Research Article - Biomedical Research (2017) Volume 28, Issue 16
Local betamethasone injection stabilized the opened-airway diameter in benign central airway stenosis
Yunfeng Chen, Danfeng Xu, Yiming Zeng*, Huaping Zhang, Dongyong Yang and Xiaoyang ChenDepartment of Pulmonary Medicine, the Second Affiliated Hospital of Fujian Medical University, Quanzhou, PR China
- *Corresponding Author:
- Yiming Zeng
Department of Pulmonary Medicine
The Second Affiliated Hospital of Fujian Medical University, PR China
Accepted date: July 31, 2017
Abstract
We assessed the stabilization of an open-airway diameter and locally injected betamethasone for benign central airway stenosis using a prospective study to compare two treatment modalities: Conventional Interventional (CI) and CI combined Local Betamethasone Injected (LBI). The average optical density value for tumor necrosis factor β1 (TGF-β1) was compared in local airway tissues before and 7 d after CI and LBI treatments. Patient prognosis was recorded after one year of treatment. Eight patients were recruited from May 2013 to May 2016 and data show a significant statistical difference in TGF-β1 (94.57 ± 35.77 vs. 155.64 ± 47.38 (t=-7.591, P=0.000) before and after the CI treatment and before and after CI +LBI treatment (145.17 ± 39.38 vs. 84.65 ± 44.34 (t=8.536, P=0.000)). TGF-β1 was measured using ANOVA to compare treatments and there was a statistical difference between the two (F=128.568, P=0.000). Prognoses were effective (6/8, 75%), moderate (1/8, 12.5%), ineffective (1/8, 12.5%) and cured (7/8, 87.5%). Benign central airway therapy should include opening an obstructed airway and stabilizing the airway diameter as well as a local steroid injection to reduce TGF-β1 and minimize the negative effect of CI.
Keywords
Tracheal stenosis, Betamethasone, Bronchoscopes, Transforming growth factor beta l, Collagen.
Introduction
The benign central airway stenosis can cause varying degrees of dyspnea and mostly caused by tuberculosis, tracheal intubation, tracheotomy and trauma [1]. The segmental resection is a classic therapeutic method, but the interventional bronchoscope has become the main treatment method with development of instrumentation and therapy methods in recent years. Bacon et al. [2] recommended that endotracheal intervention included airway dilatation, tissue destruction and stent insertion. But both the literatures [3,4] and the clinical practice experience suggested that the re-stenosis of openedairway frequently occurs. The interventional bronchoscope is also a kind of injury for airway [5,6], and the inevitable process of tissue repair may be one of the re-stenosis reasons after interventional therapy.
Therefore it is the key that how to effectively inhibit the granulation tissue formation and to stabilize the diameter of opened-airway after interventional therapy. Local application of drugs is one of the methods. The drugs currently used to stabilize airway were mitomycin C and glucocorticoid. Some studies suggested that topical application of mitomycin C and glucocorticoid have the effect of improving airway diameter after interventional therapy [7-10]. But these clinical studies were retrospective study and the efficacy was evaluated mainly by observed changes of the diameter of airway and the grade of dyspnea before and after treatment.
It was difficult to carry out a prospective controlled study, the reasons include (1) patients often fail to be observed at a unified point-in-time during the long follow-up period; (2) subjective symptom scores were affected by the patient's tolerance for narrow airway. So we need an index which can evaluate the effect of drugs on the inhibiting the granulation tissue formation in a short time. We detected the difference of tissue tumor necrosis factor β1 (TGF-β1) expression before and after Convention Interventional (CI) or combined Local Betamethasone Injection (LBI) and analyses the clinical data, in order to understand the effect and mechanism of LBI.
Materials and Methods
Conduct of the study
This study was a single-center prospective self-controlled trial, which was conducted in accordance with the declaration of Helsinki, and was approved by the ethics committee of Fujian Medical College (XJS2013135). Written informed consent was obtained from all participants. The study began in May 2013 and ended in May 2016.
