Research Article - Current Pediatric Research (2021) Volume 25, Issue 7
Late preterm births and associated neonatal outcomes in a tertiary care center-A prospective observational study.
BS Gamini1, Siddu Charki2*, MM Patil2, Shailaja R Bidri1, Neelamma Patil1, SS Kalyanshettar2, SV Patil2
1Department of Obstetrics & Gynecology, BLDE (DU) Shri BM Patil Medical College Hospital and Research Centre, Vijayapur, India
2Department of Pediatrics, BLDE (DU) Shri BM Patil Medical College Hospital and Research Centre, Vijayapur, India
Corresponding Author:
- Dr. Siddu Charki
Department of Neonatology and Pediatrics
BLDE (DU) Shri BM Patil Medical College Hospital and Research Centre,
Vijayapur India
Tel: +919008002974
E-mail: drsidducharki@gmail.com;sidducharki@bldedu.ac.in
Accepted date: July 20th, 2021
Abstract
Background: Prematurity is one of the leading causes of morbidity and mortality among newborns. The incidence of preterm deliveries especially the late preterm births have unfortunately gone up in the last decade. Late preterm births are associated with increased neonatal complications compared to term births. This study makes an effort to find out the relevant maternal and fetal factors associated with late preterm births. This study also assesses the maternal and neonatal outcomes associated with late preterm births. Methods: This prospective observational study was conducted at Maternal and Child Health Unit of Shri B M Patil Medical College Hospital Vijayapur, Karnataka over a period of 1 year. 200 late preterm births and 200 term births were enrolled in the study. During the study period, all neonates delivered in the hospital were divided into two groups as late preterm group and term group. Maternal and neonatal data was collected in predefined structured proforma. Results: The mother's mean age in the late preterm group was 24.34 ± 4.07 years, and among the term group was 25.24 ± 4.54 years, which was not statistically significant (P=0.857). The obstetric risk factors observed for late preterm births were inadequate antenatal care (39%), premature rupture of membranes (31%), hypertensive disease of pregnancy (24.5%), previous preterm delivery (21%), and maternal anemia (13%). When two or more factors were found, late preterm labor incidence was 32.6% in this study. 14.5% late preterm's needed resuscitation (P=0.003), 45% late preterm neonates had difficulty establishing feeding at birth (P<0.001), 34% late preterm’s had respiratory distress at birth (P<0.001), 12% had hypoxic-ischemic encephalopathy (Stage2/3) (0.003), 35% had early-onset sepsis (P<0.001), 28% had jaundice (P<0.001), 24% had hypoglycemia (P<0.001), 41% had hypothermia (P<0.001), 13.5% had HSPDA (P<0.006). The duration of hospital stay was significantly more in late preterm neonates (8.7 ± 1.6 days) as compared to term neonates (3.9 ± 1.1 days) with a pvalue of <0.05. Most important is the mortality, which was significantly more among late preterm neonates (18%) than term neonates (6%) with a p-value of 0.011. Conclusion: Maternal risk factors such as preterm premature rupture of membrane, inadequate antenatal care, hypertensive disorders of pregnancy, and maternal anemia were associated with late preterm births. Since late preterm birth is an independent risk factor for neonatal morbidity and mortality compared to term neonates, knowing maternal and perinatal risk factors is essential. Early identification and management of these risk factors reduces the neonatal morbidities and mortalities.
Keywords
Antenatal care, Hypertensive disorder of pregnancy, Preterm premature rupture of membrane.
Introduction
Prematurity is one of the leading causes of morbidity and mortality among newborns, occurring in more than one in ten live births. Late preterm neonates are born between 34 and 36, 6/7 weeks of gestation and they constitute around 70% of all preterm deliveries in 2009 which has further increased over a decade [1]. The majority of late preterm births are due to spontaneous preterm labor, preterm premature rupture of the membrane, and deliveries due to feto-maternal indications. Other obstetric conditions include maternal urinary tract infection, hypertensive disease of pregnancy, gestational diabetes, and multiple pregnancies. In utero growth restriction and the non-reassuring fetal status represent the main fetal factors [2-5]. Recommendations for antenatal steroids administration for fetal lung maturity in terms of gestational age and tocolysis are not well established. Still, most practitioners do not advocate the use of antenatal corticosteroids or tocolysis after 34 completed weeks of gestation.
