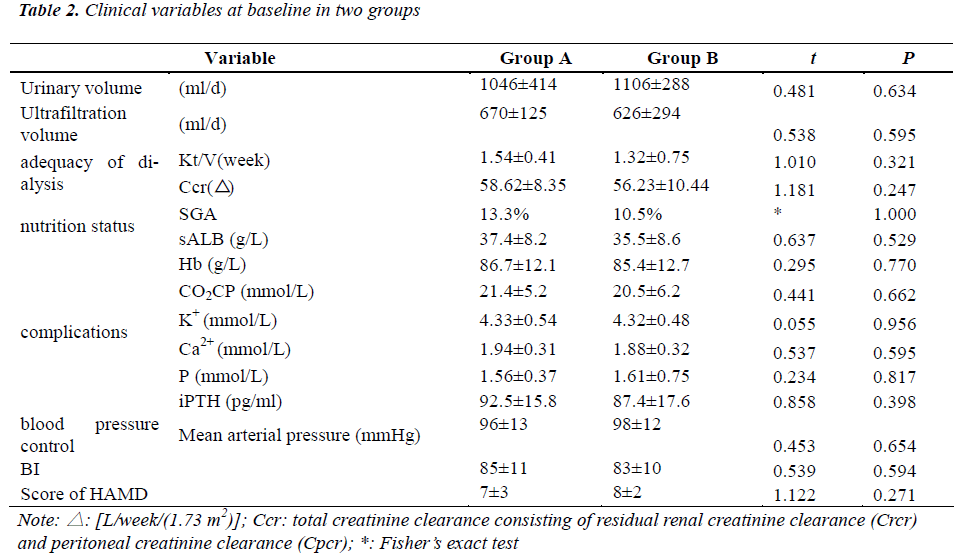
Before study, the related medical variables were measured. The Kt/V per week and Ccr were employed to evaluate the adequacy of dialysis; subjective global assessment (SGA) and serum albumin (sALB) were used to assess the nutritional status; hemoglobin (Hb), Serum carbon dioxide combining power (CO2CP), serum levels of potassium (K+), calcium (Ca2+), phosphorus (P) and free parathyroid hormone (iPTH) were applied to evaluate the control of complications of chronic renal failure; mean arterial pressure was used to assess the control of blood pressure; BI was used to evaluate the ADL, score of HAMD was applied to assess the severity of depression aiming to detect the ability of self-care and the influence of PD on mental status.
Our results showed there were no significant differences in the residual urinary volume, ultrafiltration volume, adequacy of dialysis, nutrition status, complications, blood pressure control, BI of ADL and severity of depression between two group (P>0.05) (Table 2).
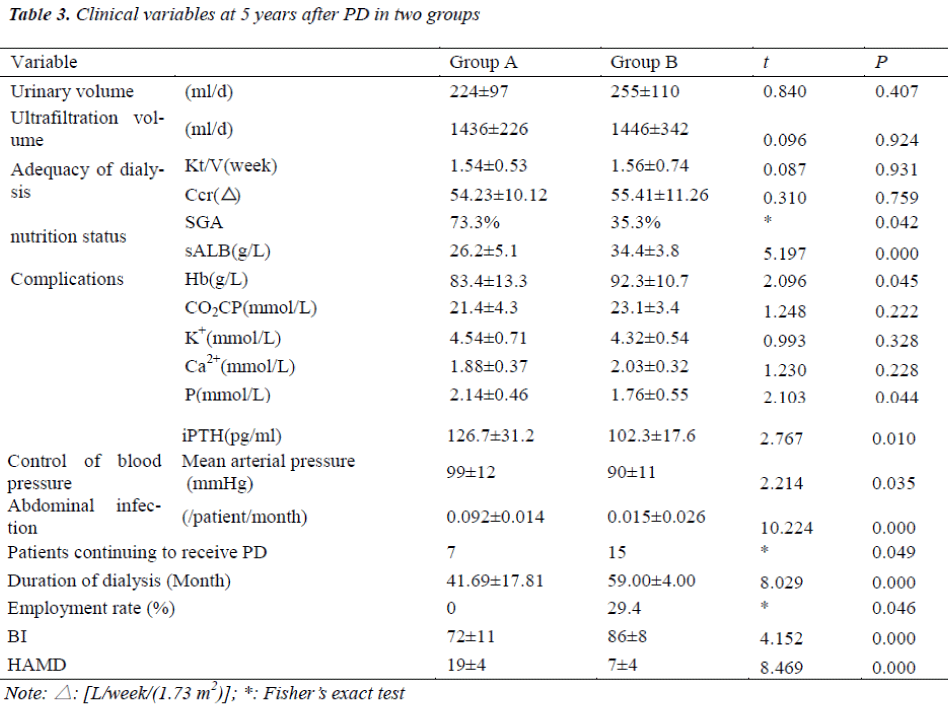
Clinical variables at 5 years after PD
Five years after PD, clinical variables were measured again. Results showed some patients in Group A could not continuously receive CAPD but underwent DAPD and these patients were excluded from this study. However, the duration of CAPD was also recorded for analysis. In the Group B, the majority of patients continuously undergo DAPD. There were no marked differences in the residual urinary volume, daily ultrafiltration volume, adequacy of dialysis (Kt/V per week and Ccr), and serum levels of CO2CP, K+ and Ca2+ between two groups.