Inclusion and exclusion criteria
Inclusion criteria: diagnosed as central airway stenosis by double source Computed Tomography (CT), and additional criteria for enrolment included benign stenosis diagnosed by pathology and required bronchoscopic interventional treatment.
Exclusion criteria: bronchial amyloidosis; bronchogenic tuberculosis with tracheomalacia or positive of tubercle bacillus in sputum; airway malignant or benign tumors, foreign body in bronchus; pregnancy; ≤ 14 y of age; the pathogeny of stenosis unable to remove (like airway stent); does not agree with the trial.
Study design
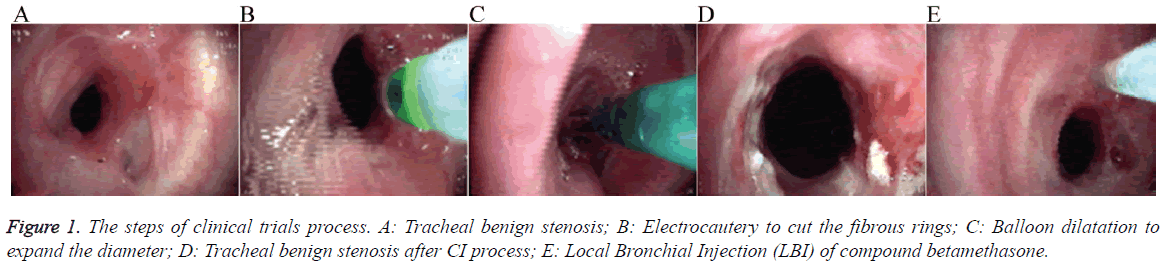
Clinical trials process: (1) CI therapy process: tracheal benign stenosis was shown in Figure 1A, using electrocautery to cut the fibrous rings (Figure 1B), then combined with balloon dilatation to expand the diameter (Figure 1C), at the end used electrocautery treatment to clean up the extrude scar tissue; (2) Figure 1D showed the tracheal benign stenosis after CI process; LBI of compound betamethasone (Schering-Plough Labo N.V., Madison, USA) process: injected compound betamethasone in the opened-airway with sclerosing needle by flexible bronchoscope (Figure 1E). At the lesion 0, 3, 6 and 9 points compound betamethasone was slowly injected 0.5 ml respectively until local swelling or overflow, and total amount was 2 ml; (3) Bronchoscopes process: 1. The first bronchoscopy operation, after enrolled the pathological specimens were obtained at first and then CI process was executed (Figure 1A); 2. The second bronchoscopy operation, 7 d later the pathological specimens were obtained and then repeated CI process, and if the airway diameter was ensured to ventilation then execute LBI, but if the diameter was not enough the bronchoscopy operation would repeated 7 d later; 3. Obtain specimens and assessing effect was conducted after LBI 7 d later.
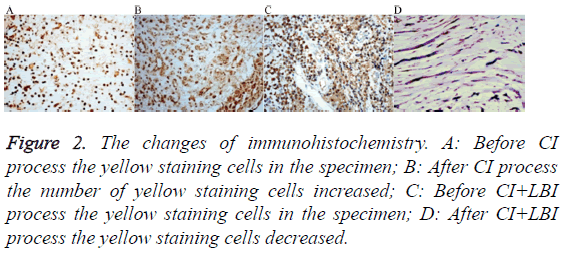
Immunohistochemistry of TGF-β1
Streptavidin-Perosidase (SP) immunohistochemical method was used to detect the TGF-β1, Phosphate Buffered Saline (PBS) substituted for the primary antibody was served as a negative control. In each specimens 1 piece of sections well stained were measured. Five high-fold visual field were chosen at upper left, lower left, upper right, lower right and middle 5 points from each section. The TGF-β1 positive cells were defined as the purple and brown staining in the cytoplasm. The average absorbance value of each field was measured by IPP6.0 graphic analysis software.