Neonates born beyond 34 weeks are fallaciously termed as 'near term,' and adverse perinatal outcomes in these neonates are undoubtedly enhanced. The risk of neonatal outcomes is inversely proportional to gestational age. The frequency and severity of neonatal complications are reduced in all fetuses with increase in duration of fetus in utero. Late preterm neonates are at increased risk for complications in comparison to term neonates, such as respiratory complications like Respiratory Distress Syndrome (RDS), Persistent Pulmonary Hypertension (PPHN), Transient Tachypnea of the Newborn (TTN), Metabolic complications like hypoglycemia, and hypocalcemia, temperature instability, neonatal hyperbilirubinemia, feeding difficulties including Necrotizing Entero Colitis(NEC) and prolonged Neonatal Intensive Care Unit (NICU) stay [6,7].
Long-term studies indicate that, compared to term infants, late preterm neonates are at an augmented risk for adverse neurodevelopment outcomes and learning disabilities, with a neurocognitive impairment that may persist into adulthood [8- 12]. Awareness of the factors that lead to late preterm births can provide healthcare professionals with the knowledge to prevent late preterm births, reducing neonatal morbidity and mortality. Thus, this study aimed to determine maternal and fetal risk factors associated with the late preterm births compared to a term and study the morbidity and mortality pattern of late preterm neonates compared to term neonates.
Methods
This prospective observational cohort study was conducted at Maternal and Child Health Unit of Shri BM Patil Medical College Hospital and Research Center, BLDE (DU), Vijayapura, Karnataka, India, from October 2019 to September 2020. Late Preterm neonates born between 34; 0/7 and 36; 6/7 weeks of gestation were compared with the equal number of term neonates (37; 0/7 to 41; 6/7 weeks gestation). Consent was obtained from the mothers and parents of all neonates included in the study, and the institutional ethics committee approved the study.
Inclusion criteria
Neonates with gestation age of 34; 0/7 and 36; 6/7 weeks and neonates with the gestational age of 37; 0/7 to 41; 6/7 weeks gestation.
Exclusion criteria
Neonates wherein the gestational age could not be ascertained either by ultrasound or by New Ballard score and neonates with major congenital malformations and chromosomal anomalies were excluded.
Sample size
Was calculated using the formula n=z2pq/d2, where z=1.96, p=prevalence of late preterm infants in this hospital as per the previous records, q=(1-p), d=95% confidence interval. The sample size as calculated by the above formula was 187. Hence a total of 200 late preterms and 200 term neonates were included in the study group from October 2019 to September 2020.
During the study period, all neonates delivered in the hospital were subjected to gestation assessment by early obstetric ultrasound (6-12 weeks) or by new Ballard score. The enrolled babies were divided into two groups as follows. Late Preterm Neonates: Gestational age 34; 0/7 to 36; 6/7 weeks. Term Neonates: Gestational age 37; 0/7 to 41; 6/7 weeks.
Data was collected in predefined structured proforma regarding the following maternal and fetal aspects: Maternal age, parity, H/o abortion, h/o pretermdelivery in a previous pregnancy, hypertensive disorders of pregnancy, maternal anemia, PPROM, multiple pregnancies, post caesarean pregnancy, gestational diabetes mellitus, maternal infections, artificial reproductive techniques, malpresentation, uterine anomalies, mode of delivery; apgar score and NICU admissions.
Data were collected regarding the following neonatal aspects: 1) Gestation; (2) Sex; (3) Birth weight; (4) Need for resuscitation at birth and APGAR scoring; (5) In case of NICU admission, the following details were documented: Respiratory distress, metabolic disturbances like hypoglycemia, feeding difficulties, nec, neonatal jaundice, sepsis, hypothermia, need for mechanical ventilation, need for inotropes, hemodynamically significant patent ductusarteriosus, intraventricular hemorrhage, congenital anomalies, duration of NICU stay and mortality.
Statistical analysis
The statistical methods (descriptive studies, chi-square/ contingency coefficient analysis, and independent samples ttest) were carried out through the SPSS for Windows (version 23.0). The p-value <0.05 was taken as statistically significant.