In the Group B, the nutrition status, the serum levels of Hb, P- and iPTH, mean arterial pressure, abdominal infection, number of patients continuing to receive PD, duration of PD, employment rate, BI, score of HAMD were markedly superior to those in the Group A (P<0.05) (Table 3).
Discussion
The commonly used methods for PD include CAPD and IPD. Classic IPD is the initial way for PD and mainly applied in acute renal failure patients who are unable to receive hemodialysis (HD). Generally, in IPD, 25-L of dialysate was used within 24 h and exchange was performed with 2 L of dialysate once every 2 h (perfusion for 10 min, dwelling for 90 min and draining for 20 min). Exchange in short time may maximize the ultrafiltration. However, long-term dialysis with this method can not assure the sufficient clearance of solutes. Thus, generally, IPD is applied in patients temporarily (acute renal failure, waiting for training of CAPD, fluid leakage, postoperation, requirement of massive dehydration due to body fluid overload. In addition, IPD may also be used in old patients who have no vascular access or those receiving CAPD in whom the HD is unstable and self-management is difficult to perform. In the CAPD, dialysate is perfused into the abdominal cavity and allow to be dwelled in the abdominal cavity until nest dialysis is required. Generally, exchange is done forth daily and according to disease condition. Under this condition, dialysate may be present in the abdominal cavity all the day. The adequacy of dialysis in CAPD is superior to that in IPD and thus CAPD has been the most widely used method for PD [4-6].
In China mainland, the patients receiving PD account for about 10% of patients receiving dialysis [7]. The causes of inability to widely and long-lastingly apply PD include inferiority in the clearance of water and small molecular substances to HD, high prevalence of abdominal distension, loss of appetite and malnutrition following PD, risk for abdominal infection and presence of peritoneal ultrafiltration failure within 2~3 years.
With the prolongation of PD, peritoneal angiogenesis and fibrosis are present, the functions of aquaporins and tight junction protein are lost and peritoneal mast cells aggregate, all of which may cause damage to peritoneum leading to changes in structure and transfer ability of peritoperitoneum. These may finally result in peritoneal ultrafiltration failure and subsequent PD failure [8]. The causes of PD related peritoneal fibrosis and subsequent dialysis failure are numerous and mainly include recurrent peritonitis, influence of dialysate on peritoneum and cytokines.
Generally, the adequacy of PD include: (1) the dialysis dose is sufficient or the effectiveness of dialysis is satisfactory; (2) the mortality do not increase at a specific dialysis dose, but reduction of this dialysis dose may significantly increases mortality; (3) Following dialysis, patients feel well and have favorable appetite, gain of body weight and physical recovery, the chronic complications are reduced or absent, and uremia related toxins are completely cleared [9]. However, a lot of clinical studies have demonstrated that the adequacy of dialysis can not be evaluated with urea and/or creatinine clearance alone [10]. The water balance and maintenance of homeostasis may be more important than those above. Thus, sufficient PD refers to dialysis at a specific dose can achieve long term survival and maintain favorable quality of life.