Treatment process
After completing the trials process and the airway was fully opened, the patients were discharged and followed up with bronchoscope. The airway diameter and symptoms were assessed every 4-6 w in 6 months and every 3 months in the next 6 months. CI If necessary always combined LBI.
Standard for clinical effect
The judgment standard for clinical effect was refer to previous literature [4]: (1) Effective: After finished trial process the intervention was not applied and free of symptoms during 1 y follow-up; (2) Moderate: Re-stenosis in the first 6 months then intervention was applied less than 3 times, but the re-stenosis had not occurred and free of symptoms for 1 y after the last intervention; (3) Ineffective: 3 or more interventions were required due to recurrent granulation tissue formation within 6 months; (4) Cured: After the last intervention the openedairway kept stable and free of symptoms during 1 y follow-up.
Statistical analysis
SPSS13.0 software was used. Measurement data was described by ͞x ± s and quantitative data by rate. The paired t-test was used to the comparisons of the average optical density value of TGF-β1 before and 7 d after the CI treatment and the LBI treatment, and the variation tendency of 2 treatment methods were tested by repeated measure ANOVA, and a two-sided P<0.05 was considered statistically significant.
Results
Baseline characteristics
Total of 14 patients enrolled, 6 patients were excluded: (1) 1 patient for the tracheal stent obstructing granulation tissue formation and the stent could not be removed, (2) 2 patients for the specimens were fibrous tissue without no cells, (3) 2 patients not followed-up on schedule, (4) 1 patient for the cryotherapy was used to clean up the extrude scar tissue. 8 patients completed the trial were included 4 men and 4 women, the etiology of stenoses were tracheotomy (N=3), endotracheal tube inserted (N=1), tracheobronchial tuberculosis (N=4). The LBI process was executed combined with the second CI (N=6) or the third CI (N=2).
Prognosis
According to the definition, the prognosis were effective (6/8, 75%), moderate (1/8, 12.5%), ineffective (1/8, 12.5%) and cured (7/8, 87.5%). The only ineffective patient 49-year-old male had been underwent tracheotomy and mechanical ventilation before, and suffered 3 CI+LBI processes after clinical trials process and accepted permanent tracheotomy again. All 8 patients hadn't found any adverse effects caused by LBI.
Changes of absorbance of TGF-β1
The changes before and after CI process were the number of cells and the TGF-β1 in the cytoplasm increased and tissue deep dyeing brown (Figures 2A and 2B). But after LBI process all the effect was alleviated (Figures 2C and 2D). The absorbance of TGF-β1 increased from 94.57 ± 35.77 to 155.64 ± 47.38 after CI process. There have statistical differences by paired t-test (t=-7.591, P=0.000). The absorbance of TGF-β1 decreased from 145.17 ± 39.38 to 84.65 ± 44.34 after LBI process. The difference was statistically significant (t=8.536, P=0.000). The trend of TGF-β1 before and after the two treatments had significant statistical differences by repeated measure ANOVA (F=128.568, P=0.000).
Figure 2: The changes of immunohistochemistry. A: Before CI process the yellow staining cells in the specimen; B: After CI process the number of yellow staining cells increased; C: Before CI+LBI process the yellow staining cells in the specimen; D: After CI+LBI process the yellow staining cells decreased.
Discussion
The classic and standard therapeutic method was segmental resection with end-to-end anastomosis, but Amoros et al. [11] reported 54 patients with the overall mortality (1.85%) and postoperative complication (27.5%) which included restenosis (14.2%), granulation tissue (13.1%), edema (10.5%), anastomotic dehiscence (7.1%), and tracheoesophageal fistula (7.1%), furthermore Krajc et al. [12] reported 164 patients with the complication (17.1%) and interventional therapy (4.9%). A lot of patients can't accept the segmental resection for the length of lesion and underlying disease. Therefore, the endotracheal intervention is often preferable. The therapy was comprehensive application of many methods include balloon dilatation, laser, electrocautery, argon plasma coagulation, stents, cryotherapy, endobronchial brachytherapy [2].