Results
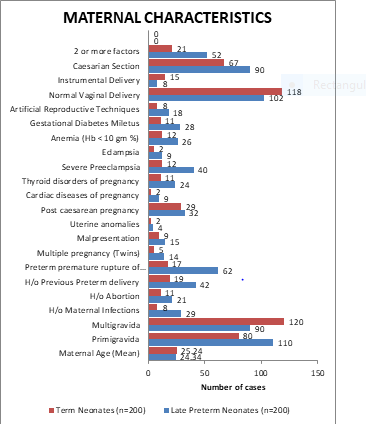
In the present study, 200 late preterm neonates were compared with 200 term neonates. The mother's mean age in the late preterm group was 24.34 ± 4.07 years, and among the term group was 25.24 ± 4.54 years, which was not statistically significant. There were 65 neonates between 34 to 35 weeks gestation, 63 neonates between 35/1 to 36 weeks gestation, and 72 neonates between 36/1 to 37 weeks gestation. The obstetric risk factors observed for late preterm delivery were premature rupture of membranes (31%), pregnancy-induced hypertension (20%), eclampsia (4.5%), previous preterm delivery (21%), maternal anemia (13%), multiple pregnancies (7%), maternal infections (14.5%), gestational diabetes mellitus (14%), history of one or more abortions (10.5%), malpresentation (7.5%), post cesarean pregnancy (16%), cardiac diseases of pregnancy (4.5%), thyroid disorders of pregnancy (12%), and uterine malformations (2%). An artificial reproductive technique was observed in 9% of late preterm deliveries compared to 4% in term deliveries. When two or more factors were found, late preterm labor incidence was 32.6% in this study. Primipara and multiparas had similar late preterm delivery rates compared to term delivery, whereas more multiparas had term deliveries (Table1 and Figure 1).
| Maternal characteristics | Late preterm births (n=200) | Term births (n=200) | P value |
|---|---|---|---|
| Maternal age (mean ± sd) | 24.34 ± 4.07 | 25.24 ± 4.54 | 0.857 |
| Parity | |||
| Primigravida | 110 | 80 | 0.002* |
| Multigravida | 90 | 120 | 0.003* |
| Inadequate antenatal care | 78 | 24 | <0.001* |
| H/o Maternal Infections | 29 | 8 | <0.001* |
| H/o Abortion(1 or more) | 21 | 11 | 0.065 |
| H/o Previous preterm delivery | 42 | 19 | 0.002* |
| Premature Rupture of Membranes (PROM) | 62 | 17 | <0.001* |
| Multiple pregnancy (Twins) | 14 | 5 | 0.030* |
| Malpresentation | 15 | 9 | 0.207 |
| Uterine anomalies | 4 | 2 | 0.794 |
| Post caesarean pregnancy | 32 | 29 | 0.677 |
| Cardiac diseases of pregnancy | 9 | 2 | 0.032* |
| Thyroid disorders of pregnancy | 24 | 11 | 0.021* |
| Hypertensive disorders of pregnancy | |||
| Severe preeclampsia | 40 | 12 | <0.001* |
| Eclampsia | 9 | 2 | 0.032* |
| Anemia (Hb<10 gm %) | 26 | 12 | 0.017* |
| Gestational diabetes miletus | 28 | 11 | 0.004* |
| Artificial reproductive techniques | 18 | 8 | 0.043* |
| Mode of delivery | |||
| Normal vaginal delivery | 102 | 118 | 0.108 |
| Instrumental delivery | 8 | 15 | 0.133 |
| Caesarian section | 90 | 67 | 0.019* |
| 2 or more factors | 52 | 21 | <0.001* |
Table 1. Maternal characteristics among late preterm births and term births.
Among the study group, 102 neonates were delivered by vaginal delivery, 08 cases by operative instrumental delivery, and 90 by cesarean section. Among the late preterm neonates, 149 neonates were appropriate for gestational age, 46 neonates were small for gestational age, and 05 neonates were large for gestational age. Among the late preterm neonates, 58 neonates were <1.5 kg, 93 neonates were 1.5 kg-2.5 kg and 49 neonates were >2.5 kg.