Traditional HD and PD emphasize the clearance of small molecules but ignore the importance of volume management. In addition, to enhance the clearance of small molecules does not reduce the high mortality [11]. Moreover, the volume load and hypertension, left ventricular hypertrophy and inflammation are closely related to malnutrition and have become important predictors of death in patients receiving PD [12,13]. These demonstrate the importance of volume management and blood pressure control.
To assure the good effectiveness of dialysis, prevent peritoneal fibrosis, delay peritoneal ultrafiltration failure and prolong the life-span of PD technique have been clinical challenges. To solve these problems, we abandoned traditional CAPD and modified classic IPD. In the present study, DAPD was employed for the maintenance of PD. In this method, 4 exchanges were carried out and each exchange was done for 3~4 h. Following 4 exchanges, the abdomen was allowed to be dry. This method abandoned the indwelling of dialysate for 24 h in CAPD and a dry abdomen was allowed for a relatively long time which maintains the normal physiology. Under this condition, it has enough time to recover the peritoneal mesothelial cells and the functions of intraperitoneal organs, especially the gastrointestinal tract. The motility, absorption and digestion of gastrointestinal tract are not affected in the “dry abdomen” state, the nutrition status is improved, the sleep is not influenced, activity of daily living is maintained and the risk for operation related abdominal infection is also reduced. The long-term observation demonstrated that this method could effectively prevent and delay peritoneal fibrosis and peritoneal ultrafiltration failure, preserve the long-term effectiveness of clinical dialysis, increase the quality of life and prolong the duration of PD.
In the present study, all patients receiving DAPD smoothly underwent PD and the duration of PD was far longer than generally 2~3 years. In addition, at the same dialysis dose, dialysis with this method presented advantages in the adequacy of dialysis, improvements of nutrition status, anemia, acid-base balance, electrolyte metabolism and hyperparathyroidism, control of blood pressure and abdominal infection and improvement of activity of daily living, depression and social activities.
The DAPD has less influence on gastrointestinal function. Thus, the appetite, absorption, limitation in activity of daily living, nutrition status and quality of life are improved [14]. Malnutrition is frequently found in patients receiving PD and can be used to predict the incidence of complications and mortality of these patients [15-18]. To improve the nutrition status is critical for the improvement and control of some complications [19].
In addition, we also found that, when compared with standard CAPD in which a large amount of dialysate is dwelled in the abdominal cavity all the day, modified DAPD allows a dry abdomen overnight, which significantly improves the quality of sleep, alleviates the fluid retention, maintains the stable cardiovascular function and is beneficial for the control of blood pressure and recovery and maintenance of activity of daily living. Thus, patients are susceptible to accept this method for PD, which improve the compliance to treatment and alleviate the influence of end stage renal disease on mental health in these patients.
In addition, numerous studies have found that anxiety and depression are the common concomitant diseases in patients with uremia [20-23]. Both PD and HD may cause limitation on the normal activity in these patients. However, the activity is closely related to the self-reported quality of life, mood and social function [24]. When compared with traditional CAPD, the DAPD used in the present study allows a dry abdomen overnight, which also improves the daily activity and alleviate the burden on time, energy, and economy due to PD. Of course, this also improves the depression and subsequently the quality of life and prolongs the duration of PD. Since the application of this method, the majority of patients received DAPD for more than 5 years and satisfactory clinical effectiveness has been achieved.
Taken together, based on the long-term observation on clinical effectiveness of DAPD, our findings demonstrate the dry abdomen state in DAPD is helpful to recover peritoneal mesothelial cells, delay peritoneal ultrafiltration failure, improve the functions of intraperitoneal organs, alleviate fluid retention, stabilizes the cardiovascular system, improve the nutrition status and resistance in these patients, preserve the favorable daily activity, alleviate the depression, improve the quality of life and relieve the economic burden achieving favorable clinical effectiveness.
References
- Burkart JM: The ADEMEX study and PD adequacy. Blood Purif 2003;21 (1): 37-41
- Pu CQ. Cerebrovascular disease. Beijing: People's Mil- itary Medical Press. pp520-538, 1999.