Nevertheless Fadaizadeh et al. [6] suggested that electrocautery and argon plasma coagulation caused inflammation and sedimentation of collagen, furthermore the stent is a strong stimulation factor leading to overgrowth of granulation tissue [5], even if the silicone stents can't avoid this effect [13]. The central airway stenosis is a life-threaten disease and the immediate effect of open-airway was got by laser, electrocautery, argon plasma coagulation and stents which we called Conventional Interventional (CI) in this paper. Can these techniques induce granulation tissue formation and cause restenosis in vivo? We found that the absorbance of TGF-β1 increased from 94.57 ± 35.77 to 155.64 ± 47.38 after CI process which illustrated these CI techniques been one of the stimulation restenosis factors. Therefore it is important to find a method to relieve the effect of the airway reinjured and granulation tissue formation by CI thus stabilized the openairway diameter.
There were controversy about the efficiency of local application glucocorticoids [14] and mitomycin [15]. Perepelitsyn and Shapshay [14] suggested no advantage to the use of intralesional steroids as an adjuvant treatment than using the CO2 laser single (success 18.2% vs. 15%) by a retrospective cohort study according to the symptom and restenosis times. But the steroids were 0.4 mg/cc Depo- Medrol. According to our experience and comparing the steroids dosage in our research was too low. The other research found restenosis interphase time increasing from 11 ± 4 d to 99 ± 56 d and the airway diameter and symptoms improved by CI combined triamcinolone injected every 3 w repeat 3 times [8]. We considered that the CI process such as balloon dilatation and electrocautery et al. had dual function (1) Positive effect was dilatating airway diameter; (2) Negative effect delayed effect of granulation tissue formation and restenosis. Which one dominant was influenced by lots of facts like individual difference and strength of CI and intensity of protopathy inflammation and so on. So it is easy to draw contradictory conclusion about the effect of steroids in benign central airway stenosis by clinical observation merely.
The TGF-β1 released from cells in a large latent complex is the crucial factor for adult wound healing, and after acute injury TGF-β1 is rapidly up-regulated and secreted to initiating inflammation and granulation tissue formation [16], furthermore regulate myofibroblast differentiation to contract wounds [17]. On the contrary deregulation of TGF-β target genes would cause non-healing chronic wounds [18]. Karagiannidis et al. found that TGF-β1 was high expressed to enhance the proliferation of fibroblasts from benign tracheal and stent stenoses instead of Ki-67 indicating the proliferating epithelium, and suggested that local drug application must target TGF-β1 [19]. Measuring the variance of TGF-β1 in the lesion can preferably clarification the steroids effect of inhibits granulation tissue formation comparison of simply observing therapeutic effect. We creatively combined TGF- β1 and the clinical data and used CI as control in order to understand the effect and mechanism of LBI.
The mechanisms of steroids inhibiting granulation tissue formation include (1) steroids impact TGF-β signaling [20]; (2) regulation of the TGF-β binding to receptor [21]; (3) the effect is concentration-dependent and high dose steroid (200 ng/ml dexamethasone) can abolish the TGF effect [22]. Recently the steroids intralesional injection was used in keloid scar [23] and a wide spectrum of rheumatic disorders [24] and so on. Compound betamethasone injection has a long effective duration for the long metabolic time of betamethasone dipropionate.
When the CI process combined LBI process we got a good clinic results. During 12 months follow-up the 75% (6/8) patients only needed 2 times CI process and 1 time LBI process, and 12.5% (1/8) patients need CI+LBI one more time and 12.5% (1/8) patient was failure. Although we didn't set a group of patients accepted CI process only as control, from the previous literature the about 30%-50% patients needed repeated CI processes and more invasive therapy [3,4,25]. From mechanism the absorbance of TGF-β1 decreased from 145.17 ± 39.38 to 84.65 ± 44.34. We considered that granulation tissue formation and the influence of CI were inhibited by betamethasone.