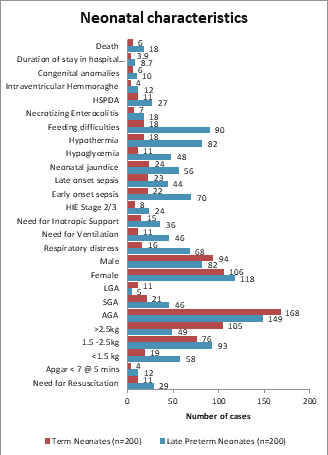
29 late preterm's needed resuscitation at birth compared to 11 term neonates, which was statistically significant. Of the 29 neonates who required resuscitation, 13 late preterm’s required endotracheal intubation compared to 7 term neonates, which was statistically significant (p=0.04). APGAR score was <7 at 5 mins in 12 late preterm’s than four-term neonates, which was statistically significant (p<0.05). About 90 late preterm neonates had difficulty establishing feeding at birth.
They needed assistance for setting feeding in the form of help by a counselor, or pallada feeds, or nasogastric tube feeding compared to only 18 term neonates was statistically significant (<0.001). Sixty-eight late preterm’s had respiratory distress at birth with a SAS Score of 2-3/10 compared to 16 of term neonates, which was statistically significant (<0.001). Forty-six late preterm neonates required ventilation support, either noninvasive or invasive, compared to 11 term neonates, which was statistically significant (<0.001). The need for Inotropic support was high in the late preterm group (36 cases) as compared to 15 term neonates, which was statistically significant (<0.001). 24 late preterm neonates had hypoxicischemic encephalopathy (Stage 2/3) compared to 8 term neonates, which was statistically significant (0.003).
Early-onset sepsis (probable sepsis and culture-positive sepsis) was more common amongst late preterm neonates (70) as compared to 22 term neonates, which was statistically significant(<0.001). About 56 late preterm neonates had jaundice significant enough to require intervention in the form of phototherapy as against 24 term neonates, which was statistically significant (<0.001). Forty-eight late preterm neonates had hypoglycemia significant enough to require intervention against 11 term neonates, which was statistically significant (<0.001). The incidence of hypothermia was prevalent among late preterm neonates (82) as compared to term neonates (18), which were statistically significant. The frequency of HSPDA was more in the late preterm group (27) than 11 term neonates requiring PDA closure treatment, which was statistically significant (0.006). Necrotizing enterocolitis rates were more common in the late preterm group (18) as compared to the term group (7), statistically significant (0.023). IVH was more in the late preterm group (12 cases) compared to 4 term neonates, which was statistically significant (0.04). The duration of hospital stay was significantly more in late preterm neonates (8.7 ± 1.6 days) as compared to term neonates (3.9 ± 1.1 days) with a p-value of <0.05. Most important is the mortality, which was significantly more among late preterm neonates (18%) than term neonates (6%) with a p-value of 0.011 (Table 2 and Figure 2).
| Neonatal characteristics | Late preterm births (n=200) | Term births (n=200) | P value |
|---|---|---|---|
| Need for resuscitation | 29 | 11 | 0.003* |
| Apgar <7@5 mins | 12 | 4 | 0.041* |
| Birth weight | |||
| <1.5 kg | 58 | 19 | <0.001* |
| 1.5 kg-2.5kg | 93 | 76 | 0.085 |
| >2.5 kg | 49 | 105 | <0.001* |
| Gestational age | |||
| AGA | 149 | 168 | <0.001* |
| SGA | 46 | 21 | 0.999 |
| LGA | 5 | 11 | 0.126 |
| Gender | |||
| Female | 118 | 106 | 0.227 |
| Male | 82 | 94 | 0.227 |
| Respiratory distress | 68 | 16 | <0.001* |
| Need for ventilation | 46 | 11 | <0.001* |
| Need for Inotropic Support | 36 | 15 | <0.001* |
| HIE Stage 2/3 | 24 | 8 | 0.003* |
| Early onset sepsis | 70 | 22 | <0.001* |
| Late onset sepsis | 44 | 23 | 0.005* |
| Neonatal jaundice | 56 | 24 | <0.001* |
| Hypoglycemia | 48 | 11 | <0.001* |
| Hypothermia | 82 | 18 | <0.001* |
| Feeding difficulties | 90 | 18 | <0.001* |
| Necrotizing enterocolitis | 18 | 7 | 0.023* |
| HSPDA | 27 | 11 | 0.006* |
| Intraventricular hemmoraghe | 12 | 4 | 0.041* |
| Congenital anomalies | 10 | 6 | 0.307 |
| Duration of stay in hospital (days) (Mean ± SD) | 8.7 ± 1.6 | 3.9 ± 1.1 | 0.041* |
| Death | 18 | 6 | 0.011* |
Table 2. Neonatal characteristics among late preterm births and term births.