- Cai ZJ. Basic and clinical research on depression. Bei- jing: Science Press 1997; 86-109
- Coles GA. Clinical research in peritoneal dialy- sis .Contrib Nephrol 2001; 131: 125-131
- Gokal R. Peritoneal dialysis in the 21 st century: an analysis of current p roblems and future developments. J Am Soc Nephrol 2002; 13 (Supp l1): 104-116
- Grzegorzewska AE. What is new in peritoneal dialysis in the years 2003-2004. Rocz Akad Med Bialymst 2004; 49: 170-173
- Wang T, Ye RG. Peritoneal dialysis should be a treat- ment of choice for patients with end stage renal failure in China. Chin J Integ Trad West Nephrol 2002; 3: 1
- Gao D, Liu ZS, Zhao ZZ. Detection of Basic fibroblast growth factor in the peritoneum of patients with ul- trafiltration failure following peritoneal dialysis. J Zhenzhou Univ (Med Sci) 2010; 45 (6): 917-920
- Dong J. The investigation of adequacy variables and their ideal values for peritoneal dialysis. Chin J Blood Purif 2010; 9 (10): 526-528
- Gong DH, Ji DX. New understandings on urea kinetic model and adequacy of dialysis in hemodialysis. Chin J Nephrol Dial Transplant 2001; 10 (3): 278
- Paniagua R, Amato D, Vonesh E, Correa-Rotter R, Ramos A, Moran J, Mujais S; Mexican Nephrology Collaborative Study Group. Effects of increased perito- neal clearances on mortality rates in peritoneal dialysis: ADEMEX, a prospective,randomized,controlled trial. J Am Soc Nephrol 2002; 13: 1307-1320
- Brunkhorst R.Hypervolemia, arterial hypertension and cardiovascular disease: A largely neglected problem in peritoneal dialysis. Clin Nephrol 2008; 69: 233-238
- Stegmayr BG.Ultrafiltration and dry weight-what are the cardiovascular effects? Artif Organs 2003; 27: 227-229
- Gui ZH, Wang HL, Zhang JY. Malnutrition inflamma- tion score can evaluate malnutrition-inflammation sta- tus in Chinese peritoneal dialysis patients. Chin J Blood Purific 2010; 9 (10): 529-533
- Dombros NV. Pathogenesis and management of malnu- trition in chronic peritoneal dialysis patients. Nephrol Dial Transplant 2001; 16(Supp l6): 111-113
- CANADA - USA (CANUSA) Peritoneal Dialysis Study Group. Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. J Am Soc Nephrol 1996; 7 (2): 198-207
- Guo DH, Liu WH, Zhang DL. Analysis of causes and predictors of death in patients receiving sustained he- modialysis and peritoneal dialysis. Chin Gen Pract 2007; 10 (9): 704.
- Liu S, Zhang DL, Liu J. Relationship between Micro- inflammatory State, Dialysis Adequacy and Nutritional Status in Diabetic Nephropathy Patients Undergoing Peritineal Dialysis. Chin Gen Pract 2008; 11 (8): 1475
- Zhu N, Yuan WJ, Liu J. Correlation of high mobility group box protein 1 with microinflammatory state and nutritional status in continuous ambulatory peritoneal dialysis patients. Chin J Nephrol 2010; 26 (10): 801-802
- Lye WC, Chan PS, Leong SO, van der Straaten JC. Psychosocial and psychiatric morbidity in patients on CAPD. Adv Perit Dial 1997; 13: 134-136.
- Juergensen PH, Zemchenkov A, Watnick S, Finkelstein S, Wuerth D, Finkelstein FO. Comparison of quality- of-life assessment in Russia and the United States in chronic peritoneal dialysis patients. Adv Perit Dial 2002; 18: 55-57
- Hinrichsen GA, Lieberman JA, Pollack S, Steinberg H. Depression in hemodialysis patients. Psychosomatics 1989; 30 (3): 284-289
- Yao Q, Qian JQ, Yuan XC. Influence of depression on patients receiving peritoneal dialysis. Chin J Nephrol 2001; 17(2): 123-125
- Kutner NG, Zhang R,Mc Clellan WM. Patient-reported quality of life early in dialysis treatmen:the effects as- sociated with usual exercise activity. Nephrol Nurs J 2000;27 (4): 357-367.