Bacon et al. [2] suggested that the options of treating tracheal and bronchial obstruction by bronchoscope included airway dilatation, tissue destruction and stent insertion. But the three options belong to one purpose which is dilating the airway and the strategy of stabilizing the diameter of airway is necessary for the next step. Our opinion is that the strategy of therapy includes two necessary procedures: (1) open the obstructive airway (2) stable the diameter of airway. The steroids local injection is one of the methods for the step 2.
There was still limitation in this research for relatively few patients due to (1) the benign central airway stenosis isn't a common disease, (2) part of patients were excluded for refusing to follow-up on schedule because the painful experience by interventional therapy, (3) the specimen of airway by bronchoscope was small and indeterminateness and non-repeatable, 2 patients were excluded for the unanalyzable specimen. The next study was necessary to investigate the dose and injection frequency of steroid for fare-thee-well.
Conclusion
Our pilot studied from mechanism of granulation tissue formation found that the CI process can induce granulation tissue formation and opened-airway restenosis, and steroid local injection can restrain the generation of TGF-β1 thereby relieving the negative effect of CI process. Furthermore this result could be proven by the good clinical result. Combined this study and pertinent literature [8] we suggest that the strategy of benign central airway therapy should include two necessary procedures (1) Open the obstructive airway (2) Stable the diameter of opened-airway. The steroid local injection is one of the methods for the step 2.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Murgu SD, Egressy K, Laxmanan B, Doblare G, Ortiz-Comino R, Hogarth DK. Central airway obstruction: benign strictures, tracheobronchomalacia, and malignancy-related obstruction. Chest 2016; 150: 426-441.
- Bacon JL, Patterson CM, Madden BP. Indications and interventional options for non-resectable tracheal stenosis. J Thorac Dis 2014; 6: 258-270.
- Gelbard A, Francis DO, Sandulache VC, Simmons JC, Donovan DT, Ongkasuwan J. Causes and consequences of adult laryngotracheal stenosis. Laryngoscope 2015; 125: 1137-1143.
- Rahman NA, Fruchter O, Shitrit D, Fox BD, Kramer MR. Flexible bronchoscopic management of benign tracheal stenosis: long term follow-up of 115 patients. J Cardiothorac Surg 2010; 5: 2.
- Guibert N, Mazieres J, Marquette CH, Rouviere D, Didier A. Integration of interventional bronchoscopy in the management of lung cancer. Eur Respir Rev 2015; 24: 378-391.
- Fadaizadeh L, Hoseini MS, Bagheri M. Anaesthesia management during interventional bronchoscopic procedures: laryngeal mask airway or rigid bronchoscope. Turk J Anaesthesiol Reanim 2014; 42: 302-307.
- Teo F, Anantham D, Feller-Kopman D, Ernst A. Bronchoscopic management of sarcoidosis related bronchial stenosis with adjunctive topical mitomycin C. Ann Thorac Surg 2010; 89: 2005-2007.
- Reichert LK, Zhao AS, Galati LT, Shapshay SM. The efficacy of mitomycin c in the treatment of laryngotracheal stenosis: results and experiences with a difficult disease entity. ORL J Otorhinolaryngol Relat Spec 2015; 77: 351-358.
- Shadmehr MB, Abbasidezfouli A, Farzanegan R, Pejhan S, Daneshvar Kakhaki A, Sheikhy K, Saghebi SR, Sadeghbeigee F, Gharedaghi A, Jahanshahi N, Zangi M. The role of systemic steroids in postintubation tracheal stenosis: a randomized clinical trial. Ann Thorac Surg 2017; 103: 246-253.
- Nouraei SA, Obholzer R, Ind PW, Salama AD, Pusey CD. Results of endoscopic surgery and intralesional steroid therapy for airway compromise due to tracheobronchial Wegeners granulomatosis. Thorax 2008; 63: 49-52.
- Amorós JM, Ramos R, Villalonga R, Morera R, Ferrer G, Díaz P. Tracheal and cricotracheal resection for laryngotracheal stenosis: experience in 54 consecutive cases. Eur J Cardiothorac Surg 2006; 29: 35-39.