Discussion
The present study assessed the risk factors associated with late prematurity, identifying many determinants that need to be recognized early to prevent it. Young and advanced maternal age is a known risk factor for preterm labor. Carter et al. quoted that age <17 and >35 is associated with increased risk of late preterm birth [13]. In our study, the mother's mean age in the late preterm group was 24.34 ± 4.07 years, and the term group was 25.24 ± 4.54 years, which was not statistically significant.
Increased prevalence of late preterm birth in nulliparous mothers was observed by Melamed et al. in, whereas primipara and multiparas had similar rates of late preterm delivery compared to term delivery in our study [14]. Multiparas had an increased rate of term deliveries compared to preterm deliveries, which is comparable to the data quoted by Mandruzzato et al. Association of previous abortion (1 or more) whether induced or spontaneous with late preterm birth is uncertain [15]. Throp et al. quoted an increased risk of preterm birth among women who previously had abortion [16]. 42% of women had late preterm birth with a history of previous abortion, which was not statistically significant in this study.
Laughon et al. reported that spontaneous labor, preterm premature rupture of membranes, and indicated deliveries accounted for about 30% of late preterm births.3 Late preterm births are secondary to various factors, mainly; maternal medical and obstetric complications, significant congenital anomalies, isolated spontaneous deliveries, and no recorded indications as documented by Reddy et al. [17]. Lubow et al. stated that spontaneous labor and rupture of membranes were the most common (92%) indications for late preterm delivery [18]. In our study, spontaneous late preterm labor was observed in 59% patients and 41% of patients were induced labor for various maternal and fetal factors such as preeclampsia, PPROM. Increased frequency of obstetric interventions resulting from maternal complications or pre-existing medical conditions attribute increased incidence of late preterm birth [19].
Several maternal medical conditions, such as diabetes, hypertensive disorders of pregnancy, and asthma, are associated with an increased risk for preterm birth. The decision to deliver a neonate preterm is taken by balancing the maternal and fetal consequences of continuing the pregnancy against the morbidity and mortality risks associated with prematurity [20].
Laughon, in their study observed a significant association between the occurrence of maternal comorbidities and the increased risk of prematurity. The main comorbidities were maternal hypertensive disease and diabetes [3,5]. In the present study, there was a statistically significant association between premature birth and maternal medical conditions like hypertensive disease of pregnancy (p=0.001) or diabetes (p=0.004) in the late preterm births. We observed that increase frequency of late preterm birth was associated with preterm premature rupture of membrane (31%), hypertensive disorder of pregnancy (20%), maternal anemia (13%), and eclampsia (4.5%), cardiac diseases of pregnancy (4.5%), gestational diabetes mellitus (14%), thyroid disorders of pregnancy (12%) and artificial reproductive techniques (9%) in this study.
Nadin et al. quoted women who did not receive adequate antenatal care were almost four times at higher risk of premature birth. Brown et al. stated that prematurity is associated with inadequate antenatal care [21,22]. The present study, observed that inadequate antenatal care was a forecaster of late prematurity with statistically significant p value (p=0.001), similar to Machado et al. [23].As described by Machado et al, in the present study, pregnant women with inadequate antenatal care were raised in the late preterm group (39%), far above the term group (18.6%) [23].
According to the Leal et al. study, urinary tract infection is the most common maternal infection present during pregnancy related to preterm labor and prematurity [24]. A statistically significant association between preterm birth and maternal infections was observed in this study (p ≤ 0.001). Laughon et al. stated spontaneous preterm birth, including preterm labor and PROM, resulted in two-thirds of all late preterm births [3]. Hypertensive disease of pregnancy, and diabetes represented the other third. This study reported 31% PROM cases resulting in late premature births, comparable to the Hackenhaar et al. study [25].
Nadin et al. stated that early maternal hospitalization during pregnancy indicates the occurrence of maternal or fetal health problems, which may either result in premature birth or cesarean section [22]. When maternal or obstetric complications occur, the delivery method's risks and benefits can be considered with expectant management on a daily basis for maternal and neonatal health to determine the best delivery time. An increased frequency was observed in the present study in pregnant women with late preterm births requiring hospitalization for more than 24 hours until delivery, probably because there was an effort made to postpone premature birth by arresting spontaneous labor.
Cesarean sections are an effective life-saving intervention for mothers and babies, but only when appropriately indicated for medical reasons as stated by World Health Organization. The observations of the present study, state that the cesarean section rate was 45% in the late preterm group and 33.5% in the term group. Among all the cesarean section cases, 13% of patients underwent repeat cesarean, and 8% had successful labor trials after cesarean section. This data is similar to study by Guimaraes et al. which quoted that Brazil has a high prevalence of cesarean births (52.8%), with 38.1% being performed in public hospitals [26]. The studied hospital is a tertiary care center for high-risk pregnancies in North Karnataka, India, where the most complex cases are managed and hence the likelihood of requiring a cesarean section is high. Lisonkova et al. showed that in centers with increased prematurity rates, neonatal death rates were lower [27]. Late preterm births that occur for medical reasons are advantageous as they were performed on those at risk of mortality.
In this study, 29% newborn had weight less than 1.5 Kg, 46.5% newborn weighed 1.5-2.5 Kg and 24.5% newborn weighed >2.5 kg. 6% of the newborn had Apgar 7 or less, and 13% of newborns required NICU admission for various neonatal problems. Raju et al. and Hunt reported that neonatal morbidities are seven times higher than in late preterm births [28,29]. McIntire et al. have stated that Respiratory Distress Syndrome (RDS), Persistent Pulmonary Hypertension of Newborns (PPHNs), neonatal jaundice, Intraventricular Hemorrhage (IVH), neonatal culture positive sepsis, hypothermia, hypoglycemia, and feeding difficulties was observed more often in late preterm neonates [30,31]. In the present study, 34% of neonates presented with respiratory distress, among which 23% neonates required ventilation support, 12% neonates had features suggestive of HIE 2/3, 18% neonates required Inotropic support, 35% neonates had early-onset sepsis, whereas 22% had late-onset sepsis, 13.5% had HSPDA, 28% had hyperbilirubinemia, 24% had hypoglycemia, 9% had NEC, 6% had Intraventricular Hemorrhage (IVH), 41% had temperature instability, 45% had feeding difficulties, and 5 % had Congenital anomalies similar to study done by Verklan [31].
Conclusion
Higher incidences of preterm premature rupture of membrane, inadequate antenatal care, hypertensive disorders of pregnancy, and maternal anemia were associated with late preterm births, resulting in 21% of newborns requiring NICU admission. The increased association of late preterm births with inadequate antenatal checkup, suggests the need to establish robust health policies to enhance the antenatal visits thereby reducing unfavorable outcomes. This study contributes by identifying maternal and perinatal risk factors associated with late preterm births in formulating health care policies. Since late preterm birth is an independent risk factor for neonatal morbidity and mortality compared to term neonates, knowing maternal and perinatal risk factors is essential. Early identification and management of these risk factors reduces the neonatal morbidities and mortalities.
References
- Bick D. Born too soon: The global issue of preterm birth. Midwifery. 2012; 28(4): 401-2.
- McIntire DD, Leveno KJ. Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol 2008; 111(1):35-41.
- Laughon SK, Reddy UM, Sun L, et al. Precursors for late preterm birth in singleton gestations. Obstet Gynecol 2010; 116(5):1047-55.
- Bouchet N, Gayet-Ageron A, Areta ML, et al. Avoiding late preterm deliveries to reduce neonatal complications: An 11-year cohort study. BMC Pregnancy Childbirth2018; 18(1):17.
- Araújo BF, Zatti H, Madi JM, et al. Analysis of neonatal morbidity and mortality in late- preterm newborn infants. J Pediatr (Rio J) 2012; 88(3):259-66.
- Leone A, Ersfeld P, Adams M, et al. Neonatal morbidity in singleton late preterm infants compared with full-term infants. Acta Pediatr 2012; 101(1):e6-10.
- Natarajan G, Shankaran S. Short- and long-term outcomes of moderate and late preterm infants. Am J Perinatol 2016; 33(3):305-17.