- Krajc T, Janik M, Benej R, Lucenic M, Majer I, Demian J, Harustiak S. Urgent segmental resection as the primary strategy in management of benign tracheal stenosis. A single center experience in 164 consecutive cases. Interact Cardiovasc Thorac Surg 2009; 9: 983-989.
- Eom JS, Kim H, Jeon K, Um SW, Koh WJ, Suh GY, Chung MP, Kwon OJ. Tracheal wall thickening is associated with the granulation tissue formation around silicone stents in patients with post-tuberculosis tracheal stenosis. Yonsei Med J 2013; 54: 949-956.
- Perepelitsyn I, Shapshay SM. Endoscopic treatment of laryngeal and tracheal stenosis-has mitomycin C improved the outcome? Otolaryngol Head Neck Surg 2004; 131: 16-20.
- Hartnick CJ, Hartley BE, Lacy PD, Liu J, Bean JA, Willging JP, Myer CM, Cotton RT. Topical mitomycin application after laryngotracheal reconstruction: a randomized, double-blind, placebo-controlled trial. Arch Otolaryngol Head Neck Surg 2001; 127: 1260-1264.
- Ramirez H, Patel SB, Pastar I. The role of TGFi2 signaling in wound epithelialization. Adv Wound Care (New Rochelle) 2014; 3: 482-491.
- Van De Water L, Varney S, Tomasek JJ. Mechanoregulation of the myofibroblast in wound contraction, scarring, and fibrosis: opportunities for new therapeutic intervention. Adv Wound Care (New Rochelle) 2013; 2: 122-141.
- Pastar I, Stojadinovic O, Krzyzanowska A, Barrientos S, Stuelten C, Zimmerman K, Blumenberg M, Brem H, Tomic-Canic M. Attenuation of the transforming growth factor beta-signaling pathway in chronic venous ulcers. Mol Med 2010; 16: 92-101.
- Karagiannidis C, Velehorschi V, Obertrifter B, Macha HN, Linder A, Freitag L. High-level expression of matrix-associated transforming growth factor-beta1 in benign airway stenosis. Chest 2006; 129: 1298-1304.
- Schwartze JT, Becker S, Sakkas E, Wujak LA, Niess G, Usemann J, Reichenberger F, Herold S, Vadász I, Mayer K, Seeger W, Morty RE. Glucocorticoids recruit Tgfbr3 and Smad1 to shift transforming growth factor-β signaling from the Tgfbr1/Smad2/3 axis to the Acvrl1/Smad1 axis in lung fibroblasts. J Biol Chem 2014; 289: 3262-3275.
- Centrella M, McCarthy TL, Canalis E. Glucocorticoid regulation of transforming growth factor-β1 activity and binding in osteoblast-enriched cultures from fetal rat bone. Mol Cell Biol 1991; 11: 4490-4496.
- Zhou H, Sivasankar M, Kraus DH, Sandulache VC, Amin M, Branski RC. Glucocorticoids regulate extracellular matrix metabolism in human vocal fold fibroblasts. Laryngoscope 2011; 121: 1915-1919.
- Trisliana Perdanasari A, Lazzeri D, Su W, Xi W, Zheng Z, Ke L, Min P, Feng S, Zhang YX, Persichetti P. Recent developments in the use of intralesional injections keloid treatment. Arch Plast Surg 2014; 41: 620-629.
- Manchikanti L, Nampiaparampil DE, Manchikanti KN, Falco FJ, Singh V, Benyamin RM, Kaye AD, Sehgal N, Soin A, Simopoulos TT, Bakshi S, Gharibo CG, Gilligan CJ, Hirsch JA. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: A systematic review of randomized controlled trials. Surg Neurol Int 2015; 6: 194-235.
- Nair S, Mohan S, Mandal G, Nilakantan A. Tracheal stenosis: our experience at a tertiary care centre in India with special regard to cause and management. Indian J Otolaryngol Head Neck Surg 2014; 66: 51-56.