- McLaurin KK, Hall CB, Jackson EA, et al. Persistence of morbidity and cost differences between late-preterm and term infants during the first year of life. Pediatrics 2009; 123(2):653-9.
- McGowan JE, Alderdice FA, Holmes VA, Johnston L. Early childhood development of late-preterm infants: A systematic review. Pediatrics 2011; 127(6):1111-24.
- Teune MJ, Bakhuizen S, Bannerman CG, et al. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol 2011; 205(4):374.e1-9.
- Heinonen K, Eriksson JG, Lahti J, et al. Late preterm birth and neurocognitive performance in late adulthood: A birth cohort study. Pediatrics 2015; 135(4):e818-25.
- Costa BC, Vecchi AA, Granzotto JA, et al. Comparative analysis of complications of late preterm infants vs. term infants. Bol Cient Pediatr 2015; 04:33-7.
- Carter MF, Fowler S, Holden A, et al. The late preterm birth rate and its association with comorbidities in a population-based study. Am J Perinatol 2011; 28(9):703-7.
- Melamed N, Klinger G, Tenenbaum-Gavish K, et al. Short-term neonatal outcome in low-risk, spontaneous, singleton, late preterm deliveries. Obstet Gynecol 2009; 114(2pt1):253-60.
- Mandruzzato GP, Calì G, Chiaffarino F, et al. Risk factors for late preterm births: A Case-control study. Gynecol Obstet. 2013; 3(6):1-5.
- Thorp JM, Hartmann KE, Shadigian E. Long-term physical and psychological health consequences of induced abortion: Review of the evidence. ObstetGynecolSurv 2003; 58(1):67-79.
- Reddy UM, Ko CW, Raju TN, et al. Delivery indications late-preterm gestations and infant mortality rates in the United States. Pediatrics 2009; 124(1):234-40.
- Lubow JM, How HY, Habli M, et al. Indications for delivery and short-term neonatal outcomes in late preterm as compared with term births. Am J ObstetGynecol 2009; 200(5):e30-3.
- Villar J, Abalos E, Carroli G, et al. Heterogeneity of perinatal outcomes in the preterm delivery syndrome. ObstetGynecol 2004; 104(1):78-87.
- Behrman RE. Institute of Medicine, Committee on understanding premature birth and assuring healthy outcomes, board on health sciences policy,Preterm birth: Causes, consequences, and prevention. Washington, DC: National Academies Press; 2007.
- Brown HK, Speechley KN, Macnab J, et al. Biological determinants of spontaneous late preterm and early term birth: a retrospective cohort study. BJOG 2015; 122(4):491-9.
- Abdel Razeq NM, Khader YS, Batieha AM. The incidence, risk factors, and mortality of preterm neonates: A prospective study from Jordan. Turk J ObstetGynecol 2017; 14(1):28-36.
- Machado AK, Marmitt LP, Cesar JA. Late preterm birth in the far south of Brazil: a population-based study. Rev Bras SaudeMatern Infant 2016; 16(2):121-8.
- Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, et al. Prevalence and risk factors related to preterm birth in Brazil. Reprod Health 2016; 13(Suppl 3):127.
- Hackenhaar AA, Albernaz EP, Fonseca TM. Preterm premature rupture of the fetal membranes: association with sociodemographic factors and maternal genitourinary infections. J Pediatr (Rio J) 2014; 90(2):197-202.
- Guimarães RM, Silva RL, Dutra VG, et al. Factors associated to the type of childbirth in public and private hospitals in Brazil. Rev Bras Saude Mater Infant. 2017; 17(3):581-90.
- Lisonkova S, Sabr Y, Butler B, et al. International comparisons of preterm birth: Higher rates of late preterm birth are associated with lower rates of stillbirth and neonatal death. BJOG 2012; 119(3):1630-9.
- Raju TN, Higgins RD, Stark AR, et al. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of child health and Human Development. Pediatrics 2006; 118(3):1207-14.
- Hunt CE. Ontogeny of autonomic regulation in late preterm infants born at 34-37 weeks postmenstrual age. Semin Perinatol 2006; 30(2):73-6.
- McIntire DD, Leveno KJ. Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynecol 2008; 111(1):35-41.
- Verklan MT. So, he's a little premature...what's the big deal? Crit Care Nurs Clin North Am 2009; 21(2):149-61.